1. Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, Whitehead WE, Dumitrascu DL, Fang X, Fukudo S, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of rome foundation global study. Gastroenterology. 2021; 160:99–114.e3. PMID:
32294476.

2. Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology. 2016; 150:1262–1279.

3. Lacy BE, Mearin F, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel disorders. Gastroenterology. 2016; 150:1393–1407.E5.

4. Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, Mareya SM, Shaw AL, Bortey E, Forbes WP. TARGET Study Group. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011; 364:22–32. PMID:
21208106.

5. Lembo A, Pimentel M, Rao SS, Schoenfeld P, Cash B, Weinstock LB, Paterson C, Bortey E, Forbes WP. Repeat treatment with rifaximin is safe and effective in patients with diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2016; 151:1113–1121. PMID:
27528177.

6. Ponziani FR, Zocco MA, D'Aversa F, Pompili M, Gasbarrini A. Eubiotic properties of rifaximin: disruption of the traditional concepts in gut microbiota modulation. World J Gastroenterol. 2017; 23:4491–4499. PMID:
28740337.

7. Mazzawi T, Lied GA, Sangnes DA, El-Salhy M, Hov JR, Gilja OH, Hatlebakk JG, Hausken T. The kinetics of gut microbial community composition in patients with irritable bowel syndrome following fecal microbiota transplantation. PLoS One. 2018; 13:e0194904. PMID:
30427836.

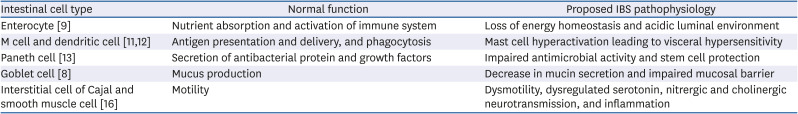
8. Soderholm AT, Pedicord VA. Intestinal epithelial cells: at the interface of the microbiota and mucosal immunity. Immunology. 2019; 158:267–280. PMID:
31509239.

9. Mowat AM, Agace WW. Regional specialization within the intestinal immune system. Nat Rev Immunol. 2014; 14:667–685. PMID:
25234148.

10. Ratanasirintrawoot S, Israsena N. Stem cells in the intestine: possible roles in pathogenesis of irritable bowel syndrome. J Neurogastroenterol Motil. 2016; 22:367–382. PMID:
27184041.

11. O'Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006; 7:688–693. PMID:
16819463.
12. Li M, Zhang L, Lu B, Chen Z, Chu L, Meng L, Fan Y. Role of dendritic cell-mediated abnormal immune response in visceral hypersensitivity. Int J Clin Exp Med. 2015; 8:13243–13250. PMID:
26550249.
13. Zhou C, Fang X, Xu J, Gao J, Zhang L, Zhao J, Meng Y, Zhou W, Han X, Bai Y, et al.
Bifidobacterium longum alleviates irritable bowel syndrome-related visceral hypersensitivity and microbiota dysbiosis via Paneth cell regulation. Gut Microbes. 2020; 12:1782156. PMID:
32584650.
14. Vincent AD, Wang XY, Parsons SP, Khan WI, Huizinga JD. Abnormal absorptive colonic motor activity in germ-free mice is rectified by butyrate, an effect possibly mediated by mucosal serotonin. Am J Physiol Gastrointest Liver Physiol. 2018; 315:G896–907. PMID:
30095295.

15. Geremia A, Biancheri P, Allan P, Corazza GR, Di Sabatino A. Innate and adaptive immunity in inflammatory bowel disease. Autoimmun Rev. 2014; 13:3–10. PMID:
23774107.

16. Eshraghian A, Eshraghian H. Interstitial cells of Cajal: a novel hypothesis for the pathophysiology of irritable bowel syndrome. Can J Gastroenterol. 2011; 25:277–279. PMID:
21647464.

17. El-Salhy M, Hausken T, Gilja OH, Hatlebakk JG. The possible role of gastrointestinal endocrine cells in the pathophysiology of irritable bowel syndrome. Expert Rev Gastroenterol Hepatol. 2017; 11:139–148. PMID:
27927062.

18. Chong PP, Chin VK, Looi CY, Wong WF, Madhavan P, Yong VC. The microbiome and irritable bowel syndrome - A review on the pathophysiology, current research and future therapy. Front Microbiol. 2019; 10:1136. PMID:
31244784.

19. Davenport ER, Sanders JG, Song SJ, Amato KR, Clark AG, Knight R. The human microbiome in evolution. BMC Biol. 2017; 15:127. PMID:
29282061.

20. Scarpellini E, Ianiro G, Attili F, Bassanelli C, De Santis A, Gasbarrini A. The human gut microbiota and virome: potential therapeutic implications. Dig Liver Dis. 2015; 47:1007–1012. PMID:
26257129.

21. Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007; 449:804–810. PMID:
17943116.

22. Rinninella E, Raoul P, Cintoni M, Franceschi F, Miggiano GA, Gasbarrini A, Mele MC. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms. 2019; 7:14.

23. Jeffery IB, O'Toole PW, Öhman L, Claesson MJ, Deane J, Quigley EM, Simrén M. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. 2012; 61:997–1006. PMID:
22180058.

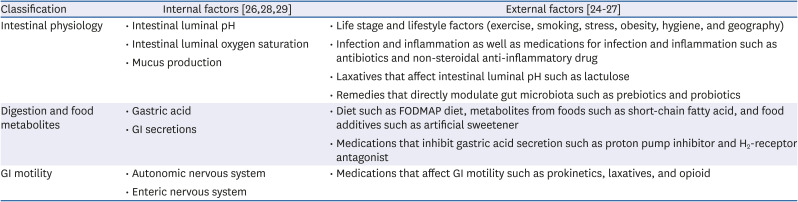
24. Dominguez-Bello MG, Blaser MJ, Ley RE, Knight R. Development of the human gastrointestinal microbiota and insights from high-throughput sequencing. Gastroenterology. 2011; 140:1713–1719. PMID:
21530737.

25. Conlon MA, Bird AR. The impact of diet and lifestyle on gut microbiota and human health. Nutrients. 2014; 7:17–44. PMID:
25545101.

26. Simrén M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG; Rome Foundation Committee. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013; 62:159–176. PMID:
22730468.

27. Tuddenham S, Sears CL. The intestinal microbiome and health. Curr Opin Infect Dis. 2015; 28:464–470. PMID:
26237547.

28. Duncan SH, Louis P, Thomson JM, Flint HJ. The role of pH in determining the species composition of the human colonic microbiota. Environ Microbiol. 2009; 11:2112–2122. PMID:
19397676.

29. Nicholson JK, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W, Pettersson S. Host-gut microbiota metabolic interactions. Science. 2012; 336:1262–1267. PMID:
22674330.

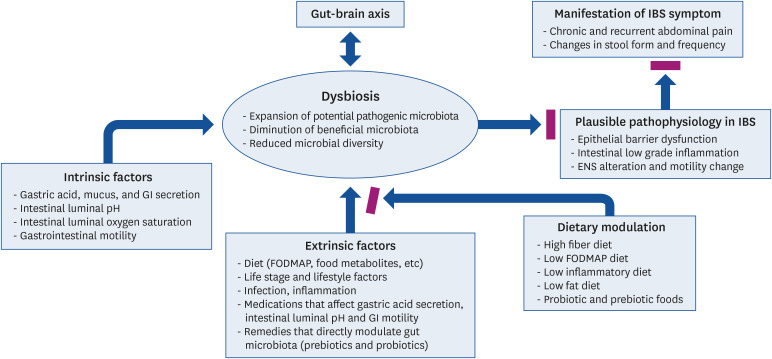
30. Quigley EM. The gut-brain axis and the microbiome: clues to pathophysiology and opportunities for novel management strategies in irritable bowel syndrome (IBS). J Clin Med. 2018; 7:6.

31. van de Wouw M, Schellekens H, Dinan TG, Cryan JF. Microbiota-gut-brain axis: modulator of host metabolism and appetite. J Nutr. 2017; 147:727–745. PMID:
28356427.

32. Fung C, Vanden Berghe P. Functional circuits and signal processing in the enteric nervous system. Cell Mol Life Sci. 2020; 77:4505–4522. PMID:
32424438.

33. Bhattarai Y, Muniz Pedrogo DA, Kashyap PC. Irritable bowel syndrome: a gut microbiota-related disorder? Am J Physiol Gastrointest Liver Physiol. 2017; 312:G52–62. PMID:
27881403.

34. Agus A, Planchais J, Sokol H. Gut microbiota regulation of tryptophan metabolism in health and disease. Cell Host Microbe. 2018; 23:716–724. PMID:
29902437.

35. Gao K, Mu CL, Farzi A, Zhu WY. Tryptophan metabolism: a link between the gut microbiota and brain. Adv Nutr. 2020; 11:709–723. PMID:
31825083.

36. Yano JM, Yu K, Donaldson GP, Shastri GG, Ann P, Ma L, Nagler CR, Ismagilov RF, Mazmanian SK, Hsiao EY. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015; 161:264–276. PMID:
25860609.

37. De Vadder F, Grasset E, Mannerås Holm L, Karsenty G, Macpherson AJ, Olofsson LE, Bäckhed F. Gut microbiota regulates maturation of the adult enteric nervous system via enteric serotonin networks. Proc Natl Acad Sci U S A. 2018; 115:6458–6463. PMID:
29866843.

38. Berstad A, Raa J, Valeur J. Tryptophan: ‘essential’ for the pathogenesis of irritable bowel syndrome? Scand J Gastroenterol. 2014; 49:1493–1498. PMID:
25000845.

39. Bosi A, Banfi D, Bistoletti M, Giaroni C, Baj A. Tryptophan metabolites along the microbiota-gut-brain axis: an interkingdom communication system influencing the gut in health and disease. Int J Tryptophan Res. 2020; 13:1178646920928984. PMID:
32577079.

40. Zelante T, Iannitti RG, Cunha C, De Luca A, Giovannini G, Pieraccini G, Zecchi R, D'Angelo C, Massi-Benedetti C, Fallarino F, et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity. 2013; 39:372–385. PMID:
23973224.

41. O'Mahony SM, Clarke G, Borre YE, Dinan TG, Cryan JF. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res. 2015; 277:32–48. PMID:
25078296.
42. Williams BB, Van Benschoten AH, Cimermancic P, Donia MS, Zimmermann M, Taketani M, Ishihara A, Kashyap PC, Fraser JS, Fischbach MA. Discovery and characterization of gut microbiota decarboxylases that can produce the neurotransmitter tryptamine. Cell Host Microbe. 2014; 16:495–503. PMID:
25263219.

43. Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E. Dysbiosis and the immune system. Nat Rev Immunol. 2017; 17:219–232. PMID:
28260787.

44. Petersen C, Round JL. Defining dysbiosis and its influence on host immunity and disease. Cell Microbiol. 2014; 16:1024–1033. PMID:
24798552.

45. Bellini M, Gambaccini D, Stasi C, Urbano MT, Marchi S, Usai-Satta P. Irritable bowel syndrome: a disease still searching for pathogenesis, diagnosis and therapy. World J Gastroenterol. 2014; 20:8807–8820. PMID:
25083055.
46. Tap J, Derrien M, Törnblom H, Brazeilles R, Cools-Portier S, Doré J, Störsrud S, Le Nevé B, Öhman L, Simrén M. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology. 2017; 152:111–123.e8. PMID:
27725146.

47. Schmidt TS, Raes J, Bork P. The human gut microbiome: from association to modulation. Cell. 2018; 172:1198–1215. PMID:
29522742.

48. Hyland NP, Cryan JF. Microbe-host interactions: influence of the gut microbiota on the enteric nervous system. Dev Biol. 2016; 417:182–187. PMID:
27343895.

49. Pittayanon R, Lau JT, Yuan Y, Leontiadis GI, Tse F, Surette M, Moayyedi P. Gut microbiota in patients with irritable bowel syndrome-A systematic review. Gastroenterology. 2019; 157:97–108. PMID:
30940523.

50. Rodiño-Janeiro BK, Vicario M, Alonso-Cotoner C, Pascua-García R, Santos J. A Review of microbiota and irritable bowel syndrome: future in therapies. Adv Ther. 2018; 35:289–310. PMID:
29498019.

51. Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto JM, Kennedy S, et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013; 500:541–546. PMID:
23985870.

52. Merino VR, Nakano V, Liu C, Song Y, Finegold SM, Avila-Campos MJ. Quantitative detection of enterotoxigenic Bacteroides fragilis subtypes isolated from children with and without diarrhea. J Clin Microbiol. 2011; 49:416–418. PMID:
20980581.

53. Distrutti E, Monaldi L, Ricci P, Fiorucci S. Gut microbiota role in irritable bowel syndrome: new therapeutic strategies. World J Gastroenterol. 2016; 22:2219–2241. PMID:
26900286.

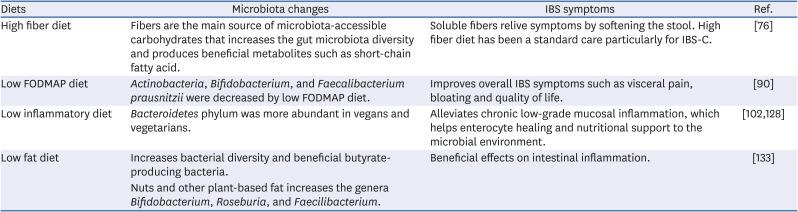
54. David LA, Maurice CF, Carmody RN, Gootenberg DB, Button JE, Wolfe BE, Ling AV, Devlin AS, Varma Y, Fischbach MA, et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014; 505:559–563. PMID:
24336217.

55. Muegge BD, Kuczynski J, Knights D, Clemente JC, González A, Fontana L, Henrissat B, Knight R, Gordon JI. Diet drives convergence in gut microbiome functions across mammalian phylogeny and within humans. Science. 2011; 332:970–974. PMID:
21596990.

56. Chey WD. Food: the main course to wellness and illness in patients with irritable bowel syndrome. Am J Gastroenterol. 2016; 111:366–371. PMID:
26856749.

57. Chey WD, Whelan K. Dietary guidelines for irritable bowel syndrome are important for gastroenterologists, dietitians and people with irritable bowel syndrome. J Hum Nutr Diet. 2016; 29:547–548. PMID:
27599641.

58. Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012; 486:207–214. PMID:
22699609.
59. Conlon MA, Bird AR, Clarke JM, Le Leu RK, Christophersen CT, Lockett TJ, Topping DL. Lowering of large bowel butyrate levels in healthy populations is unlikely to be beneficial. J Nutr. 2015; 145:1030–1031. PMID:
25934666.

60. Madsen KL. Interactions between microbes and the gut epithelium. J Clin Gastroenterol. 2011; 45(Suppl):S111–S114. PMID:
21992948.

61. Thursby E, Juge N. Introduction to the human gut microbiota. Biochem J. 2017; 474:1823–1836. PMID:
28512250.

62. McKenzie YA, Bowyer RK, Leach H, Gulia P, Horobin J, O'Sullivan NA, Pettitt C, Reeves LB, Seamark L, Williams M, et al. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016; 29:549–575. PMID:
27272325.

63. Halmos EP, Christophersen CT, Bird AR, Shepherd SJ, Gibson PR, Muir JG. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut. 2015; 64:93–100. PMID:
25016597.

64. Holscher HD. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. 2017; 8:172–184. PMID:
28165863.

65. Ma N, Tian Y, Wu Y, Ma X. Contributions of the interaction between dietary protein and gut microbiota to intestinal health. Curr Protein Pept Sci. 2017; 18:795–808. PMID:
28215168.

66. Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, Abrouk M, Farahnik B, Nakamura M, Zhu TH, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017; 15:73. PMID:
28388917.

67. Tuck CJ, Vanner SJ. Dietary therapies for functional bowel symptoms: Recent advances, challenges, and future directions. Neurogastroenterol Motil. 2018; 30:e13238.

68. Didari T, Mozaffari S, Nikfar S, Abdollahi M. Effectiveness of probiotics in irritable bowel syndrome: updated systematic review with meta-analysis. World J Gastroenterol. 2015; 21:3072–3084. PMID:
25780308.

69. Grabitske HA, Slavin JL. Low-digestible carbohydrates in practice. J Am Diet Assoc. 2008; 108:1677–1681. PMID:
18926133.

70. Murray K, Wilkinson-Smith V, Hoad C, Costigan C, Cox E, Lam C, Marciani L, Gowland P, Spiller RC. Differential effects of FODMAPs (fermentable oligo-, di-, mono-saccharides and polyols) on small and large intestinal contents in healthy subjects shown by MRI. Am J Gastroenterol. 2014; 109:110–119. PMID:
24247211.

71. Mayer EA, Savidge T, Shulman RJ. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014; 146:1500–1512. PMID:
24583088.

72. Macfarlane GT, Macfarlane S. Bacteria, colonic fermentation, and gastrointestinal health. J AOAC Int. 2012; 95:50–60. PMID:
22468341.

73. Farup PG, Rudi K, Hestad K. Faecal short-chain fatty acids - a diagnostic biomarker for irritable bowel syndrome? BMC Gastroenterol. 2016; 16:51. PMID:
27121286.

74. Tana C, Umesaki Y, Imaoka A, Handa T, Kanazawa M, Fukudo S. Altered profiles of intestinal microbiota and organic acids may be the origin of symptoms in irritable bowel syndrome. Neurogastroenterol Motil. 2010; 22:512–519. e114–515. PMID:
19903265.

75. El-Salhy M, Ystad SO, Mazzawi T, Gundersen D. Dietary fiber in irritable bowel syndrome (Review). Int J Mol Med. 2017; 40:607–613. PMID:
28731144.

76. Clevers E, Tran M, Van Oudenhove L, Störsrud S, Böhn L, Törnblom H, Simrén M. Adherence to diet low in fermentable carbohydrates and traditional diet for irritable bowel syndrome. Nutrition. 2020; 73:110719. PMID:
32086111.

77. Rajilić-Stojanović M, Jonkers DM, Salonen A, Hanevik K, Raes J, Jalanka J, de Vos WM, Manichanh C, Golic N, Enck P, et al. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol. 2015; 110:278–287. PMID:
25623659.

78. Muir JG, Gibson PR. The low FODMAP diet for treatment of irritable bowel syndrome and other gastrointestinal disorders. Gastroenterol Hepatol (N Y). 2013; 9:450–452. PMID:
23935555.
79. Shepherd SJ, Parker FC, Muir JG, Gibson PR. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008; 6:765–771. PMID:
18456565.

80. De Giorgio R, Volta U, Gibson PR. Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction? Gut. 2016; 65:169–178. PMID:
26078292.

81. Shepherd SJ, Lomer MC, Gibson PR. Short-chain carbohydrates and functional gastrointestinal disorders. Am J Gastroenterol. 2013; 108:707–717. PMID:
23588241.

82. McIntosh K, Reed DE, Schneider T, Dang F, Keshteli AH, De Palma G, Madsen K, Bercik P, Vanner S. FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut. 2017; 66:1241–1251. PMID:
26976734.

83. Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014; 146:67–75.e5. PMID:
24076059.
84. Austin GL, Dalton CB, Hu Y, Morris CB, Hankins J, Weinland SR, Westman EC, Yancy WS Jr, Drossman DA. A very low-carbohydrate diet improves symptoms and quality of life in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009; 7:706–708.e1. PMID:
19281859.

85. Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006; 106:1631–1639. PMID:
17000196.

86. Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016; 55:897–906. PMID:
25982757.

87. Staudacher HM, Whelan K. The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS. Gut. 2017; 66:1517–1527. PMID:
28592442.

88. Varjú P, Farkas N, Hegyi P, Garami A, Szabó I, Illés A, Solymár M, Vincze Á, Balaskó M, Pár G, et al. Low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet improves symptoms in adults suffering from irritable bowel syndrome (IBS) compared to standard IBS diet: a meta-analysis of clinical studies. PLoS One. 2017; 12:e0182942. PMID:
28806407.

89. Dionne J, Ford AC, Yuan Y, Chey WD, Lacy BE, Saito YA, Quigley EM, Moayyedi P. A systematic review and meta-analysis evaluating the efficacy of a gluten-free diet and a low FODMAPs diet in treating symptoms of irritable bowel syndrome. Am J Gastroenterol. 2018; 113:1290–1300. PMID:
30046155.

90. Hustoft TN, Hausken T, Ystad SO, Valeur J, Brokstad K, Hatlebakk JG, Lied GA. Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2017; 29:e12969.

91. Bellini M, Tonarelli S, Nagy AG, Pancetti A, Costa F, Ricchiuti A, de Bortoli N, Mosca M, Marchi S, Rossi A. Low FODMAP diet: evidence, doubts, and hopes. Nutrients. 2020; 12:148.

92. Staudacher HM, Lomer MC, Anderson JL, Barrett JS, Muir JG, Irving PM, Whelan K. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012; 142:1510–1518. PMID:
22739368.

93. Staudacher HM, Whelan K. Altered gastrointestinal microbiota in irritable bowel syndrome and its modification by diet: probiotics, prebiotics and the low FODMAP diet. Proc Nutr Soc. 2016; 75:306–318. PMID:
26908093.

94. Chumpitazi BP, Hollister EB, Oezguen N, Tsai CM, McMeans AR, Luna RA, Savidge TC, Versalovic J, Shulman RJ. Gut microbiota influences low fermentable substrate diet efficacy in children with irritable bowel syndrome. Gut Microbes. 2014; 5:165–175. PMID:
24637601.

95. Chumpitazi BP, Cope JL, Hollister EB, Tsai CM, McMeans AR, Luna RA, Versalovic J, Shulman RJ. Randomised clinical trial: gut microbiome biomarkers are associated with clinical response to a low FODMAP diet in children with the irritable bowel syndrome. Aliment Pharmacol Ther. 2015; 42:418–427. PMID:
26104013.

96. Daïen CI, Pinget GV, Tan JK, Macia L. Detrimental impact of microbiota-accessible carbohydrate-deprived diet on gut and immune homeostasis: an overview. Front Immunol. 2017; 8:548. PMID:
28553291.

97. Chadwick VS, Chen W, Shu D, Paulus B, Bethwaite P, Tie A, Wilson I. Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology. 2002; 122:1778–1783. PMID:
12055584.

98. O'Sullivan M, Clayton N, Breslin NP, Harman I, Bountra C, McLaren A, O'Morain CA. Increased mast cells in the irritable bowel syndrome. Neurogastroenterol Motil. 2000; 12:449–457. PMID:
11012945.
99. Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004; 126:693–702. PMID:
14988823.

100. Akiho H, Ihara E, Nakamura K. Low-grade inflammation plays a pivotal role in gastrointestinal dysfunction in irritable bowel syndrome. World J Gastrointest Pathophysiol. 2010; 1:97–105. PMID:
21607147.

101. Sinagra E, Pompei G, Tomasello G, Cappello F, Morreale GC, Amvrosiadis G, Rossi F, Lo Monte AI, Rizzo AG, Raimondo D. Inflammation in irritable bowel syndrome: myth or new treatment target? World J Gastroenterol. 2016; 22:2242–2255. PMID:
26900287.

102. El-Salhy M, Gundersen D. Diet in irritable bowel syndrome. Nutr J. 2015; 14:36. PMID:
25880820.

103. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014; 17:1689–1696. PMID:
23941862.

104. Buscail C, Sabate JM, Bouchoucha M, Kesse-Guyot E, Hercberg S, Benamouzig R, Julia C. Western dietary pattern is associated with irritable bowel syndrome in the French NutriNet Cohort. Nutrients. 2017; 9:986.

105. Khayyatzadeh SS, Esmaillzadeh A, Saneei P, Keshteli AH, Adibi P. Dietary patterns and prevalence of irritable bowel syndrome in Iranian adults. Neurogastroenterol Motil. 2016; 28:1921–1933. PMID:
27324285.

106. Calder PC, Ahluwalia N, Brouns F, Buetler T, Clement K, Cunningham K, Esposito K, Jönsson LS, Kolb H, Lansink M, et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br J Nutr. 2011; 106(Suppl 3):S5–S78. PMID:
22133051.

107. Galland L. Diet and inflammation. Nutr Clin Pract. 2010; 25:634–640. PMID:
21139128.

108. Menotti A, Puddu PE. How the seven countries study contributed to the definition and development of the Mediterranean diet concept: a 50-year journey. Nutr Metab Cardiovasc Dis. 2015; 25:245–252. PMID:
25650160.

109. Hidalgo-Mora JJ, García-Vigara A, Sánchez-Sánchez ML, García-Pérez MÁ, Tarín J, Cano A. The Mediterranean diet: a historical perspective on food for health. Maturitas. 2020; 132:65–69. PMID:
31883665.

110. Trichopoulou A, Martínez-González MA, Tong TY, Forouhi NG, Khandelwal S, Prabhakaran D, Mozaffarian D, de Lorgeril M. Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Med. 2014; 12:112. PMID:
25055810.

111. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018; 378:e34. PMID:
29897866.

112. Gambino CM, Accardi G, Aiello A, Candore G, Dara-Guccione G, Mirisola M, Procopio A, Taormina G, Caruso C. Effect of extra virgin olive oil and table olives on the immuneinflammatory responses: potential clinical applications. Endocr Metab Immune Disord Drug Targets. 2018; 18:14–22. PMID:
29141570.

113. Deiana M, Serra G, Corona G. Modulation of intestinal epithelium homeostasis by extra virgin olive oil phenolic compounds. Food Funct. 2018; 9:4085–4099. PMID:
30083682.

114. Farràs M, Martinez-Gili L, Portune K, Arranz S, Frost G, Tondo M, Blanco-Vaca F. Modulation of the gut microbiota by olive oil phenolic compounds: implications for lipid metabolism, immune system, and obesity. Nutrients. 2020; 12:2200.

115. Salas-Salvadó J, Casas-Agustench P, Murphy MM, López-Uriarte P, Bulló M. The effect of nuts on inflammation. Asia Pac J Clin Nutr. 2008; 17(Suppl 1):333–336. PMID:
18296371.
116. Holscher HD, Guetterman HM, Swanson KS, An R, Matthan NR, Lichtenstein AH, Novotny JA, Baer DJ. Walnut consumption alters the gastrointestinal microbiota, microbially derived secondary bile acids, and health markers in healthy adults: a randomized controlled trial. J Nutr. 2018; 148:861–867. PMID:
29726951.

117. Bamberger C, Rossmeier A, Lechner K, Wu L, Waldmann E, Fischer S, Stark RG, Altenhofer J, Henze K, Parhofer KG. A walnut-enriched diet affects gut microbiome in healthy caucasian subjects: a randomized, controlled trial. Nutrients. 2018; 10:244.

118. Zito FP, Polese B, Vozzella L, Gala A, Genovese D, Verlezza V, Medugno F, Santini A, Barrea L, Cargiolli M, et al. Good adherence to mediterranean diet can prevent gastrointestinal symptoms: a survey from Southern Italy. World J Gastrointest Pharmacol Ther. 2016; 7:564–571. PMID:
27867690.

119. Shin PK, Park SJ, Kim MS, Kwon DY, Kim MJ, Kim K, Chun S, Lee HJ, Choi SW. A traditional Korean diet with a low dietary inflammatory index increases anti-inflammatory IL-10 and decreases pro-inflammatory NF-κB in a small dietary intervention study. Nutrients. 2020; 12:2468.

120. Barbalho SM, Goulart RA, Araújo AC, Guiguer ÉL, Bechara MD. Irritable bowel syndrome: a review of the general aspects and the potential role of vitamin D. Expert Rev Gastroenterol Hepatol. 2019; 13:345–359. PMID:
30791775.

121. Jalili M, Vahedi H, Poustchi H, Hekmatdoost A. Effects of vitamin D supplementation in patients with irritable bowel syndrome: a randomized, double-blind, placebo-controlled clinical trial. Int J Prev Med. 2019; 10:16. PMID:
30820303.

122. Khalighi Sikaroudi M, Mokhtare M, Janani L, Faghihi Kashani AH, Masoodi M, Agah S, Abbaspour N, Dehnad A, Shidfar F. Vitamin D3 supplementation in diarrhea-predominant irritable bowel syndrome patients: the effects on symptoms improvement, serum corticotropin-releasing hormone, and interleukin-6 - A randomized clinical trial. Complement Med Res. 2020; 27:302–309. PMID:
32203968.

123. Khalighi Sikaroudi M, Mokhtare M, Shidfar F, Janani L, Faghihi Kashani A, Masoodi M, Agah S, Dehnad A, Shidfar S. Effects of vitamin D3 supplementation on clinical symptoms, quality of life, serum serotonin (5-hydroxytryptamine), 5-hydroxy-indole acetic acid, and ratio of 5-HIAA/5-HT in patients with diarrhea-predominant irritable bowel syndrome: a randomized clinical trial. EXCLI J. 2020; 19:652–667. PMID:
33013260.
124. Shi SM, Wen YL, Hou HB, Liu HX. Effectiveness of vitamin D for irritable bowel syndrome: a protocol for a systematic review of randomized controlled trial. Medicine (Baltimore). 2019; 98:e14723. PMID:
30817618.
125. Ligaarden SC, Farup PG. Low intake of vitamin B6 is associated with irritable bowel syndrome symptoms. Nutr Res. 2011; 31:356–361. PMID:
21636013.

126. Salari-Moghaddam A, Keshteli AH, Esmaillzadeh A, Adibi P. Empirically derived food-based inflammatory potential of the diet, irritable bowel syndrome, and its severity. Nutrition. 2019; 63-64:141–147. PMID:
31029043.

127. Zheng J, Hoffman KL, Chen JS, Shivappa N, Sood A, Browman GJ, Dirba DD, Hanash S, Wei P, Hebert JR, et al. Dietary inflammatory potential in relation to the gut microbiome: results from a cross-sectional study. Br J Nutr. 2020; 124:931–942. PMID:
32475373.

128. De Filippis F, Pellegrini N, Vannini L, Jeffery IB, La Storia A, Laghi L, Serrazanetti DI, Di Cagno R, Ferrocino I, Lazzi C, et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016; 65:1812–1821. PMID:
26416813.

129. Cozma-Petruţ A, Loghin F, Miere D, Dumitraşcu DL. Diet in irritable bowel syndrome: What to recommend, not what to forbid to patients! World J Gastroenterol. 2017; 23:3771–3783. PMID:
28638217.

130. Just S, Mondot S, Ecker J, Wegner K, Rath E, Gau L, Streidl T, Hery-Arnaud G, Schmidt S, Lesker TR, et al. The gut microbiota drives the impact of bile acids and fat source in diet on mouse metabolism. Microbiome. 2018; 6:134. PMID:
30071904.

131. Abulizi N, Quin C, Brown K, Chan YK, Gill SK, Gibson DL. Gut mucosal proteins and bacteriome are shaped by the saturation index of dietary lipids. Nutrients. 2019; 11:418.

132. Shen W, Wolf PG, Carbonero F, Zhong W, Reid T, Gaskins HR, McIntosh MK. Intestinal and systemic inflammatory responses are positively associated with sulfidogenic bacteria abundance in high-fat-fed male C57BL/6J mice. J Nutr. 2014; 144:1181–1187. PMID:
24919690.

133. Muralidharan J, Galiè S, Hernández-Alonso P, Bulló M, Salas-Salvadó J. Plant-based fat, dietary patterns rich in vegetable fat and gut microbiota modulation. Front Nutr. 2019; 6:157. PMID:
31681786.

134. Patrone V, Minuti A, Lizier M, Miragoli F, Lucchini F, Trevisi E, Rossi F, Callegari ML. Differential effects of coconut versus soy oil on gut microbiota composition and predicted metabolic function in adult mice. BMC Genomics. 2018; 19:808. PMID:
30404613.

135. Bailey MA, Holscher HD. Microbiome-mediated effects of the Mediterranean diet on inflammation. Adv Nutr. 2018; 9:193–206. PMID:
29767701.

136. Mani V, Hollis JH, Gabler NK. Dietary oil composition differentially modulates intestinal endotoxin transport and postprandial endotoxemia. Nutr Metab (Lond). 2013; 10:6. PMID:
23305038.

137. Ford AC, Quigley EM, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Moayyedi P. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am J Gastroenterol. 2014; 109:1547–1561. PMID:
25070051.

138. Wilson B, Rossi M, Dimidi E, Whelan K. Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2019; 109:1098–1111. PMID:
30949662.

139. Staudacher HM, Lomer MC, Farquharson FM, Louis P, Fava F, Franciosi E, Scholz M, Tuohy KM, Lindsay JO, Irving PM, et al. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial. Gastroenterology. 2017; 153:936–947. PMID:
28625832.

140. Staudacher HM, Scholz M, Lomer MC, Ralph FS, Irving PM, Lindsay JO, Fava F, Tuohy K, Whelan K. Gut microbiota associations with diet in irritable bowel syndrome and the effect of low FODMAP diet and probiotics. Clin Nutr. 2021; 40:1861–1870. PMID:
33183883.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download