|
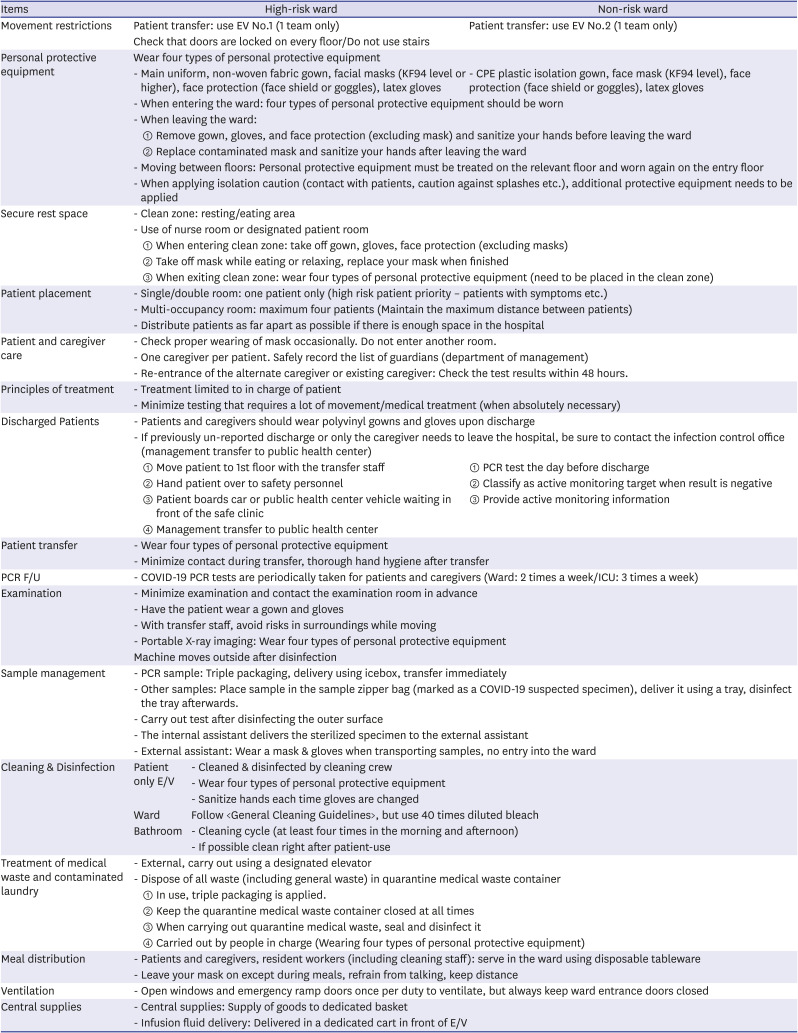
Movement restrictions |
Patient transfer: use EV No.1 (1 team only) |
Patient transfer: use EV No.2 (1 team only) |
|
Check that doors are locked on every floor/Do not use stairs |
|
Personal protective equipment |
Wear four types of personal protective equipment |
|
- Main uniform, non-woven fabric gown, facial masks (KF94 level or higher), face protection (face shield or goggles), latex gloves |
- CPE plastic isolation gown, face mask (KF94 level), face protection (face shield or goggles), latex gloves |
|
- When entering the ward: four types of personal protective equipment should be worn |
|
- When leaving the ward: |
|
① Remove gown, gloves, and face protection (excluding mask) and sanitize your hands before leaving the ward |
|
② Replace contaminated mask and sanitize your hands after leaving the ward |
|
- Moving between floors: Personal protective equipment must be treated on the relevant floor and worn again on the entry floor |
|
- When applying isolation caution (contact with patients, caution against splashes etc.), additional protective equipment needs to be applied |
|
Secure rest space |
- Clean zone: resting/eating area |
|
- Use of nurse room or designated patient room |
|
① When entering clean zone: take off gown, gloves, face protection (excluding masks) |
|
② Take off mask while eating or relaxing, replace your mask when finished |
|
③ When exiting clean zone: wear four types of personal protective equipment (need to be placed in the clean zone) |
|
Patient placement |
- Single/double room: one patient only (high risk patient priority – patients with symptoms etc.) |
|
- Multi-occupancy room: maximum four patients (Maintain the maximum distance between patients) |
|
- Distribute patients as far apart as possible if there is enough space in the hospital |
|
Patient and caregiver care |
- Check proper wearing of mask occasionally. Do not enter another room. |
|
- One caregiver per patient. Safely record the list of guardians (department of management) |
|
- Re-entrance of the alternate caregiver or existing caregiver: Check the test results within 48 hours. |
|
Principles of treatment |
- Treatment limited to in charge of patient |
|
- Minimize testing that requires a lot of movement/medical treatment (when absolutely necessary) |
|
Discharged Patients |
- Patients and caregivers should wear polyvinyl gowns and gloves upon discharge |
|
- If previously un-reported discharge or only the caregiver needs to leave the hospital, be sure to contact the infection control office (management transfer to public health center) |
|
① Move patient to 1st floor with the transfer staff |
① PCR test the day before discharge |
|
② Hand patient over to safety personnel |
② Classify as active monitoring target when result is negative |
|
③ Patient boards car or public health center vehicle waiting in front of the safe clinic |
③ Provide active monitoring information |
|
④ Management transfer to public health center |
|
|
Patient transfer |
- Wear four types of personal protective equipment |
|
- Minimize contact during transfer, thorough hand hygiene after transfer |
|
PCR F/U |
- COVID-19 PCR tests are periodically taken for patients and caregivers (Ward: 2 times a week/ICU: 3 times a week) |
|
Examination |
- Minimize examination and contact the examination room in advance |
|
- Have the patient wear a gown and gloves |
|
- With transfer staff, avoid risks in surroundings while moving |
|
- Portable X-ray imaging: Wear four types of personal protective equipment |
|
Machine moves outside after disinfection |
|
Sample management |
- PCR sample: Triple packaging, delivery using icebox, transfer immediately |
|
- Other samples: Place sample in the sample zipper bag (marked as a COVID-19 suspected specimen), deliver it using a tray, disinfect the tray afterwards. |
|
- Carry out test after disinfecting the outer surface |
|
- The internal assistant delivers the sterilized specimen to the external assistant |
|
- External assistant: Wear a mask & gloves when transporting samples, no entry into the ward |
|
Cleaning & Disinfection |
Patient only E/V |
- Cleaned & disinfected by cleaning crew |
|
- Wear four types of personal protective equipment |
|
- Sanitize hands each time gloves are changed |
|
Ward |
Follow <General Cleaning Guidelines>, but use 40 times diluted bleach |
|
Bathroom |
- Cleaning cycle (at least four times in the morning and afternoon) |
|
- If possible clean right after patient-use |
|
Treatment of medical waste and contaminated laundry |
- External, carry out using a designated elevator |
|
- Dispose of all waste (including general waste) in quarantine medical waste container |
|
① In use, triple packaging is applied. |
|
② Keep the quarantine medical waste container closed at all times |
|
③ When carrying out quarantine medical waste, seal and disinfect it |
|
④ Carried out by people in charge (Wearing four types of personal protective equipment) |
|
Meal distribution |
- Patients and caregivers, resident workers (including cleaning staff): serve in the ward using disposable tableware |
|
- Leave your mask on except during meals, refrain from talking, keep distance |
|
Ventilation |
- Open windows and emergency ramp doors once per duty to ventilate, but always keep ward entrance doors closed |
|
Central supplies |
- Central supplies: Supply of goods to dedicated basket |
|
- Infusion fluid delivery: Delivered in a dedicated cart in front of E/V |









 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download