INTRODUCTION
On March 11, 2020, the World Health Organization declared the coronavirus disease 2019 (COVID-19) a pandemic. At the time, there were more than 110,000 confirmed cases and 4,000 deaths in 113 countries, including Korea.
1 In Korea, the first COVID-19 patient was confirmed on January 20, 2020, and the infection quickly spread nationwide. The first wave of COVID-19 in Korea occurred throughout February and March 2020, and the second wave occurred in August 2020. On December 25, 2020, during the third wave, a record-high of 1,241 new cases were confirmed. To reduce the spread of COVID-19, the Korea Disease Control and Prevention Agency focused on and implemented precautionary measures such as the mandatory use of face masks in public places, extensive COVID-19 screening tests, social distancing, and self-quarantine. However, the incidence of COVID-19 continued to rise and fall, and as of March 1, 2021, the daily number of new confirmed cases was around 300.
234
Several studies published on previous epidemics (e.g., SARS, Ebola) have reported that a massive outbreak of an infectious disease increases depression and anxiety among public, highlighting the importance of psychiatric assessment and early intervention during an epidemic to decrease the risk of various mental disorders.
567 COVID-19 is anticipated to have a greater impact on the mental health of the general public than the previously mentioned epidemics.
Amid the prolonged COVID-19 pandemic in Korea, the Korean people are nervous about the potential onset of a fourth wave of COVID-19 in the country. With continued enforcement of prevention measures, people are instructed to avoid outdoor activities and, thus, are restricted to their homes in their leisure time. The pandemic brought an economic slump; many people lost their jobs or are suffering from financial difficulties. In response, the government issued payments to support the people. Moreover, the number of people undergoing self-quarantine as a result of being in close contact with a confirmed patient is increasing, and the practice of social distancing calls for various changes in interpersonal relationships. Taken together, we suspect that the prolonged COVID-19 pandemic will trigger more serious mental health problems.
However, to the best of our knowledge, the levels of depression and anxiety and their predictors among the Korean general public during the COVID-19 pandemic have not been studied. Thus, this study examines the level of depression and anxiety and their predictors among the general public in Busan, Korea.
Go to :

METHODS
Study design and participants
This was a cross-sectional study. A self-reported questionnaire was administered anonymously using an online platform to 2,288 adult residents of Busan, Korea, to examine the impacts of COVID-19 on them. Study data were collected for 18 days, from August 14 to August 31, 2020. During this time, the number of confirmed cases in Korea had increased from 14,000 to 19,000, and as of August 14, the incidence of COVID-19 in Busan was 5.8 per 100,000 population.
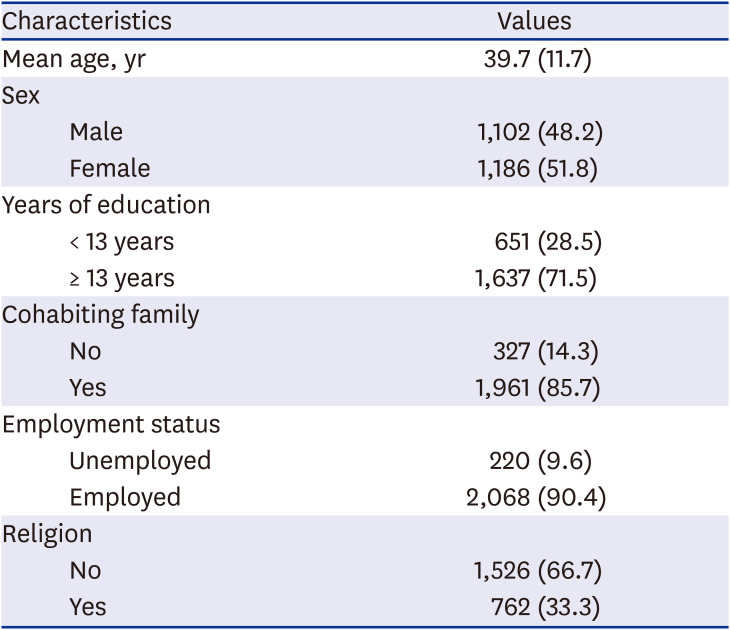
89 The participants of the questionnaire were sampled via quota sampling by sex, age, and region from Busan residents aged 19–60 years, and each person was allowed to submit the questionnaire only once. The questionnaire specified that confidentiality and anonymity will be ensured for all collected information and that the information will only be used for research purposes.
Questionnaire
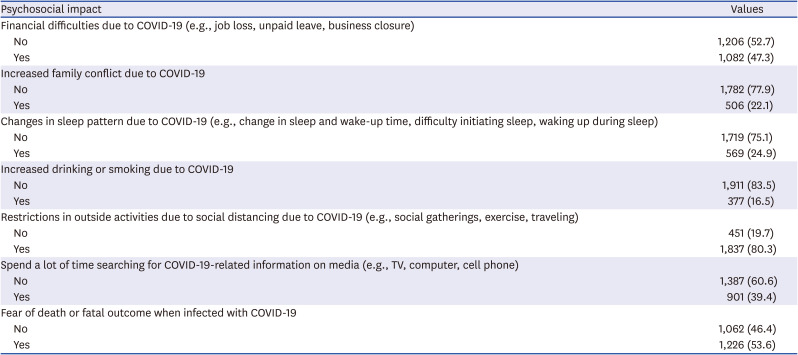
The questionnaire was administered through an online platform. The participants were asked their sex, age, and education level and instructed to answer yes or no to the questions about family living together, employment status, and religion. To collect information about the impact of COVID-19 on their daily lives, the participants were asked to answer yes or no to the questions asking about “financial difficulties as a result of COVID-19,” “increased family conflict due to COVID-19,” “changes in sleep pattern due to COVID-19,” “increased drinking or smoking due to COVID-19,” “restrictions in outside activities due to social distancing practices due to COVID-19,” “spending a lot of time searching for COVID-19-related information on media,” and “fear of death or fatal outcome when infected with COVID-19.”
Participants' depression and anxiety were assessed using the standardized Korean version of the PHQ-4, which was developed, adapted, and published in a previous study with proving its acceptable validity and reliability.
10 The PHQ-4 is a self-report questionnaire consisting of the PHQ-2 and GAD-2, which are the shortened versions containing the first 2 items of the PHQ-9 developed to screen depressive disorders and GAD-7 developed to screen anxiety disorders, respectively. The PHQ-2 and GAD-2 consist of simple questions appropriate for large-scale epidemiological studies; they have also been validated in a population-based study.
1112 The PHQ-2 and GAD-2 use a 4-point scale from 0 to 3 for each item, so the total scores can range from 0 to 6. A total score of 3 or higher is used as the cutoff to determine depressive or anxiety disorders for a quick screening.
1314 According to previous studies, the PHQ-2 predicted a major depressive disorder with 83% sensitivity and 90% specificity when the cutoff was set to 3 or higher; while the GAD-2 predicted a generalized anxiety disorder with 86% sensitivity and 83% specificity, panic disorder with 76% sensitivity and 81% specificity, and social anxiety disorder with 70% sensitivity and 81% specificity when the cutoff was set to 3 or higher.
1516 Therefore, we also set the cutoff values of PHQ-2 and GAD-2 to 3 or higher. In other words, a PHQ-2 score of 3 or higher indicates “depression” and a score of below 3 indicates “no depression,” and a GAD-2 score of 3 or higher indicates “anxiety” and a score of below 3 indicates “no anxiety.” In our study, the PHQ-4 showed satisfactory reliability (Cronbach's α = 0.87).
Statistical analysis
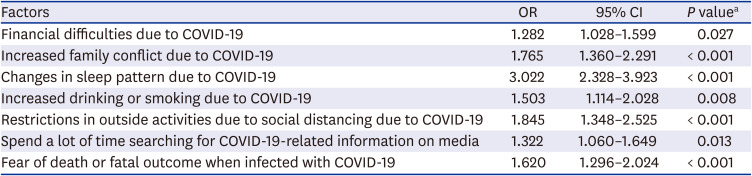
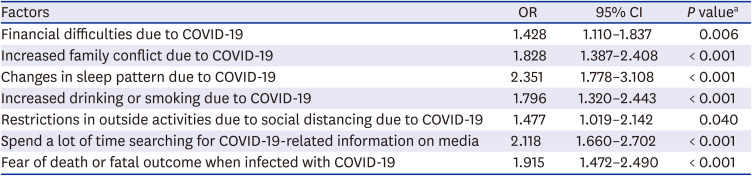
The participants' sociodemographic data were presented using descriptive statistics, namely, mean and standard deviation, or N and percentage. The correlation between depression and anxiety and the impact of COVID-19 was analyzed using logistic regression. In the logistic regression, the yes or no responses to “increased family conflict due to COVID-19,” “changes in sleep pattern due to COVID-19,” “increased drinking or smoking due to COVID-19,” “restrictions in outside activities due to social distancing practices due to COVID-19,” “spending a lot of time searching for COVID-19-related information on media,” and “fear of death or fatal outcome when infected with COVID-19” were entered as the independent variables. The dependent variables were set to “depression” and “anxiety” based on the cutoffs of PHQ-2 and GAD-2; and age, sex, education level, family living together, employment status, and religion status were set as covariates. The results of logistic regression were presented as odds ratios (ORs) and 95% confidence intervals (CIs), and a P value < 0.05 was considered statistically significant. The SPSS statistical software package (version 22.0; IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
Ethics statement
This study was approved by the Institutional Review Board of Dong-A University Hospital (DAUHIRB-20-104). Informed consent was submitted by all subjects when they were enrolled.
Go to :

DISCUSSION
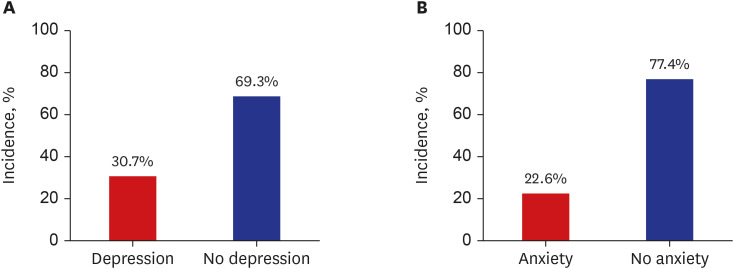
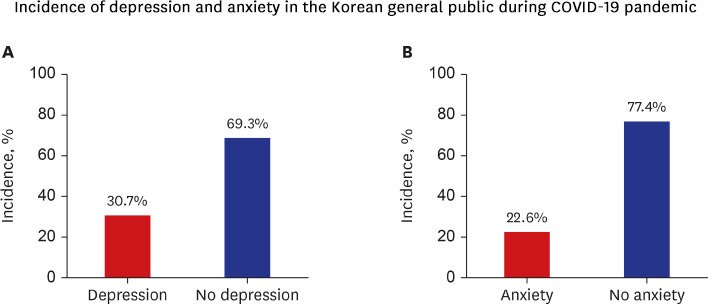
Primarily, this study aimed to examine the current levels of depression and anxiety among the general public in Busan, Korea, during the COVID-19 pandemic. Among our participants, 30.7% had a PHQ-2 score of 3 or higher, indicating depression, and 22.6% had a GAD-2 score of 3 or higher, indicating anxiety. Most previous studies set a PHQ-2 or GAD-2 score of 3 or higher as the cutoff score and considered it as a “yellow flag” warranting screening; thus, the result that 30.7% and 22.6% of the general public need depression and anxiety screening is alarming.
To the best of our knowledge, this study is the first to survey the general public using the PHQ-4 in Korea, and no previous research data exist to compare our results. Thus, there were limitations in comparing the pre-COVID-19 period with the COVID-19 period. However, among studies published before the outbreak of COVID-19, a 2014 study conducted on the general public in Korea reported that 6.7% of the population scored 10 or higher on the PHQ-9, which indicates the need for depression screening.
17 A 2011 study in Hong Kong and a 2014 study in Germany reported rates of 4.2% and 6.4%, respectively, for a PHQ-2 score of 3 or higher, and a 2011 study in Austria and a 2014 study in Germany reported rates of 10.2% and 4.8%, respectively, for a GAD-2 score of 3 or higher, which are markedly different from our results.
141819 Additionally, a study that compared depression and anxiety before and after COVID-19 using PHQ-9 and GAD-7 in May 2020 in Hong Kong reported that depression and anxiety rose from 10.7% to 19.8% and from 4.1% to 14.0%, respectively.
20 While a direct comparison is difficult, these results suggest that the prevalence of depression and anxiety increased after the outbreak of COVID-19 in Busan, Korea, highlighting the importance of early intervention.
This study also aimed to identify the factors associated with depression and anxiety during the COVID-19 pandemic. Among the various factors found to predict depression and anxiety, changes in sleep pattern due to COVID-19 were the most potent predictors of depression, followed by restrictions in outside activities and increased family conflicts. For anxiety, changes in sleep pattern due to COVID-19 were also the most potent predictors, followed by time spent using media to obtain COVID-19-related information and fear of infection.
Changes in sleep pattern had the strongest association with both depression and anxiety. Sleep problems are known to be closely linked to depression and anxiety, as evident by its inclusion in the DSM-5 diagnostic criteria for major depressive disorder and generalized anxiety disorder.
21 According to a study published in July 2020 in Hong Kong, 38.3% of the participants reported a deteriorated quality of sleep after the outbreak of COVID-19, and 29.8% and 29.1% of the participants reported having difficulty initiating sleep or sleeping less since the outbreak of COVID-19, respectively. Moreover, 29.9% of the participants had an ISI of 10 or higher, indicating clinical insomnia.
7 When viewed in light of our results, it is evident that sleep problems have emerged as an important mental health problem during the COVID-19 pandemic, and there is a need for assessment and early intervention for sleep problems to relieve depression and anxiety.
In Busan, Korea, level 2 social distancing was implemented on August 17, 2020, during the study period. People were advised to refrain from using multipurpose facilities where people gather, and mandatory remote learning was extended for students. Moreover, indoor social gatherings of 50 or more people and outdoor social gatherings of 100 or more people were banned. These measures curtailed individuals' outdoor activities. The consequent social isolation and loneliness severely impacted individuals' depression. Furthermore, many Korean adults live with their families, as opposed to living alone. Due to the nature of such a living arrangement, most people spent more time with their family within a restricted space because of restrictions on outdoor activities. This may have been helpful in terms of loneliness, but it may also have triggered family conflicts. Further, conflicts with family members, with whom one must live every day, may be a cause of severe depression in individuals.
The impact of public media on anxiety has been extensively documented in the literature. A paper published in December 2020 reported that exposure to the mass media did not significantly increase one's level of knowledge about COVID-19 and only increased their anxiety about infection and bias toward infected individuals.
22 In today's world where media is replete with non-validated information, individuals are easily exposed to incorrect information, superstitions, and urban myths. Moreover, exposure to such information increases anxiety. Therefore, the government and health care professionals must implement measures to curb misinformation and strive to alleviate anxiety among the general public by delivering accurate and evidence-based information via reputable media.
Finally, fear of fatal outcomes of infection was also associated with increased anxiety. As of August 15, during the study period, the total number of deaths from COVID-19 in Korea was 305. Worldwide, the number of deaths was 757,003, with a fatality rate of 3.60%. Based on these statistics, it is reasonable for individuals to think that they might have fatal outcomes if they contract COVID-19. However, if such thinking intensifies, it may lead to “catastrophizing,” a type of cognitive error stated in cognitive behavioral therapy, which would exacerbate their anxiety level. A Chinese study published in March 2020 proposed online-based cognitive behavioral therapy as a potential early intervention.
23 This is an intervention worth consideration in Korea, where “contactless” has become a social trend.
This study has several strengths and limitations. One strength is that a large study sample was used by sampling the population using quota sampling based on sex, age, and region. Thus, our study sample represents the general public in Busan, Korea. Further, we examined the current levels of depression and anxiety and their associated factors among residents of a single city (Busan). Thus, the results will be useful in devising mental health policies tailored to the context of the city. One limitation of this study is that a contactless, self-reported questionnaire survey was conducted. This type of survey is prone to overestimation of study parameters, which may impact the reliability of the information.
24 Second, this study was a cross-sectional study; therefore, the causality between depression and anxiety and their associated factors could not be determined. Third, participants' socioeconomic status and pre-existing physical and mental health disorders were not surveyed. These factors may serve as potential confounders influencing depression and anxiety. Fourth, the PHQ-4 is a simple screening tool with fewer questions compared to the PHQ-9 or GAD-7, so it is possible that participants' depression and anxiety might have been overestimated.
In essence, based on the PHQ-4 scores, 30.7% and 22.6% of the study sample consisting of Busan residents can be considered at risk for depression and anxiety, respectively. This suggests the high prevalence of depression and anxiety in the society during the COVID-19 pandemic. Furthermore, regression analysis confirmed that sleep problems, restrictions with outdoor activities, and increased family conflicts were associated with depression; while sleep problems, time spent using media, and fear of infection were associated with anxiety. Although additional studies are needed to examine the causal relationships among these factors, this study contributes to the literature by examining the current levels of depression and anxiety among the general public using a simple screening tool and identifying the potential targets of early intervention amid the growing importance of early intervention for mental health problems caused by the COVID-19 pandemic.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download