INTRODUCTION
Hypertension (HTN) is a widely prevalent condition worldwide.
1) In 2015, one out of four men and five women had elevated blood pressure (BP), according to the World Health Organization (WHO). Uncontrolled high BP increases the risk of stroke, cardiovascular disease, and renal dysfunction.
2) In a large-scale pooled cohort study of Asians, HTN was an important risk factor for stroke and ischemic heart disease.
3) Significant evidence has emerged on the benefits of early intervention and proper management for certain non-communicable diseases, including HTN.
4)5) However, most hypertensive patients are asymptomatic, so that the awareness rate is often far below 50%.
6) There is an urgent need for relevant action to increase awareness of HTN by ‘Knowing one's BP.’
May Measurement Month (MMM) is an initiative of the International Society of Hypertension (ISH), with a primary goal of improving HTN awareness by measuring BP in millions of people worldwide.
7) In its first year in 2017, MMM screened over 1.2 million people in 80 countries globally, revealing over 100,000 people with HTN who were not on treatment and over 150,000 people on antihypertensive treatment who were not controlled.
8) From 2019, the Korean Society of Hypertension (KSH) actively responded to ISH's call and led the project as a name of MMM 2019 Korea. Here we report the results of MMM 2019 Korea.
RESULTS
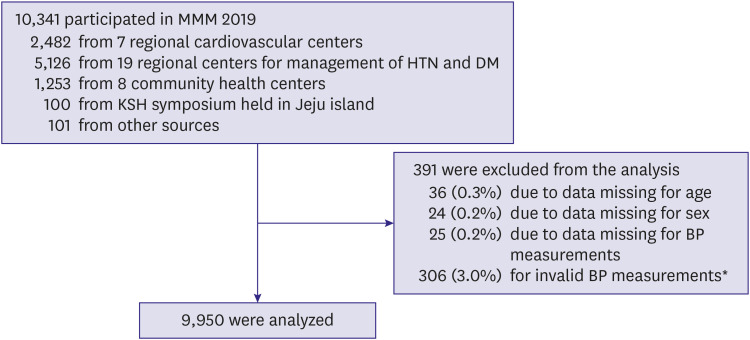
In May of 2019, the MMM campaign was held at 25 community health centers under the Seoul Metropolitan Government, 19 regional centers for the management of HTN and DM under the KDCA, and 7 national regional cardiocerebrovascular centers. Additionally, the Seoul Metropolitan Government conducted a 7-day BP measurement campaign from the first to the last week of May. A street campaign was held at Seoul City Hall Plaza. Through these efforts, we acquired data on 10,341 participants and 13,092 BP measurements (
Figure 1).
Figure 1
Flow chart of MMM 2019 Korea analysis.
HTN = hypertension; BP = blood pressure; DM = diabetes mellitus; HTN = hypertension; KSH = Korean Society of Hypertension; MMM = May Measurement Month.
*Only systolic or diastolic values available, values in single digits, systolic BP higher than diastolic BP.
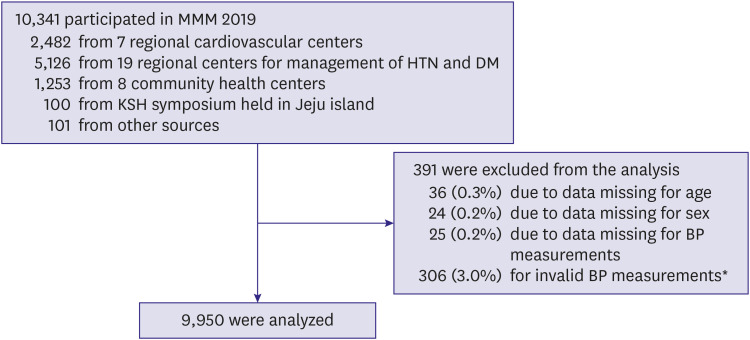

Among total participants, data was missing in 0.3% for age, 0.2% for sex, and 0.2% for BP values. After cleansing, data on 9,950 participants were used for analyses (
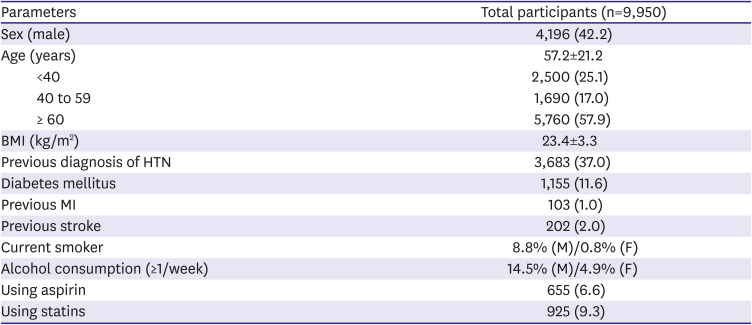
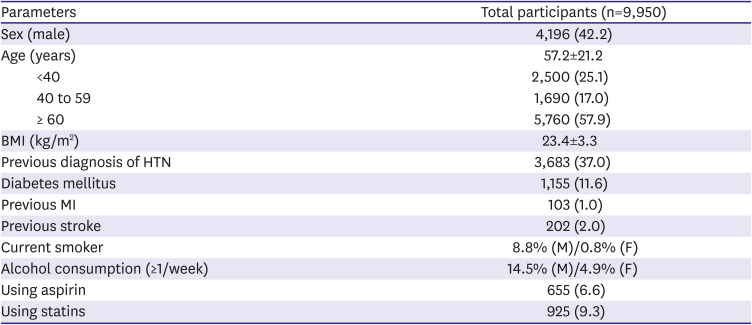
Figure 1). All participants were Korean in ethnicity, the mean age was 57.2 ± 21.2 years, and 57.8% were females. Of the 9,950 participants with valid data, 3,683 (37.0%) reported a previous diagnosis of HTN, and 91.3% (3,365/3,683) of those diagnosed were using antihypertensive medications. The mean body mass index was 23.4 ± 3.3 kg/m
2. The proportion of current smokers was 4.2% (8.8% in men and 0.8% in women), and 8.9% of the population (14.5% in men and 4.9% in women) answered to consume alcohol ≥1/week. For other comorbidities, 1,155 (11.6%) reported having DM, 202 (2.0%) reported a history of the previous stroke, 103 (1.0%) reported an episode of prior MI, and 655 (6.6%) and 925 (9.3%) of participants were taking aspirin and statins, respectively (
Table 1).
Table 1
Baseline characteristics of MMM 2019 Korea
|
Parameters |
Total participants (n=9,950) |
|
Sex (male) |
4,196 (42.2) |
|
Age (years) |
57.2±21.2 |
|
<40 |
2,500 (25.1) |
|
40 to 59 |
1,690 (17.0) |
|
≥ 60 |
5,760 (57.9) |
|
BMI (kg/m2) |
23.4±3.3 |
|
Previous diagnosis of HTN |
3,683 (37.0) |
|
Diabetes mellitus |
1,155 (11.6) |
|
Previous MI |
103 (1.0) |
|
Previous stroke |
202 (2.0) |
|
Current smoker |
8.8% (M)/0.8% (F) |
|
Alcohol consumption (≥1/week) |
14.5% (M)/4.9% (F) |
|
Using aspirin |
655 (6.6) |
|
Using statins |
925 (9.3) |

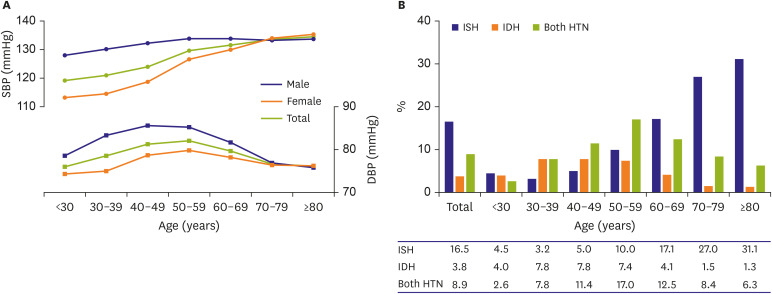
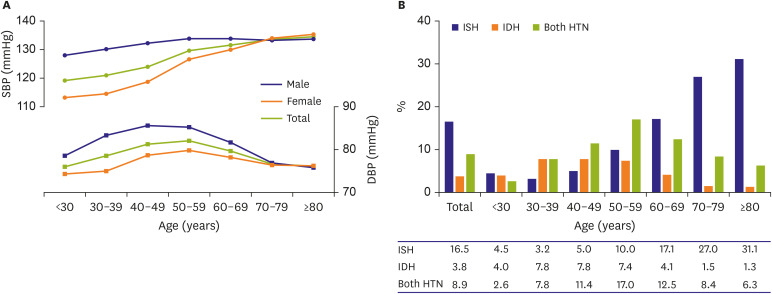
A large proportion of participants (7,102/9,950, 71.4%) underwent BP measurement only once. Mean BPs were 128.8/77.8 mmHg in the whole population, with 132.3/79.5 mmHg in men and 126.2/76.5 mmHg in women (
Supplementary Table 1). Based on these measurements, the prevalence of HTN in the study population was 50.8% (n=5,059), and 29.3% (n=2,911) of 9,950 participants had uncontrolled BP. SBP continuously increased with age, whereas DBP showed an inverted U shape, with the highest levels at ages 50–59. SBP and DBP were higher in men than in women under the age of 80. However, from ages over 50, BP values escalated stiffly in women, therefore there was no gender difference in BP values in elderly population over 70 (
Figure 2A). The crude proportion of patients with HTN increased with age, and there was also a higher proportion of patients with isolated systolic HTN in older age groups (
Figure 2B).
Figure 2
Blood pressures according to age and sex.
(A) Mean systolic and diastolic blood pressure according to age and sex. (B) Prevalence of isolated systolic hypertension and isolated diastolic hypertension according to age group.
DBP = diastolic blood pressure; HTN = hypertension; IDH = isolated diastolic hypertension; ISH = isolated systolic hypertension; SBP, systolic blood pressure.

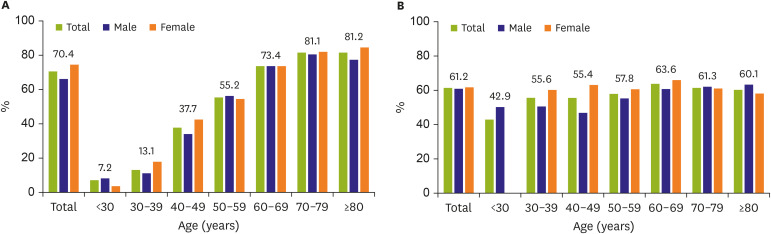
Notably, more than 20% of the participants had not measured their BP during the last 12 months (10.3% never measured BP, 10.6% had no measurements within the past year). The awareness rate in young hypertensive participants was less than 10%, 7.2% (16/223) in participants with ages under 30, and 13.1% (13/99) in the age group of 30 to 39 (
Figure 3A). The treatment rate among those prevalent with HTN was 69.2%, and control rates (1) and (2) were 42.5% and 61.2%, respectively. For those not on any hypertensive medications, the control rate was 51.0% (122/239).
Figure 3
Awareness and control rate of hypertension according to age and sex.
(A) Awareness rate of hypertension according to age and sex. (B) Control rate of hypertension according to age and sex.
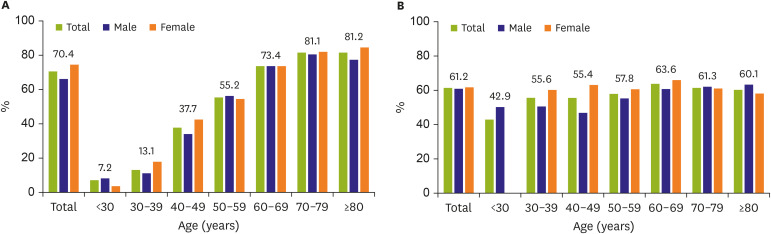

For participants under the age of 40, there was a significant difference in prevalence (23.7% in males vs. 5.5% in females, p<0.001), but no difference was observed in awareness (9.1% vs. 8.6%, p=0.895), treatment (4.1% vs. 7.4%, p=0.243), control rate (1) (2.1% vs. 3.7%, p=0.415), or control rate (2) (50.0% vs. 50.0%, p=1.000) between males and females, respectively. Prevalence, awareness, treatment, and control rates of participants according to age and sex are provided in
Supplementary Table 2 and
Figure 3A, and control rates among those on medications, according to age group, are provided in
Figure 3B.
DISCUSSION
Among the 9,000+ participants recruited in the opportunistic screening program of MMM 2019 Korea, approximately one-third of the enrolled participants had uncontrolled BP. Notably, more than 20% of the participants had not measured their BP during the last 12 months, and the awareness rate in the younger generation under 40 years old was less than 10%.
According to the Korea National Health and Nutrition Examination Survey (KNHANES), a nationally representative population-based survey between 1998 and 2015, the prevalence of HTN in Korean adults has been stable at 30%.
9)10)11) However, although the age-adjusted prevalence rate showed little change between 1998 and 2015, the unadjusted prevalence of HTN had continuously increased, owing to social aging. The rates of awareness, treatment, and control of HTN have shown substantial improvements among hypertensive subjects compared between 1998 and the period of 2007 to 2009. However, the numbers had reached a plateau, and no significant improvements have been observed since 2013.
12) In detail, the awareness of HTN increased from 25% in 1998 to 65% in 2007 but remained at 65% until 2016.
13)14)15) While awareness, treatment, and control of HTN improved remarkably, the young population, particularly men, have shown suboptimal management status.
13)16) This weakness in awareness and control of HTN among the younger population was again demonstrated in MMM 2019 Korea. The awareness rate in young hypertensive participants was less than 10%, 6.3% in participants with ages under 30, and 8.6% in the age group of 30 to 39. This study suggests that even opportunistic screening can identify significant numbers of people with raised BP, especially in the younger generation.
While the prevalence of HTN among young adults has increased, the awareness and treatment rates remained low.
17) According to KNHANES data, in young adults aged 30–39 years, the HTN prevalence has increased from 7.5% to 15.2% from 2007 to 2018, whereas the awareness and the treatment rates have remained at 35.8% and 30.9%, respectively.
5)18) Early detection and management of elevated BP in young adults could prevent future cardiovascular events. In the Coronary Artery Risk Development in Young Adults (CARDIA) study, young adults with above-normal BP levels had a significantly higher risk of subsequent cardiovascular disease than those with normal BP.
19) What is worse, even prehypertensive BP ranges (SBP 130–139 and DBP 80–89 mmHg) were associated with increased risk of subsequent cardiovascular disease events in Korean young adults, compared with normal BP.
20)21) Therefore, more attention needs to be paid to the early diagnosis and treatment of HTN in young adults.
Although MMM 2019 in Korea was highly successful, there are still areas for improvement. First, only 28.6% of patients underwent repeated BP measurements. Previous MMM campaigns have shown that BP values stabilized with repeated measurements, thus increasing the possibility of overestimating BPs in our analyses. Multiple imputations were not used due to the large proportion of missing BP data. Furthermore, to recruit more participants, most campaigns and BP measurements were performed in public places, further leading to the overestimation of BPs.
Additionally, the MMM campaign was an opportunistic event. Thus, random sampling method was not applied in recruitment. As a result, the mean average age of the study population was 57 years, and only a small number of participants under 40 years were recruited. Previously, Kang et al.
9) reported the temporal trends in prevalence and management status of HTN in Korea between 1998 and 2015 based on the KNHANES, a nationally representative population-based survey. The trend, especially the suboptimal management status of HTN among the young population, was consistent with this study, although the awareness and control rates were significantly different. Those differences might come from the difference in gender/age distribution. While the KNHANES has sampled the national represent age/gender distribution, the MMM campaign was an opportunistic event enrolling quite a large population for a single event, and it did not consider balancing age/gender distribution, therefore the values of the awareness, treatment and control rate did not represent national statistics. Although it is well known that the prevalence of HTN increases in the elderly, the participation of younger individuals would also provide valuable data. The KSH has announced the 2020 motto focusing on HTN in the younger generation: 'the earlier, the better' at the beginning of the year.
22)
In conclusion, MMM 2019 Korea campaign reported that one-third of the participants had uncontrolled BP. This screening campaign's benefit is that it identified a higher BP control rate in individuals with HTN. Remarkably, the awareness rate in young hypertensive participants was less than 10%. While awareness, treatment, and control of hypertension have improved remarkably, the younger population, particularly men, showed suboptimal management status. The MMM 2019 Korea again raised the importance of regular BP measurement in the younger population.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download