1. Draper ES, Manktelow B, Field DJ, James D. Prediction of survival for preterm births by weight and gestational age: retrospective population based study. BMJ. 1999; 319(7217):1093–1097. PMID:
10531097.

2. Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. National Institute of Child Health and Human Development Neonatal Research Network. Intensive care for extreme prematurity--moving beyond gestational age. N Engl J Med. 2008; 358(16):1672–1681. PMID:
18420500.

3. Patel RM, Rysavy MA, Bell EF, Tyson JE. Survival of infants born at periviable gestational ages. Clin Perinatol. 2017; 44(2):287–303. PMID:
28477661.

4. Shim JW, Jin HS, Bae CW. Changes in survival rate for very-low-birth-weight infants in Korea: comparison with other countries. J Korean Med Sci. 2015; 30(Suppl 1):S25–S34. PMID:
26566354.

5. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 101: Ultrasonography in pregnancy. Obstet Gynecol. 2009; 113(2 Pt 1):451–461. PMID:
19155920.
6. Seri I, Evans J. Limits of viability: definition of the gray zone. J Perinatol. 2008; 28(Suppl 1):S4–S8. PMID:
18446176.

7. Sauve RS, Robertson C, Etches P, Byrne PJ, Dayer-Zamora V. Before viability: a geographically based outcome study of infants weighing 500 grams or less at birth. Pediatrics. 1998; 101(3 Pt 1):438–445. PMID:
9481011.

8. Salihu HM, Emusu D, Aliyu ZY, Kirby RS, Alexander GR. Survival of “pre-viable” infants in the United States. Wien Klin Wochenschr. 2005; 117(9-10):324–332. PMID:
15989111.

9. Rieger-Fackeldey E, Schulze A, Pohlandt F, Schwarze R, Dinger J, Lindner W. Short-term outcome in infants with a birthweight less than 501 grams. Acta Paediatr. 2005; 94(2):211–216. PMID:
15981756.

10. Inoue H, Ochiai M, Yasuoka K, Tanaka K, Kurata H, Fujiyoshi J, et al. Early mortality and morbidity in infants with birth weight of 500 grams or less in Japan. J Pediatr. 2017; 190:112–117.e3. PMID:
28746032.

11. Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015; 372(19):1801–1811. PMID:
25946279.

12. Chang YS, Park HY, Park WS. The Korean Neonatal Network: an overview. J Korean Med Sci. 2015; 30(Suppl 1):S3–S11. PMID:
26566355.

13. Lee JH, Noh OK, Chang YS; Korean Neonatal Network. Neonatal outcomes of very low birth weight infants in Korean Neonatal Network from 2013 to 2016. J Korean Med Sci. 2019; 34(5):e40. PMID:
30718992.

14. Chang YS, Kim YJ, Koo SH, Lee JH, Hwang JH, Choi CW, et al. Outcomes and management of fetal infants with birth weight below 500 g at a tertiary center. Korean J Pediatr. 2005; 48(9):939–945.
15. Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013; 13(1):59. PMID:
23601190.

16. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163(7):1723–1729. PMID:
11401896.

17. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92(4):529–534. PMID:
305471.

18. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187(1):1–7. PMID:
413500.
19. Bae YM, Bae CW. The changes in the mortality rates of low birth weight infant and very low birth weight infant in Korea over the past 40 years. J Korean Med Sci. 2004; 19(1):27–31. PMID:
14966337.

20. Peacock JL, Marston L, Marlow N, Calvert SA, Greenough A. Neonatal and infant outcome in boys and girls born very prematurely. Pediatr Res. 2012; 71(3):305–310. PMID:
22258087.

21. O'Driscoll DN, McGovern M, Greene CM, Molloy EJ. Gender disparities in preterm neonatal outcomes. Acta Paediatr. 2018; 107(9):1494–1499.
22. Papiernik E, Zeitlin J, Delmas D, Blondel B, Künzel W, Cuttini M, et al. Differences in outcome between twins and singletons born very preterm: results from a population-based European cohort. Hum Reprod. 2010; 25(4):1035–1043. PMID:
20118116.

23. Effect of corticosteroids for fetal maturation on perinatal outcomes. NIH Consensus Development Panel on the Effect of Corticosteroids for Fetal Maturation on Perinatal Outcomes. JAMA. 1995; 273(5):413–418. PMID:
7823388.
24. Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ, Ehrenkranz RA, et al. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22 to 25 weeks' gestation. JAMA. 2011; 306(21):2348–2358. PMID:
22147379.

25. American Academy of Pediatrics Committee on Fetus and Newborn. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. The Apgar score. Pediatrics. 2015; 136(4):819–822. PMID:
26416932.
26. Cnattingius S, Johansson S, Razaz N. Apgar score and risk of neonatal death among preterm infants. N Engl J Med. 2020; 383(1):49–57. PMID:
32609981.

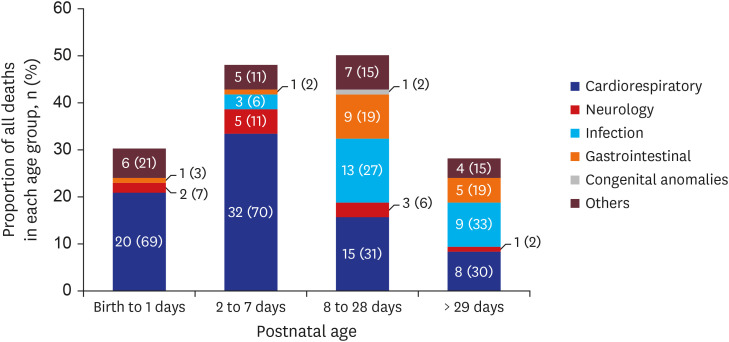
27. Park JH, Chang YS, Sung S, Park WS. Korean Neonatal Network. Mortality rate-dependent variations in the timing and causes of death in extremely preterm infants born at 23–24 weeks' gestation. Pediatr Crit Care Med. 2019; 20(7):630–637. PMID:
31013260.

28. Rocha G, Flor de Lima F, Riquito B, Guimarães H. Very preterm infant outcomes according to timing of birth. J Neonatal Perinatal Med. 2020; 13(1):97–104. PMID:
31796686.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download