INTRODUCTION
Emergency departments (EDs) are vital elements of health care systems as they form the national medical safety net that provides emergency care, including diagnostic testing and medical stabilization, for all critically ill patients, regardless of their socioeconomic statuses.
1 However, a substantial proportion of patients require urgent visit to EDs. Thus, the demand exceeds the availability of ED resources and, consequently, inter-hospital transfer (IHT) of patients between EDs occurs frequently.
23 In 2010, in the United States, about 1.5% of the patients in EDs were transferred to other hospitals, and the annual number of patients with transfer admissions increased.
4
Clinically essential transfers for specialty care, such as urgent percutaneous coronary interventions for acute myocardial infarction, are important for improving patient care, but patient preference and convenience are other major reasons behind IHTs.
567 The potential risks of IHT are disruption of care, miscommunication among medical providers, and missing medical information.
78 Given the inherent risks and complex processes, IHTs for ED admission have become a burden to ED physicians, especially in high-level EDs.
910
Many previous studies have demonstrated that patients who are transferred show worse outcomes, incur higher medical costs, and require higher medical resource utilization than those who are not transferred.
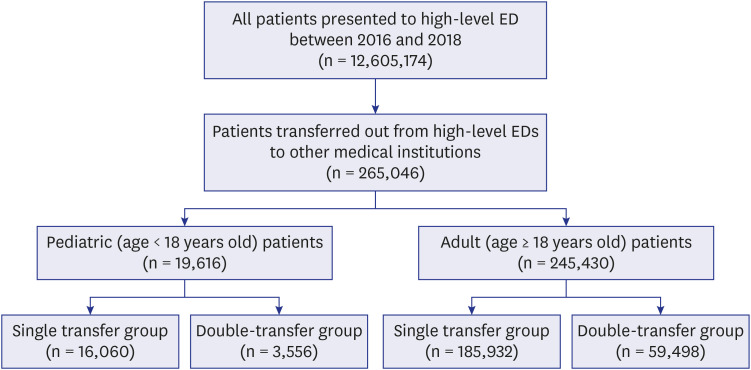
78111213 New strategies are needed to reduce the number of potentially avoidable IHTs and improve the emergency care system. Understanding the characteristics of patients who have undergone IHT is critical for designing effective strategies, especially in cases of double-transfer, i.e., transfer from a medical facility and retransfer to another medical facility. However, this subgroup of patients is understudied at the national level. In this study, we aimed to evaluate the prevalence of IHT in the EDs and to compare the characteristics and ED utilization patterns between patients who undergo single and double transfers between high-level EDs in South Korea using a nationwide prospective database system.
DISCUSSION
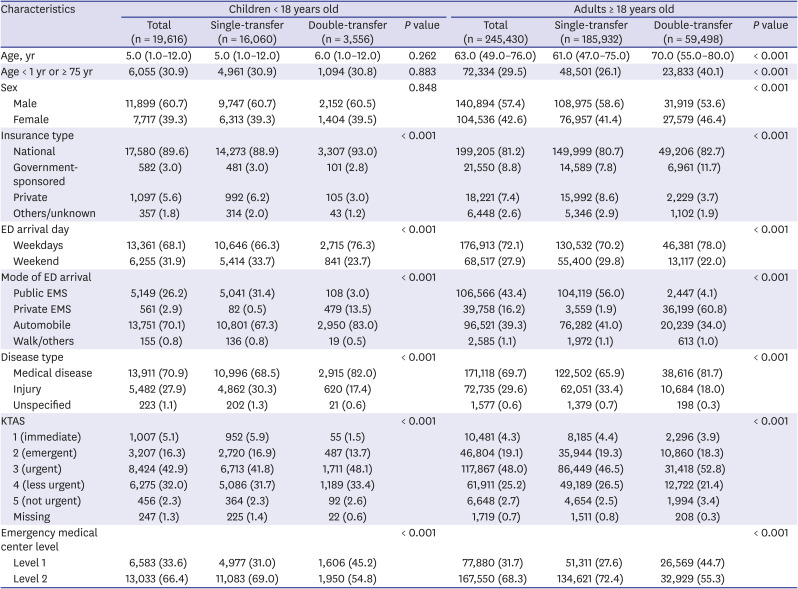
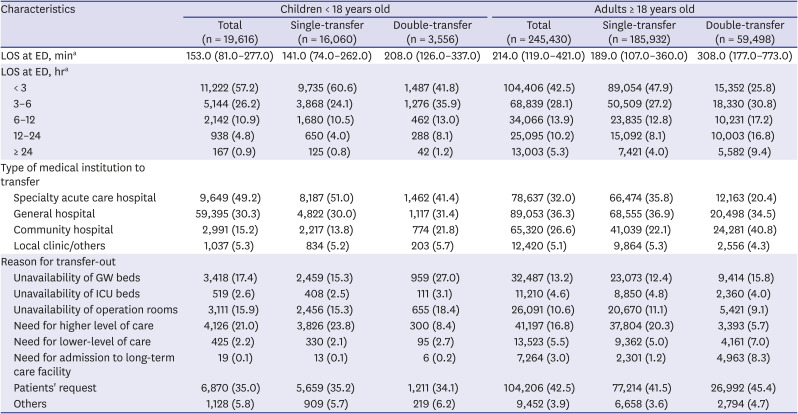
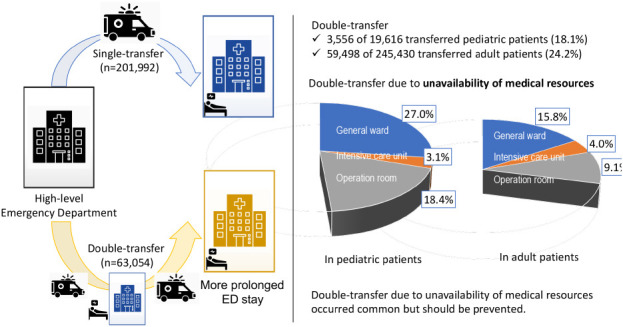
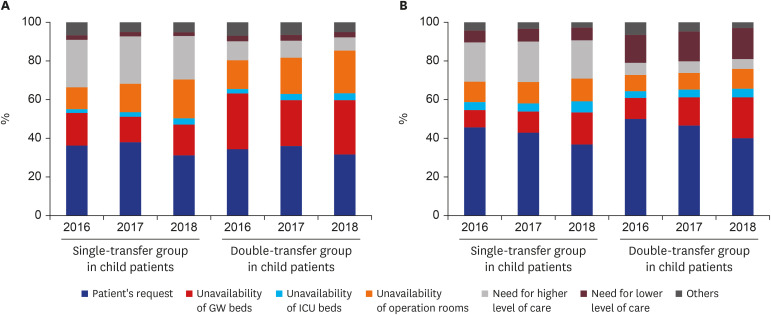
This population-based study in South Korea found that more than 1 in 6 transferred pediatric patients (18.1%) and approximately 1 in 4 transferred adult patients (24.2%) were retransferred from EDs to other EDs. The patients in the double-transfer group stayed in the EDs for long durations, with 1 in 10 pediatric patients (9.3%) and 1 in 4 adult patients (26.2%) staying for more than 12 hours in the ED. Patient request was the most common reason for transfer in both single-transfer and double-transfer groups, but unavailability of medical resources, including general ward beds (pediatric patients, 27.0%; adult patients, 15.8%), ICU beds (pediatric patients, 3.1%; adult patients, 4.0%), and operation rooms (pediatric patients, 18.4%; adult patients, 9.1%), were other common reasons for double transfers. Medical diseases such as cancer-related problems (10.0%) and pneumonia (7.4%) were the top two ED diagnoses in adult patients in the double-transfer group.
ED transfers should be conducted carefully, considering the increased risks and costs. The gaps in communication and coordination during the transfers would lead to treatment delays and even dire consequences. In our study, 2.1% (n = 265,046) of the patients who presented to high-level EDs underwent IHTs, and this figure is nearly similar to the rate of IHTs in the US (1.5–1.8%).
419 However, the double-transfer patients accounted for over 20% of all the transferred patients in our study, and this figure was approximately 10-fold higher than the proportion reported in a previous study about IHT in patients with sepsis and septic shock in the US.
20
Double transfers occurred approximately 1.5-fold more frequently than single transfers in Level 1 EDs, and the patients in the double-transfer group were usually transferred to lower-level EDs. The data suggest that the patients in the double-transfer group were unnecessarily transferred the second time from EDs in high-level hospitals and that inappropriate transfer decisions were made at the time of the first hospital transfer, which could have been prevented.
20 Additionally, our study demonstrated that patient request was the most common reason for transfer. Although the reason for the transfer could be recorded differently depending on the physician on duty or the hospital's policy, such a high proportion implied that inappropriate decision-making was prevalent.
The transfer of patients in need of specialized services was relatively low in our cohort, accounting for approximately 20% in the single-transfer group and less than 10% in the double-transfer group. Transfer for specialized care for specific medical conditions such as trauma, poisoning, and myocardial infarction is unavoidable, and timely transfer in such medical conditions can improve the outcomes.
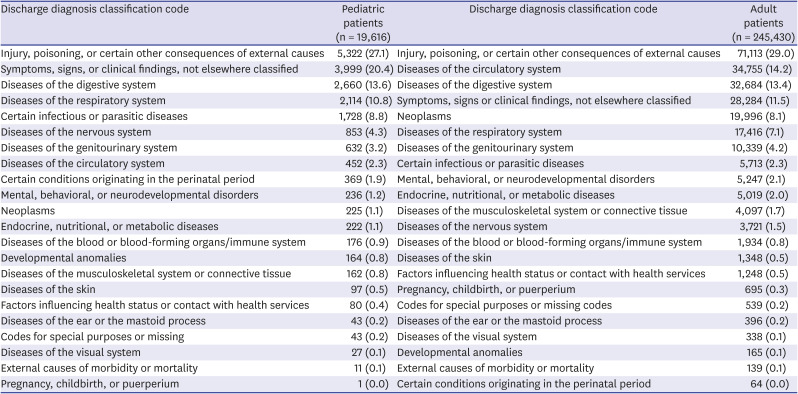
20212223 Consistent with previous studies, injuries and poisonings were the most prevalent ED diagnoses in our study.
2122 Traumatic intracranial hemorrhage, poisoning, and femur fracture were the major diseases in both pediatric and adult patients, but double-transfer occurred more frequently in adult groups. We hypothesized that the involvement of specialized specialists, such as pediatric neurosurgeons, pediatric orthopedic surgeons, and pediatric general surgeons, and the high risk of medical malpractice lawsuits on post-transfer outcomes in pediatric patients enhance the scope for appropriate transfers. Moreover, these patterns implied that the development and establishment of regional networks can improve the transfer practices and, ultimately, the optimization of medical resources.
21
Our study highlights that unavailability of medical resources was the major reason for transfers in the double-transfer group, meaning inappropriate transfers could cause harm in these patients. There should be seamless communication and coordination between the ED physicians who decide to transfer the patients and those who receive the patients to prevent redundant transfers.
9 The low absolute number and proportion of transferred patients, especially those who underwent double transfers among the total patients in the ED suggests that IHT is not an urgent problem, but such transfers can burden not only the ED or emergency medical systems because of potential medical errors and depletion of available resources but also the patients and national insurance systems at large because of increased costs.
21 Therefore, policymakers and planners who design health systems should focus on these subgroups and consider systematic interventions to improve IHT strategies for ED admission.
The NEDIS was established in 2003 to improve the quality of the national emergency medical care system. The NEMC analyzed the NEDIS data, including the status of ED use, the proportion of urgent patients, and their outcome, stratified by regions to establish national and regional emergency medical system implementation plans and to identify the shortcomings of the emergency medical systems. However, some revisions in the NEDIS data-sharing protocol would provide valuable information to emergency physicians, investigators, and policymakers. For instance, the investigators cannot determine the ED use pattern at the patient level. Although the NEDIS collected and managed the information, it did not provide the specific hospital information about where the patient was transferred to or from and about specific procedures such as embolization and endoscopic interventions during the ED stay.
This study has several limitations. First, the NEDIS data did not provide patient's details in a serial order regarding the information of the first medical facilities and post-transfer outcomes. We could not differentiate between the patients who underwent double-transfer and multiple transfers or determine the reason for the first-transfer in the double-transfer group. The possibility of overlap between single- and double-transfer groups should be acknowledged because some patients in the single-transfer group could have been transferred to another hospital, i.e., double-transfer. Furthermore, duplications of cases in the double-transfer group are also possible when they underwent multiple transfers. Moreover, we could not determine whether double-transfer was associated with worse outcomes or higher medical costs than single-transfer. Second, we could not analyze the interventions or procedures in the ED, which could lead to the overestimation of inappropriate transfers, i.e., transfers due to the unavailability of medical resources. For instance, the patients with cancer at long-term care facilities accidentally remove their percutaneous tubes for ascites drainage and are transferred for a reinsertion of the tube. After the tube insertion in the ED, they are retransferred to a long-term care facility. Such cases could contribute to the high proportion of cancer-related problems (10%) in adult patients in the double-transfer group. Third, we used the primary diagnosis code at ED discharge. However, the diagnosis codes do not reflect the severity of the illness and the coding sequences have inter- and intra-rater variability among hospitals and physicians. Finally, our study used the national data of South Korea, and the utilization patterns of EDs vary across countries and healthcare systems. We did not include the patients who presented to Level III local emergency medical institutes owing to missing data. However, the predominant disease in patients who underwent IHTs showed similarities with previous studies from other countries and suggest the generalizability of the characteristics among these patients.
821
In summary, this nationwide cohort study highlights that approximately 1 in 4 patients (23.8%) who were transferred from the ED to other medical facilities underwent double-transfer. Patient's request and unavailability of medical resources were the two most common reasons for transfer. Emergency physicians who would transfer and receive the patients should communicate and coordinate. In addition to the improvement in clinical practices, some specific interventions for transfer decision-making process at EDs, such as enhanced regionalization of specialty care hospitals, standardization of transfer guidelines, and limited telemedicine applications, should also be considered by the committee of emergency physicians and policymakers.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download