INTRODUCTION
The percent of elderly people in the world's population is increasing as a consequence of life expectancy increases, which are due to health and medical progress and a decrease in birthrate [
1]. Projections based on the assumption that the current demographic trends will continue indicate that the 21st century will be the “century of the old” in Turkey, which will be paralleled in populations around the world. In Turkey, the elderly population proportion of the total population was 8.7% in 2018. According to population projections, the elderly population proportion in Turkey is estimated to be 10.2% in 2023, 12.9% in 2030, 16.3% in 2040, 22.6% in 2060, and 25.6% in 2080 [
2].
In the aging process, various physiological, psychological, economic, and social changes can adversely affect a person's nutritional status. Such malnutrition can be accompanied by disease and weakness. The elderly may have nutritional problems and can become predisposed to the risk of malnutrition [
1]. Among the main nutritional disorders are malnutrition, overweight status, obesity, micronutrient abnormalities, and refeeding syndrome. Sarcopenia and frailty are conditions related to nutritional status and are associated with multiple complex factors [
3]. Both diet and lifestyle change contribute significantly to the development of age-related diseases, and dietary modification may contribute to the prevention of age-related diseases, thereby helping to improve the quality of life in old age [
4].
Malnutrition is a multifactorial condition among senior adults. According to a systematic review, demographic characteristics, financial characteristics, food access, appetite status, lifestyle, psychological characteristics, physical functioning, disease, oral health, and social factors can have effects on malnutrition [
5]. In the elderly, unintentional weight losses of over 5% in the last month or over 10% in the last 6 months are associated with morbidity, mortality, and postoperative complications [
6]. Studies assessing the prevalence of malnutrition among community-living elderly subjects have reported a malnutrition prevalence of 2–8% and a prevalence of malnutrition risk of 24–36% [
7]. In a study conducted in Turkey, the risk of malnutrition was 31%, and the rate of malnutrition was 13% among geriatric outpatients, whereas malnutrition risk was 39% and malnutrition rate was 25% among hospitalized patients [
8].
Malnutrition in residential areas and nursing homes is often associated with cognitive impairment, hypotension, infection, and anemia, and it may result in the deterioration of physical activities in daily life, such as dressing and washing. In hospitals, the risk of malnutrition may increase due to prolongation of hospital stay, increased morbidity, fractures, infection, and specific nutritional deficiencies, and may result in mortality [
9].
A nutritional intake assessment, a component of a nutritional status assessment, is necessary when planning individual nutritional interventions, and it is also beneficial when developing public health and nutrition policies [
10]. Changes in body composition and nutrition that occur during the aging process differ in men and women during different life stages and can be reflected by anthropometric measurements. Therefore, anthropometric measurements are an important part of nutritional assessment in geriatric medicine, because it allows determination of the patient's malnutrition, overweight, and obesity status and allows the assessment of muscle mass loss, fat mass gain and loss, and the distribution of adipose tissue [
11].
This study performed screening of malnutrition risk by using the Mini Nutritional Assessment (MNA)-long form screening tool and identified malnutrition risk factors in elderly patients in a geriatric outpatient clinic of a hospital in Istanbul, Turkey. Additionally, this study compared elderly patients with malnutrition and patients with a normal nutritional status and identified risk factors that significantly contribute to the variability between the 2 groups.
Go to :

DISCUSSION
Based on the MNA evaluation, we have shown that 24.7% of Turkish patients of this study were at risk for malnutrition and 3.3% of them were malnourished. In another study conducted in Turkey, malnutrition risk was detected in 29.1% of the elderly individuals, and malnutrition was found in 19% of these patients [
17]. In a study conducted by Mitri
et al. [
18] that evaluated nutritional status and risk factors affecting elderly individuals (n = 905) in Lebanon, malnutrition risk was present in 45.5% of the individuals, and malnutrition was present in 2.8% of them. In a study conducted by Agarwalla
et al. [
19], the nutritional status of 360 Indian older individuals' was evaluated; 15% of them were malnourished, and 55% of them had a risk of malnutrition. In a study conducted by Damayanthi
et al. [
20] in Sri Lanka, malnutrition was present in 12.5% of 999 elderly individuals (mean age 70.8 years), and malnutrition risk was detected in 52.5% of them.
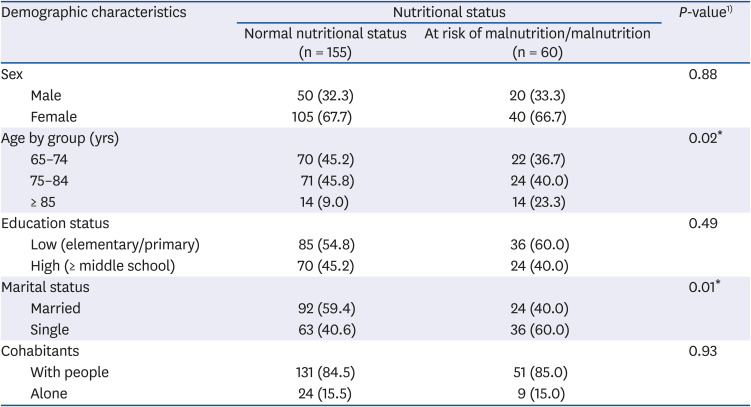
Although the results of our study are similar to the results of other studies, we have detected several malnutrition risk factors. In this study, among the sociodemographic variables, older age and being single from were associated with a poor nutritional status. Other studies have reported an association between older age, lower education, inadequate income [
21], being single [
22], and social isolation [
23] and the risk of malnutrition. In a study conducted by Kalan
et al. [
15], malnutrition was detected in 6.6%, and malnutrition risk was detected in 31.6% of Turkish patients in Turkey. In their malnourished group, self-perception of health (87.9%), protein intake (86.4%), and taking at least 3 medications (77.3%) per day were the parameters associated with the greatest decrease in MNA score [
15]. In the same study, protein intake (86.7%), health perception (74.7%), and taking at least 3 medications per day (65.2%) were the 3 parameters that were associated with the greatest decrease in MNA score in patients at risk of malnutrition [
15].
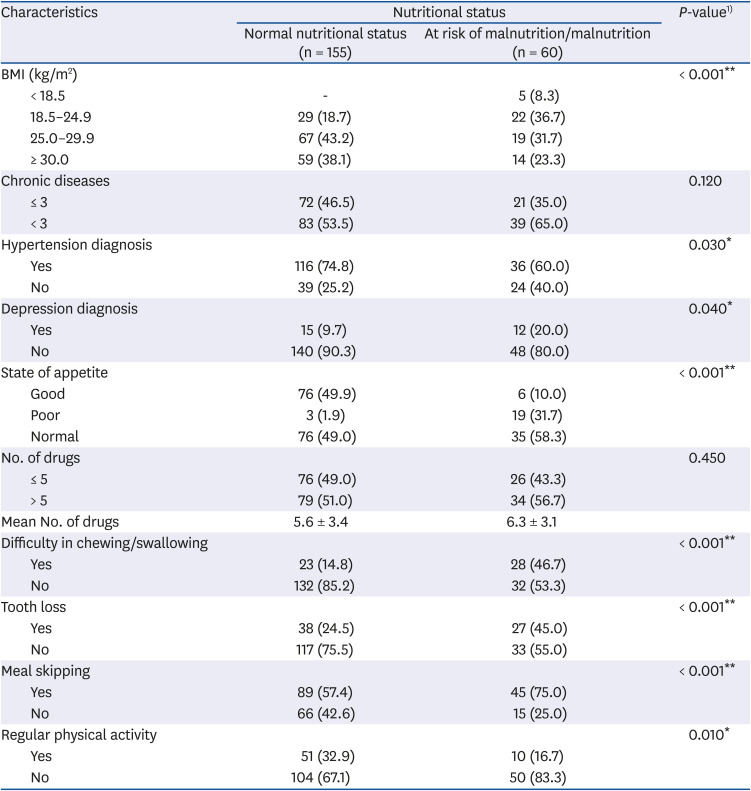
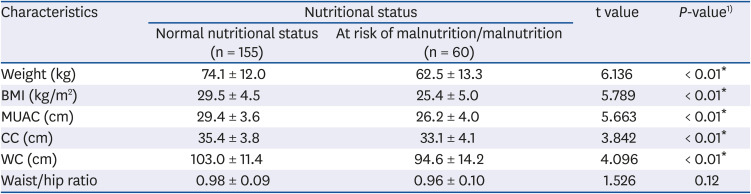
In our study, statistically significant differences were detected between nutritional status and mean body weight, BMI, MUAC, CC, waist circumference, and hip circumference (
P < 0.01). Although there are differences between the anthropometric values of the patients in both groups when classified according to MNA score, it is apparent that they have normal or high values according to standard reference values (
Table 3). We suggest that this may be related to the similar protein intake levels in the 2 groups (
Table 4). A poor nutritional status was not only present in the low-weight elderly categories as expected, but was also observed in subjects that were overweight or obese. In addition, although the waist/hip ratio was higher in the group with normal nutritional status than in the other group, in both groups, the value was higher than the standard reference value. We suggest that this result parallels that for the BMI data. These results indicate that malnutrition may occur if nutritional counseling of obese or overweight elderly adults is not performed correctly. The right advice should be directed towards a balanced and nutritious diet that meets both macro- and micronutrient needs, rather than focusing on weight loss. In a study conducted in Tarragona, Spain, the mean MNA score of 190 older individuals (67.5% female) with an average age of 85 years was 20, and 21% of them were underweight while 43.2% of them were overweight or obese [
24]. According to a study conducted in Northern Cyprus, BMI, MUAC, and CC values of patients in the malnutrition/malnutrition risk group (mean age 73 years) averaged 28.6 kg/m
2, 29.3 cm, and 34.1 cm, respectively, while the averages in patients with a normal nutritional status were 31.3 kg/m
2, 31.6 cm, and 35.5 cm, respectively [
25]. According to a study in Brazil, BMI, MUAC, and CC values of patients in the malnutrition/malnutrition risk group (mean age 72.9 years) averaged 21.6 kg/m
2, 25.7 cm, and 31.1 cm, respectively, whereas the averages in patients with a normal nutritional status (mean age 69.1 years) were be 26.7 kg/m
2, 30.3 cm, and 33.9 cm, respectively [
26]. These observations suggest that anthropometric measurements of elderly individuals should be obtained routinely, and individuals with high anthropometric measurements should be considered at risk for poor nutrition status.
In our study, we could not find a statistically significant difference between the number of chronic diseases or the number of drugs taken and the nutritional status of the patients. However, when chronic diseases were selectively examined, hypertension and depression were found to be associated with a poor nutrition status. The proportion of individuals diagnosed with depression or hypertension was higher in the group of individuals with a risk of malnutrition or malnutrition. Depression is often manifested by changes in eating behavior and weight loss in geriatric populations or geriatric institutions in the community. Physical weakness, which is associated with loss of appetite, personal care, apathy, and depression, may also contribute to malnutrition in older adults [
22].
In this study, it was observed that the patients with malnutrition or malnutrition risk were older than those with a normal nutrition status; moreover, their appetite was worse, dental loss was more frequent, chewing/swallowing difficulty was more frequent, skipping meals was more frequent, and they had less regular physical activity.
Anorexia of aging, an important factor related to malnutrition and malnutrition risk, was significantly associated with a poor nutritional status in our study. According to a study in the USA, 21.8% of individuals (average age 74.5 years) responded that they had a poor appetite. A poor appetite is an important independent predictor of low macro- and micronutrient intakes and is associated with the low dietary quality and decrease in food diversity consumed by older adults [
27].
During the aging process, increased disease prevalence, oral and dental health problems, chewing and swallowing function problems, and social difficulties in obtaining food affect food intake quality and quantity. In Sweden, a study by Hägglund
et al. [
28] reported that 63% of 391 participants (mean age 84 years) had swallowing dysfunctions, and 23% were malnourished. According to a logistic regression analysis, there is increased risk of malnutrition among elderly people with abnormal swallowing capacity [
28]. Patients in geriatric outpatient clinics should be screened routinely on their nutritional status to determine those who need nutritional support and to apply effective nutrition interventions. In order to reduce the risk of malnutrition, all elderly patients should be questioned about oral and dental health, and appropriate guidance should be given.
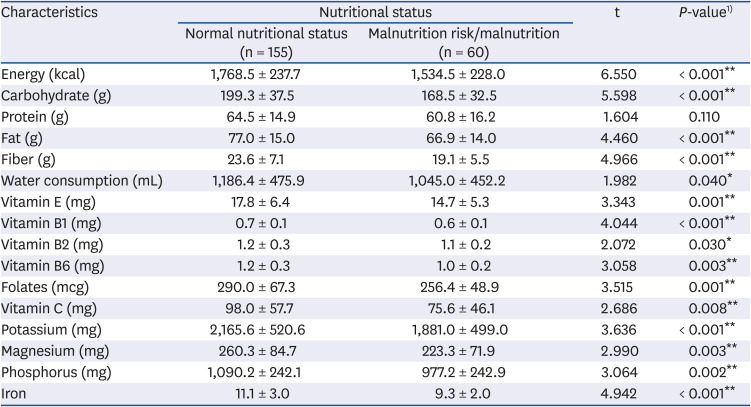
In our study, food consumption records of the patients were obtained via a daily recall method. Moreover, a food catalog was used to facilitate a patient's recall so that detailed information could be obtained. According to the results of our analysis, daily energy, carbohydrate, fat, fiber, vitamin B1, vitamin B6, vitamin C, folate, potassium, magnesium, phosphorus, and iron intake averages and water consumption levels were significantly lower in patients with malnutrition or malnutrition risk than in patients with a normal nutrition status. These observations indicate the importance of these factors on the development of malnutrition risk and malnutrition. In another study, data from 5 nutrition-related studies of elderly individuals living in Finland were combined (n = 900), and individuals with malnutrition (mean age 85 years) or malnutrition risk (mean age 82.4 years) exhibited insufficient daily energy, protein, carbohydrate, fiber, fat, vitamins B1, C, E, A, D, folate, calcium, iron, and zinc intakes compared to those in individuals with normal nutritional status (average age 78.5 years); moreover, the differences were statistically significant [
29].
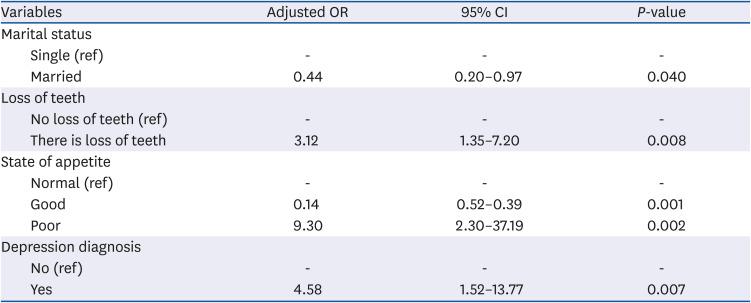
The results of our regression analysis revealed that malnutrition risk was associated with loss of teeth, being single, appetite status, and a depression diagnosis. In another study in Turkey, an age > 84 years, a low BMI, low educational background, presence of comorbidities, and high scores on depression tests were factors that were independently related to malnutrition [
17]. According to another study in Lithuania, malnutrition risk and malnutrition are related to increased age, low economic status, being single, living alone, chronic and intermittent pain, chewing difficulties, swallowing disorders, dental problems, and drug use [
21]. A study in Lebanon showed that a high number of chronic diseases, bad oral and dental health, depressive disorders, higher BMI values, and disability were variables that were significantly associated with a malnutrition status [
18]. However, in a study in Assam, India, the relationships between nutritional status, increased age, female sex, loss of appetite, chewing and swallowing difficulty, dependent functional status, inadequate financial status, and daily caloric intake were found to be significant [
19]. According to a study in the West Bengal region of India, females were significantly more malnourished than males [
30]. Being older, having a lower income, a lower level of literacy, a reduced food intake, or a low food consumption level were independently associated with a low MNA score [
30]. In a study conducted Hirose
et al. [
31], the nutritional status of Japan elderly individuals living in the community and in nursing homes (n = 1,098, mean age 81.2 years) was screened by applying the MNA-short form, and malnutrition was detected in 21.4% of the individuals. Malnutrition and individuals with malnutrition risk had more difficulty in swallowing, loss of appetite, cognitive impairment, mobility disorder, and falling history compared to those in normal nutritional status individuals, and statistically significant differences were detected (
P < 0.001) [
31]. In addition, patients whose nutritional status is deemed “good” (63.3%) have more hypertension frequency compared to those with malnutrition (43.3%), and a statistically significant difference was found [
31]. Researchers in Sri Lanka found that increasing age, hypertension, and alcohol consumption were positively related to the presence of malnutrition [
20]. Similar results were obtained in our study, with hypertension present in 74.8% of individuals with good nutritional status and in 60% of individuals with malnutrition, a statistically significant difference.
One of the main strengths of the study is the relatively large sample size of elderly adults living in urban areas of Turkey. This study also evaluated a wide range of sociodemographic, health and nutrition behavior, and functional status factors that could have a potentially adverse effect on nutritional status.
Some limitations of our study should be taken into consideration while interpreting our results. First of all, the study included subjects from only one center, a university geriatric outpatient clinic in Istanbul. Secondly, except for anthropometric measurements, all data were self-reported and subjective. As a consequence, the generalizability of our results may be limited; however, they highlight the importance of determining malnutrition risk and malnutrition status in elderly patients.
A basic strategy for keeping elderly adults healthy is to prevent chronic diseases and decrease various related complications, including malnutrition. Nutrition is a complex issue that can affect the incidence and the progression of chronic diseases, as well, it has an important role in the quality of life. The elderly are particularly sensitive to malnutrition when they have chronic mental or physical diseases. Therefore, they should be screened for malnutrition risk, and, based on the results of this study, an appropriate care plan should be developed. If nutritional deficiencies cannot be diagnosed and treated in a timely manner, the self-sufficiency of a patient can deteriorate, increasing the need for institutionalization, treatment costs, and the risk of death. In order to maintain and improve the functional status of the elderly, efforts should be undertaken to help them adopt healthy eating and lifestyle practices.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download