INTRODUCTION
Atrial fibrillation (AF)-associated ischemic stroke poses significantly higher morbidity and mortality than strokes of vascular origin.
1) Cardiac emboli originating from the left atrial appendage (LAA) are common causes of ischemic stroke in patients with AF,
2) and are associated with more severe ischemic stroke and longer transient ischemic attacks (TIAs) than strokes secondary to atherosclerotic cerebrovascular disease.
3) With the increased risk of arterial thromboembolism associated with AF, stroke prevention with oral anticoagulation (OAC) is the cornerstone of AF management.
4) Non-vitamin K antagonist oral anticoagulants (NOACs) are often superior to vitamin K antagonists with respect to efficacy and safety, and exhibit more predictable pharmacodynamics and -kinetics, making them less susceptible to drug and food interactions and eliminating the need for regular blood monitoring.
5) Given the safety issues of indefinite OAC use with either approach, LAA occlusion (LAAO) may be an alternative strategy for prevention of stroke, systemic embolization, bleeding, and death in AF patients taking OACs.
6) Recent studies have reported less disabling and lethal strokes after percutaneous LAAO with the Amplatzer cardiac plug (ACP; Abbott Vascular, St. Paul, MN, USA) or Watchman device (Boston Scientific, Marlborough, MA, USA) than those in patients on warfarin therapy.
7)8)9) However, no comparative data regarding ischemic cerebrovascular event-associated neurological outcomes following percutaneous LAA closure or NOAC treatment are available. This study investigated post-stroke neurological outcomes in non-valvular AF (NVAF) patients treated with LAAO, compared to those treated with NOAC therapy.
DISCUSSION
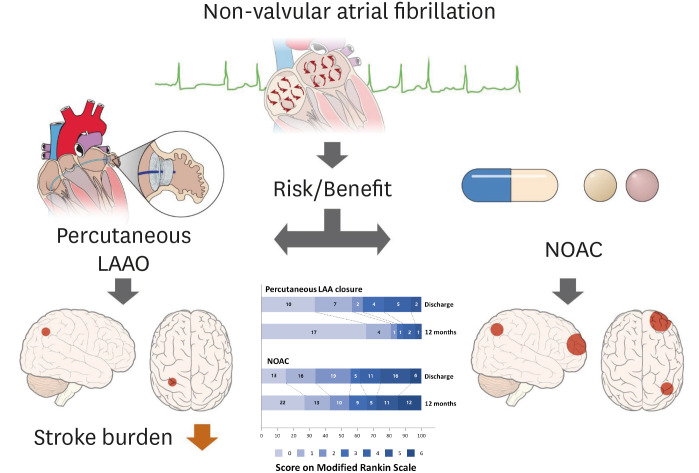
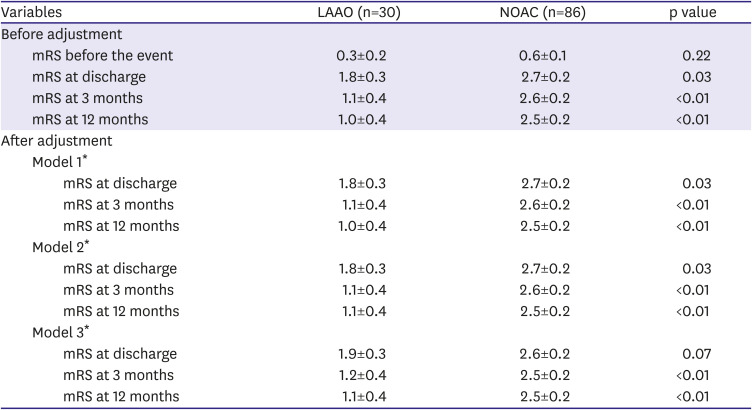
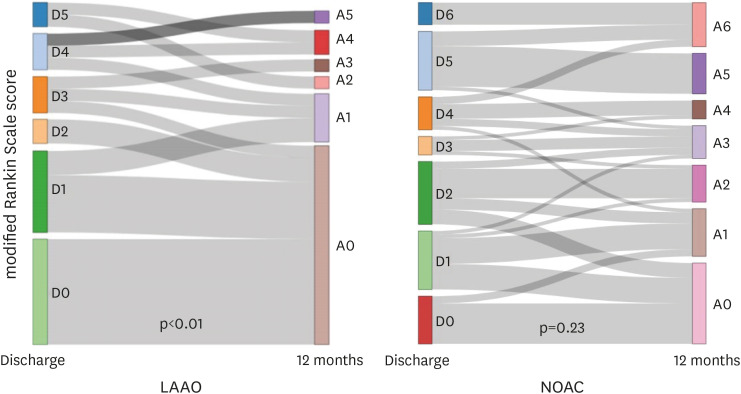
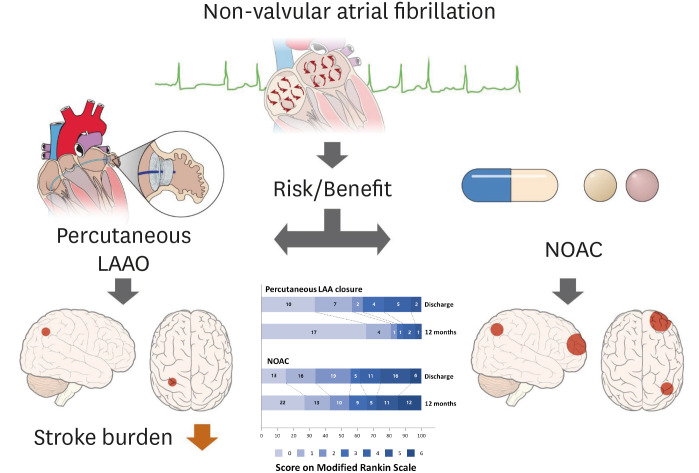
The principal findings of our study are as follows: 1) the frequency of disabling ischemic stroke was lower in NVAF patients treated with LAAO than those treated with NOAC at 3 and 12 months after discharge; 2) recovery rates from disabling ischemic stroke at discharge to 12 months post-stroke were significantly greater in LAAO patients; and 3) mRS scores between discharge and 12 months post-ischemic cerebrovascular events were significantly reduced in the LAAO group. To the best of our knowledge, this is the first clinical study comparing the neurological outcomes of NVAF patients with LAAO and NOAC treatment after ischemic cerebrovascular events, even after excluding hemorrhagic stroke (
Figure 3).
Figure 3
Stroke burden reduction with percutaneous LAAO vs. NOAC treatment.
LAAO = left atrial appendage occlusion; NOAC = non-vitamin K antagonist oral anticoagulant.

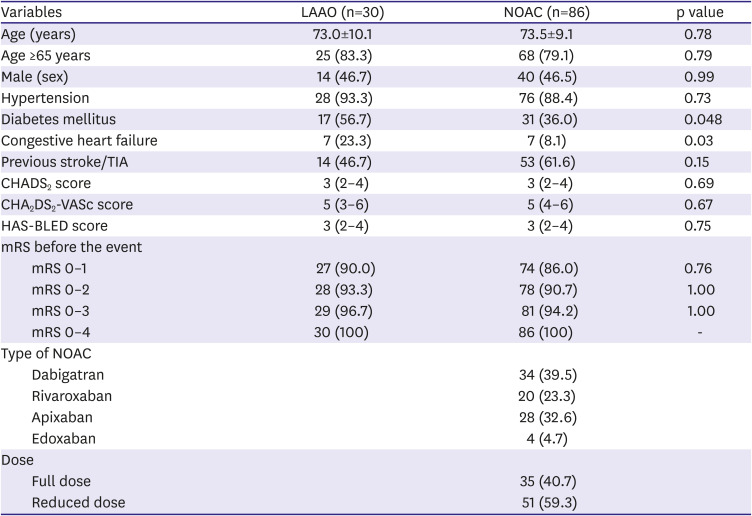
Previous papers have reported less lethal and disabling ischemic stroke after percutaneous LAAO than those treated with warfarin.
7)9) More recently, we reported that NVAF patients previously treated with LAAO experienced more favorable outcomes following ischemic cerebrovascular events than patients taking warfarin.
8) The prevalence of disabling ischemic stroke were 37.5% and 58.8% at discharge (p=0.07), 20.8% and 42.6% at 3 months (p=0.08), and 12.5% and 39.7% at 12 months (p=0.02) in the LAAO and warfarin groups, respectively. The mRS was significantly lower in the LAAO group at discharge, 3 months, and 12 months after ischemic cerebrovascular events (all p<0.01), despite no significant difference in mRS before ischemic cerebrovascular events (p=0.98). Patients in the LAAO group showed a significant reduction in mRS between discharge and 12 months (p<0.01), unlike patients in the warfarin group (p=0.10). Our current study expounded on favorable neurological outcomes of LAAO in patients with ischemic cerebrovascular events in comparison with NOAC treatment.
The incidences of ischemic stroke and TIA events were 1.33% (19 out of 1,427) and 0.77% (11 out of 1,427) in NVAF patients treated with LAAO were markedly low and within acceptable limits, especially considering the higher prevalence of previous cerebrovascular events (46.7%) and a high CHA2DS2-VASc score of 4.7±1.5 in these patients. Similarly, although hemorrhagic stroke was excluded from our formal analysis, the occurrence of intracranial hemorrhage events was low, despite relatively high HAS-BLED scores in our study participants. Thus, the low incidences of ischemic stroke, TIA, and/or hemorrhagic stroke in high-risk patients may be valuable advantages of LAAO over NOAC therapy.
Stroke in AF patients has been extensively associated with higher mortality and greater disability.
1)2) In this study, after excluding LAAO patients with functional disability before the index event, only 2 patients (8.3%) remained disabled at 12 months after discharge, compared to 29 NOAC patients (38.7%). Of these patients, 32.1% (9/28) and 38.5% (30/78) of the patients in the LAAO and NOAC groups, respectively, presented with severe functional disability (mRS >2) at hospital discharge. Moreover, rates of recovery from disabling ischemic stroke at 12 months post-event were significantly higher in the LAAO group (66.7%) than in the NOAC group (7.1%). Significantly reduced mRS scores between hospital discharge and 12 months post-stroke were also seen in LAAO patients, but not in NOAC patients. These findings corroborate those of the PROTECT-AF trial,
15) which reported disabling ischemic stroke in 31% (8/26) of patients after LAAO and in 55% (11/20) of patients after warfarin treatment with relatively low CHA
2DS
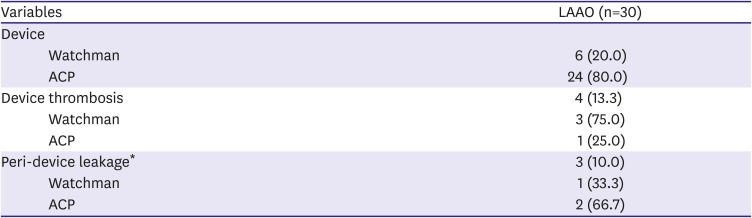
2-VASc scores. However, some differences between the PROTECT-AF study and the current study must be considered: Unlike the PROTECT-AF study, our study showed a lower rate of disabling ischemic stroke in LAAO, compared to anti-coagulant treatment only, from ischemic stroke and TIA, even after excluding hemorrhagic stroke, since hemorrhagic stroke is known to be more prevalent in anticoagulant treatment including NOAC. Secondly, the PROTECT-AF study used only the Watchman device for stroke prevention, while we included both the Watchman and ACP devices. However, the mRS scores post-stroke were not significantly different between the devices in our study, even after adjusting for multiple potential risk factors.
The favorable neurological outcomes we observed in LAAO patients may be explained in several ways. Stroke severity in NVAF could be affected by the patient characteristics of age, risk stratification, stroke mechanism, or prior antithrombotic medication status. In this study, there were no differences in age and, CHADS
2 or CHA
2DS
2-VASc scores between patients with LAAO and those with NOAC, which implies that the different neurological outcomes did not result from different baseline characteristics. Instead, compared to NOAC, LAAO could more effectively prevent thrombus formation within the heart, as most strokes in NVAF patients are caused by thrombi that originate from LAA and as severe stroke is related to larger thrombi in LAA.
2) In a previous study, LAA closure was associated with an improvement in LA mechanical function,
16) a powerful predictor of major cardiovascular events.
17) In this regard, the neurological outcomes may have been better in patients who were treated with LAAO than by NOAC. LAAO has another benefit over anticoagulation in the setting of hemorrhagic complications following cerebral infarction in that it does not impact hemorrhagic transformation; therefore, anticoagulants would likely lead to more favorable neurological outcomes. Although OAC therapy can prevent the formation of intracardiac thrombi, its efficacy may be insufficient in patients with higher CHA
2DS
2-VASc scores or previous history of stroke
18) On the contrary, the benefit of LAAO was greater in patients with higher CHA
2DS
2-VASc scores or those with previous history of stroke.
19) In addition, the clinical net benefit of LAAO can be more prominent over 9 months after the procedure.
20) Our study population had high CHA
2DS
2-VASc scores or higher proportion of previous stroke, and patients in LAAO group were followed up for more than 20 months. These factors could have led to more favorable outcomes for LAAO in our study.
Some limitations of our study should be noted. First, this is a retrospective, non-randomized, observational study that included a small number of patients, even from 3 multi-center registries. Therefore, there were some limitations in collecting detailed information of baseline characteristics, as well as comparing outcomes according to different devices and specific NOACs or different doses of NOACs. Additionally, the incidences of stroke in these registries for both groups were remarkably low because of possible incomplete reporting of stroke. Nevertheless, this is the first clinical study reporting the neurological outcomes of NVAF patients after treatment with LAAO devices, compared with NOAC therapy. Second, recurrent vascular events or hemorrhagic strokes were not analyzed in this study. Third, one should consider the different ethnicities between the LAAO group and NOAC groups. Fourth, although the degree or types of rehabilitation treatment could be associated with a patient's outcome, stroke patients included in this analysis received rehabilitation treatment in various centers, and we did not adjust the impact of rehabilitation, which could be another limitation in this study. Sixth, we did not compare the infarct size (area or volume in neuroimaging study), but we focused on comparing the functional neurological outcome through mRS and proportion of disabling ischemic stroke. Finally, in the current study, there was no imaging core lab for the acquisition and analysis of images. However, as a manner of multi-center registry, the analysis of echocardiographic images was performed by imaging specialists at each participating center, and all assessments of images were conducted following the generally recommended protocol.
10)
In conclusion, percutaneous LAAO yielded favorable neurological outcomes, compared with NOAC, in patients who experienced ischemic cerebrovascular events. These findings suggest an increased neurological benefit of LAAO over NOAC use for long-term protection against thrombus formation in NVAF patients, including those at higher risk of cardio- and cerebrovascular events.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download