INTRODUCTION
Non-obstetric surgery during pregnancy which occurs 1–2% in pregnant women is associated with adverse outcomes.
1 In a Canadian study of 2,565 pregnant women, there was increased risk of spontaneous abortion after general anesthesia.
2 Two nationwide studies in Sweden and UK showed increased risk of adverse outcomes such as stillbirth, preterm delivery, and low birth weight.
34 The American College of Obstetricians and Gynecologists (ACOG) committee noted that, although no teratogenic effect of anesthetics during pregnancy has been proven, obstetric and fetal complications may increase.
Laparoscopic surgery during pregnancy has become widely used although there has been concern for uterine injury from trocar and fetal malperfusion due to pneumoperitoneum during surgery over the past two decades.
5 Several systematic reviews and meta-analyses have suggested that laparoscopic surgery may be similar or preferable to laparotomy during pregnancy.
67891011 Most previous studies, however, have included a small number of patients and targeted only certain operations such as appendectomy or ovarian surgery. Recent nationwide study confirmed the advantages of laparoscopic surgery compared with laparotomy in 6,018 pregnant women who underwent surgery. However, that study was limited because it did not evaluate risk of major complications including preterm birth and low birth weight, but only assessed abortion and stillbirth within 7 days after surgery and premature birth during hospitalization.
12
We investigated the risk of adverse outcomes for women who underwent non-obstetric surgery during pregnancy compared with those who did not undergo such surgery. We also compared adverse outcomes after laparoscopy versus laparotomy.
METHODS
Healthcare system in Korea
In 2000, numerous health insurance systems in South Korea have been combined into a single system run by the National Health Insurance Service (NHIS). Therefore, most people living in South Korea are currently registered by the NHIS. Our study data were retrieved from the Korea National Health Insurance (KNHI) claims database from 2007–2015. In Korea, 97% of the population is obligated to participate in the KNHI program; the remaining 3% are belonged to the Medical Aid Program. Therefore, the KNHI claims database includes information on all claims for approximately 50 million Koreans, and almost all information about incidence of disease can be assessed from this database except for procedures not covered by insurance such as cosmetic surgery.
Study population
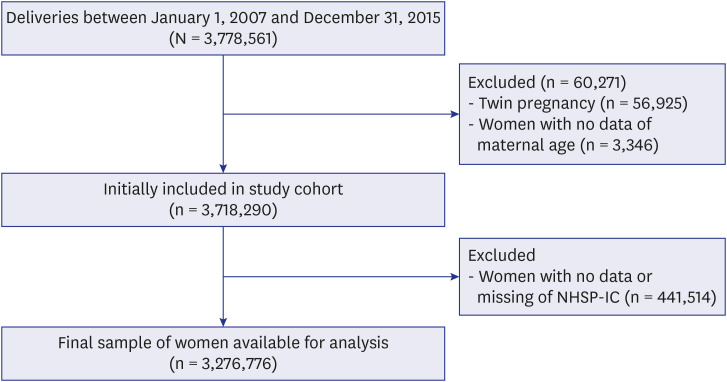
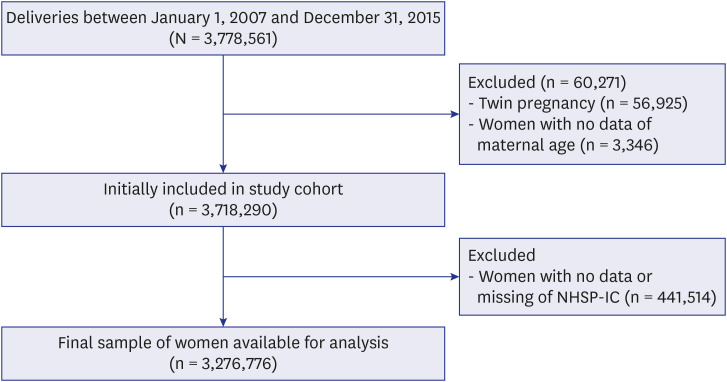
Fig. 1 showed a flow diagram of patient enrollment. We identified all women who gave birth from January 2007 to December 2015 using the KNHI claims database. Inclusion criteria were as follows: women who gave birth between January 2006 and December 2016, and had undergone the National Health Screening Program for Infant and Children (NHSP-IC) visit to evaluate neonatal characteristics. Women with no or missing NHSP-IC data were excluded from this study.
Fig. 1
Study design.
NHSP-IC = National Health Screening Program for Infant and Children.

We identified pregnant women who underwent non-obstetric surgery from the database. Patients who underwent non-obstetric surgery at the time of cesarean delivery were excluded. In this study, non-obstetric surgeries (by laparoscopy or laparotomy) included the two most common operative procedures for benign diseases: appendectomy and adnexal mass resection. The operative procedures were identified by the presence of a Korea Medical Insurance electronic data interchange (EDI) code (Appendectomy: Q2861/Q2862/Q2863, Adnexal mass resection: R4430/R4421). Laparoscopic surgery was identified by the associated Korea Medical Insurance EDI code (N0031001).
Outcomes
The primary pregnancy outcome was neonatal complications, including premature birth and low birth weight (LBW). Secondary outcomes were obstetric complications, including gestational hypertension, gestational diabetes mellitus (GDM), postpartum hemorrhage (PPH), cesarean section (C/S), and length of hospital stay after surgery. Patient characteristics such as maternal age, parity, placenta previa and placenta abruptio were evaluated using the KNHI claims database. The length of hospital stay after surgery and the time interval between surgery and delivery were also measured.
Statistical analysis
Continuous and categorical variables were described as mean ± standard deviation and percentages, respectively. Clinical characteristics were compared using the t-test for continuous variables and the χ2 test for categorical variables. Multivariate regression analysis models were used to estimate the adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) for primary and secondary endpoints. All tests were two-tailed, and P values < 0.05 were considered statistically significant. Statistical analyses were performed using SPSS version 18 (IBM Corp., Armonk, NY, USA).
Ethics statement
All procedures were in accordance with the ethical standards of the Institutional Review Board of Korea University Medical Center (No. 2020GR0109) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Retrospective data collection was anonymized and routinely collected as part of clinical practice and used for audit purposes. Informed consent was waived because of the retrospective nature of the study.
RESULTS
From a total of 3,276,776 of women who gave birth during 2007–2015, 8,167 (0.25%) underwent non-obstetric abdominal surgery, including 5,109 laparotomy patients and 3,108 laparoscopy patients.
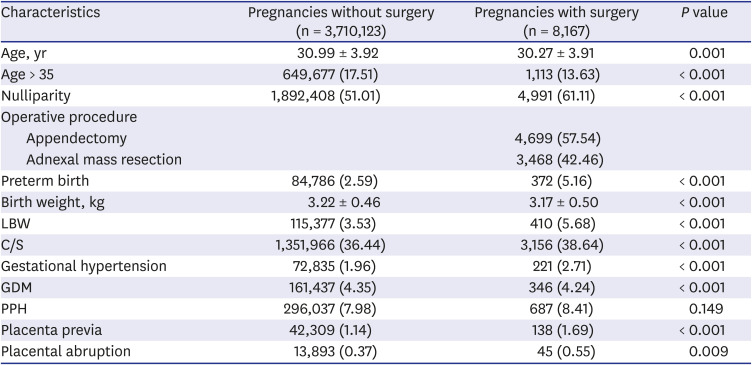
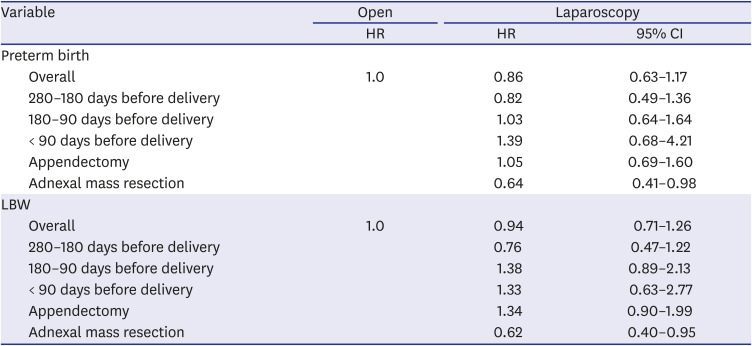
Table 1 shows the general and pregnancy characteristics of patients between pregnancies with and without surgery. For pregnancies in the surgery group, maternal age < 35 years, nulliparity, preterm birth, LBW, gestational hypertension, GDM, C/S, placenta previa, and placenta abruption were more common than in pregnancies in the group that did not undergo surgery.
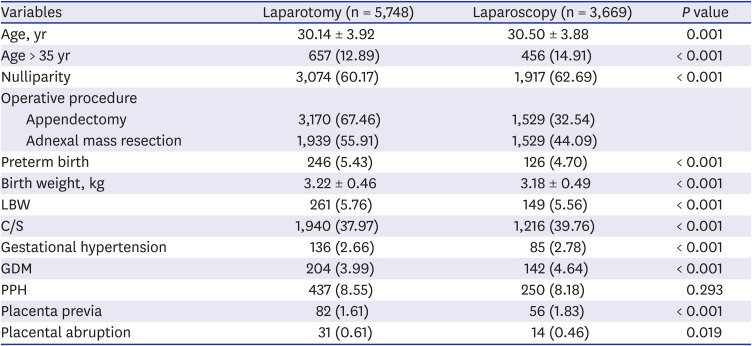
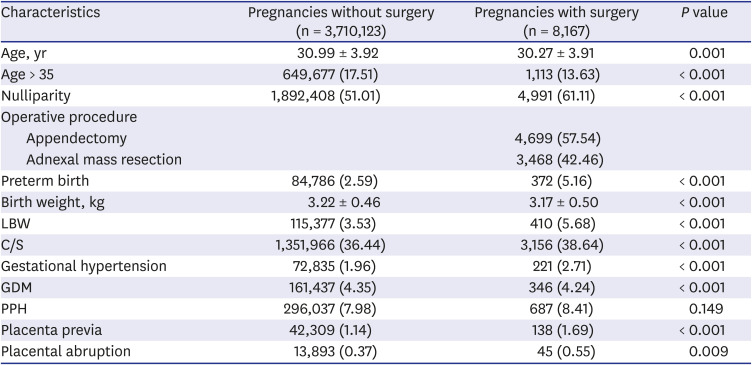
Table 2 shows the general and pregnancy characteristics of the laparoscopy and laparotomy groups. When comparing laparoscopy and laparotomy, in the laparoscopy group, maternal age < 35 years, nulliparity, C/S, gestational hypertension, GDM, and placenta previa were more common than in the laparotomy group. Preterm delivery, low birth weight, and placenta abruption were less common in the laparoscopic group compared with the laparotomy group.
Table 1
General and pregnancy characteristics of patients
|
Characteristics |
Pregnancies without surgery (n = 3,710,123) |
Pregnancies with surgery (n = 8,167) |
P value |
|
Age, yr |
30.99 ± 3.92 |
30.27 ± 3.91 |
0.001 |
|
Age > 35 |
649,677 (17.51) |
1,113 (13.63) |
< 0.001 |
|
Nulliparity |
1,892,408 (51.01) |
4,991 (61.11) |
< 0.001 |
|
Operative procedure |
|
|
|
|
Appendectomy |
|
4,699 (57.54) |
|
|
Adnexal mass resection |
|
3,468 (42.46) |
|
|
Preterm birth |
84,786 (2.59) |
372 (5.16) |
< 0.001 |
|
Birth weight, kg |
3.22 ± 0.46 |
3.17 ± 0.50 |
< 0.001 |
|
LBW |
115,377 (3.53) |
410 (5.68) |
< 0.001 |
|
C/S |
1,351,966 (36.44) |
3,156 (38.64) |
< 0.001 |
|
Gestational hypertension |
72,835 (1.96) |
221 (2.71) |
< 0.001 |
|
GDM |
161,437 (4.35) |
346 (4.24) |
< 0.001 |
|
PPH |
296,037 (7.98) |
687 (8.41) |
0.149 |
|
Placenta previa |
42,309 (1.14) |
138 (1.69) |
< 0.001 |
|
Placental abruption |
13,893 (0.37) |
45 (0.55) |
0.009 |

Table 2
General and pregnancy characteristics in laparotomy and laparoscopy groups
|
Variables |
Laparotomy (n = 5,748) |
Laparoscopy (n = 3,669) |
P value |
|
Age, yr |
30.14 ± 3.92 |
30.50 ± 3.88 |
0.001 |
|
Age > 35 yr |
657 (12.89) |
456 (14.91) |
< 0.001 |
|
Nulliparity |
3,074 (60.17) |
1,917 (62.69) |
< 0.001 |
|
Operative procedure |
|
|
|
|
Appendectomy |
3,170 (67.46) |
1,529 (32.54) |
|
|
Adnexal mass resection |
1,939 (55.91) |
1,529 (44.09) |
|
|
Preterm birth |
246 (5.43) |
126 (4.70) |
< 0.001 |
|
Birth weight, kg |
3.22 ± 0.46 |
3.18 ± 0.49 |
< 0.001 |
|
LBW |
261 (5.76) |
149 (5.56) |
< 0.001 |
|
C/S |
1,940 (37.97) |
1,216 (39.76) |
< 0.001 |
|
Gestational hypertension |
136 (2.66) |
85 (2.78) |
< 0.001 |
|
GDM |
204 (3.99) |
142 (4.64) |
< 0.001 |
|
PPH |
437 (8.55) |
250 (8.18) |
0.293 |
|
Placenta previa |
82 (1.61) |
56 (1.83) |
< 0.001 |
|
Placental abruption |
31 (0.61) |
14 (0.46) |
0.019 |

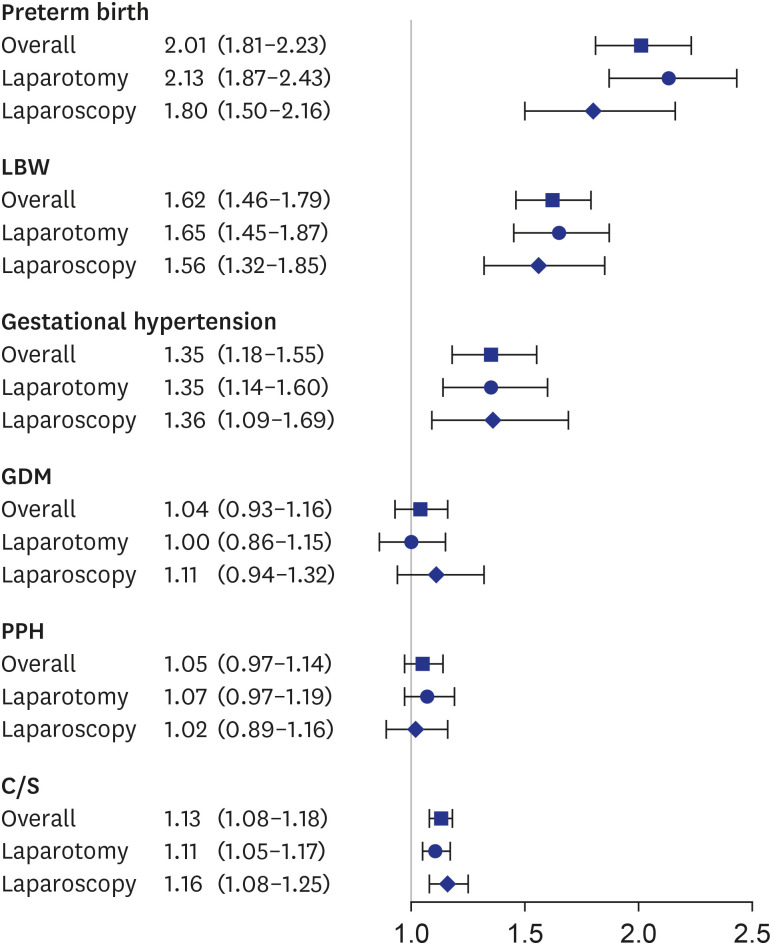
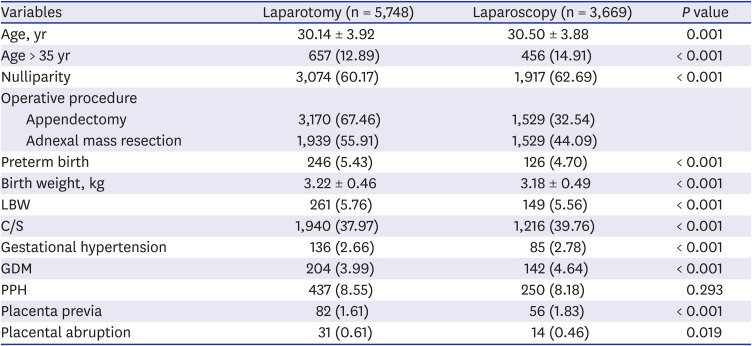
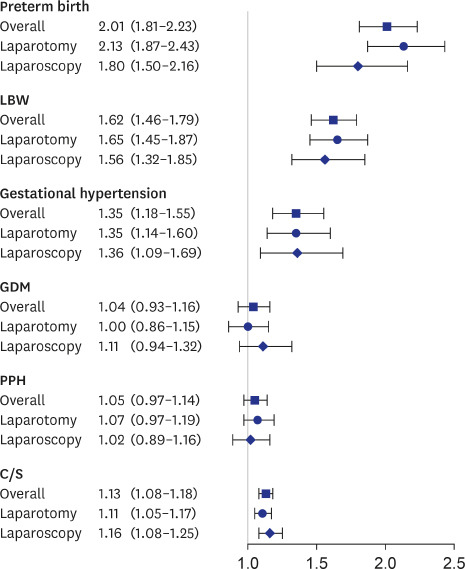
Fig. 2 shows the results of Cox proportional hazards regression analyses with fetal and obstetric complications after controlling for age, parity, and placenta previa. There was a statistically significant increase in risk of preterm birth (HR, 2.01; 95% CI, 1.81–2.23), LBW (HR, 1.62; 95% CI, 1.46–1.79), C/S (HR, 1.13; 95% CI, 1.08–1.18), and gestational hypertension (HR, 1.35; 95% CI, 1.18–1.55).
Fig. 2
Forest plot of HR for risk of adverse fetal and pregnancy outcomes associated with non-obstetric pelvic surgery during pregnancy. Age- and parity-adjusted HR and 95% CI were estimated.
HR = hazard ratio, CI = confidence interval, LBW = low birth weight, GDM = gestational diabetes mellitus, PPH = postpartum hemorrhage, C/S = cesarean section.

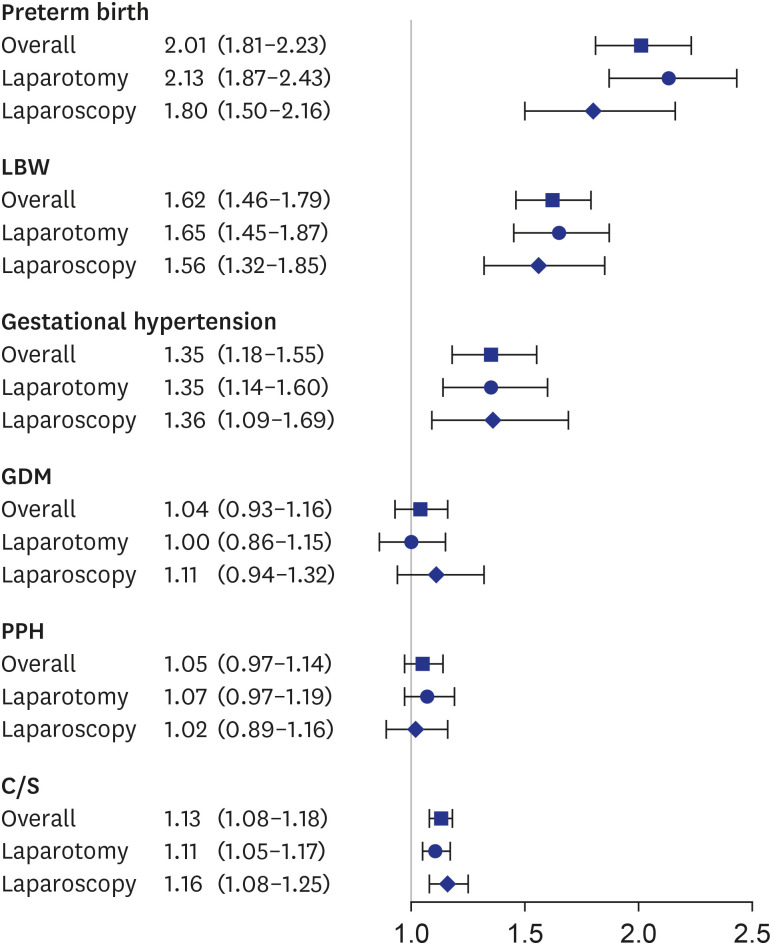
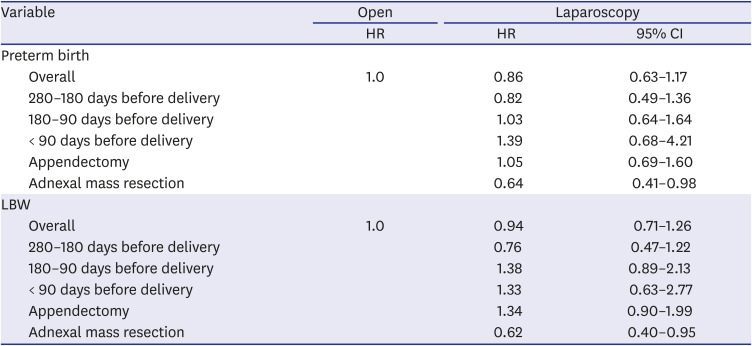
When comparing the laparoscopic and laparotomy groups for risk of fetal outcomes, the risk of preterm birth (HR, 0.64; 95% CI, 0.41–0.98) and LBW (HR, 0.62; 95% CI, 0.40–0.95) was significantly decreased in laparoscopic adnexal resection during pregnancy compared to laparotomy (
Table 3). Otherwise, there were no statistically significant differences between the two groups. In addition, in the laparoscopic group, the hospital stay was statistically significantly shorter than for the laparotomy group (6.13 ± 2.76 vs. 5.62 ± 2.75 days,
P < 0.001).
Table 3
Age- and parity-adjusted fetal outcomes stratified according to timing of surgery and type of surgery in the laparoscopy group compared with the open group
|
Variable |
Open |
Laparoscopy |
|
HR |
HR |
95% CI |
|
Preterm birth |
|
|
|
|
Overall |
1.0 |
0.86 |
0.63–1.17 |
|
280–180 days before delivery |
|
0.82 |
0.49–1.36 |
|
180–90 days before delivery |
|
1.03 |
0.64–1.64 |
|
< 90 days before delivery |
|
1.39 |
0.68–4.21 |
|
Appendectomy |
|
1.05 |
0.69–1.60 |
|
Adnexal mass resection |
|
0.64 |
0.41–0.98 |
|
LBW |
|
|
|
|
Overall |
1.0 |
0.94 |
0.71–1.26 |
|
280–180 days before delivery |
|
0.76 |
0.47–1.22 |
|
180–90 days before delivery |
|
1.38 |
0.89–2.13 |
|
< 90 days before delivery |
|
1.33 |
0.63–2.77 |
|
Appendectomy |
|
1.34 |
0.90–1.99 |
|
Adnexal mass resection |
|
0.62 |
0.40–0.95 |

When comparing the adnexal mass resection and appendectomy group for fetal and obstetrics complications, fetal complications tended to increase slightly in the open adnexal mass resection group compared to the open appendectomy group, but there was no statistically significant difference between two groups (
Supplementary Table 1).
DISCUSSION
This study showed that there was higher incidence and risk of preterm birth, low birth weight, gestational hypertension, and C/S in women who underwent non-obstetric pelvic surgery during pregnancy compared to pregnant women who did not undergo such surgery. The risk of preterm birth and LBW was significantly increased in the laparotomy group compared with laparoscopy group among the pregnant women who underwent ovarian resection. In addition, in the laparoscopic group, the hospital stay was significantly shorter than for the laparotomy group.
This study demonstrated higher risk of six adverse outcomes including preterm birth and LBW in women who underwent pelvic surgery during pregnancy compared to pregnant women who did not. This result is consistent with previous large studies.
2341314 A Swedish study of 2 million pregnancies suggested increased risk of LBW, preterm birth and growth restriction for fetuses of pregnant women who underwent surgery compared with the total population.
3 In cohort study of 6.5 million pregnancies in England, surgical operations were associated with additional stillbirth (1 per 287 surgery), preterm delivery (1 per 31 surgery), LBW (1 per 39 surgery), and C/S (1 per 25 surgery).
4 In a Taiwanese registry-based study of 150,000 pregnancies, non-obstetric surgery during pregnancy was associated with higher risk of spontaneous abortion (adjusted odd ratio [aOR], 1.53; 95% CI, 1.01–2.31), pre-eclampsia/eclampsia (aOR, 2.35; 95% CI, 1.30–4.23), gestational diabetes (aOR, 3.12; 95% CI, 1.69–5.78), prematurity (aOR, 3.31; 95% CI, 2.54–4.31), and C/S (aOR, 1.41; 95% CI, 1.17–1.71).
13
In this study, the risk of preterm birth and LBW was significantly increased for pregnant women who underwent open ovarian resection compared with laparoscopy. There are inconsistent results between previous studies. In 1997, a Swedish health registry study suggested that there was no difference in birth weight, preterm birth, growth restriction, infant survival, or fetal malformations for patients undergoing laparoscopy versus open surgery in singleton pregnancies. On other hand, a recent Japanese registry study showed that laparoscopic surgery was beneficial in terms of short-term fetal adverse events, incidence of blood transfusion, operative time, and hospital stay.
12 In a retrospective study of 262 Korean pregnant women who underwent open or laparoscopic adnexal mass resection, no significant difference was observed between two groups in adverse outcomes including preterm birth and miscarriage rate when adjusted for confounding factors such as gestational age at surgery, emergency operation and mass size.
15
However, there are some limitations to these studies. Since the Swedish study was conducted 20 years ago, the results of the study were limited for evaluating the impact of laparoscopic surgery on pregnancy. In addition, there were very few laparoscopic surgeries during the second or third trimester. In Japanese study, LBW and preterm birth were not identified. Moreover, the risk of multiple obstetric complications such as gestational hypertension and gestational diabetes during pregnancy was not assessed. As there are no related studies for ovarian resection, further studies are needed to validate the results of this study.
This study showed that hospital stay in the laparoscopy group was statistically significantly shorter than that in the laparotomy group. It has also been reported in several studies. According to the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines, advantages of laparoscopy during pregnancy appear similar to those in non-pregnant patients such as less pain and ileus, shorter hospital stays, and faster recovery.
5 A Japanese study showed that the laparoscopy group had a significantly shorter hospital stay (9.2 vs. 5.9 days,
P < 0.001) compared with the laparotomy group.
12 In a Korean study also demonstrated that laparoscopy group had a significantly shorter operation time (60.7 ± 27.1 vs. 69.7 ± 24.4 minutes,
P = 0.002) and hospital stay (4.7 ± 1.7 vs. 6.6 ± 1.3 days,
P < 0.001).
15
Our findings should be interpreted in the light of some inherent limitations of a claims database. First, this was a retrospective study. Second, other abdominopelvic surgeries such as cholecystectomy and myomectomy were excluded from the analysis due to their small number, indicating the need for additional research on these procedures. Third, there was a lack of clinical information about gestational age. Therefore, we estimated the time interval between surgery and delivery to control bias due to time of surgery. Fourth, because the study only included data on women who had live birth, no information about stillbirth was available. Finally, some important clinical characteristics of patients such as smoking and alcohol drinking habits, body mass index, and severity of comorbid conditions, were not accessible.
Nevertheless, there were many strengths to this study. This is the first nationwide study to report the risk of adverse obstetric and fetal outcomes following non-obstetric pelvic surgery during pregnancy in Korea. This is the second largest study worldwide as well as the largest such study in Asia and is based on a registry database from 3.2 million pregnancies. Furthermore, it is the first large-scale study to analyze the risk of comprehensive obstetrics and fetal adverse outcomes according to laparoscopic/open surgery, type of surgery, and time of surgery during pregnancy.
Non-obstetric pelvic surgery during pregnancy was associated with higher risk of preterm birth, LBW, gestational hypertension, placenta previa, placental abruption, and C/S. Although the benefits and safety of laparoscopy during pregnancy appear similar to those of laparotomy in pregnancy outcomes, laparoscopic adnexal mass resection was associated with a lower risk of LBW. The results of this study should be considered when selecting surgical and procedural approaches to optimize patient outcomes.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download