This article has been
cited by other articles in ScienceCentral.
We thank Lee and Burns for their interest in our review article focused on the invasive physiologic methods for evaluating the appropriateness of percutaneous coronary intervention (PCI).
1) Lee and Burns introduced non-invasive cardiac imaging methods that can be used for detecting residual myocardial ischemia after PCI.
2) While agreeing that these non-invasive cardiac imaging tests can provide important information in patients who underwent PCI, we would like to discuss the strengths and weaknesses of invasive and non-invasive tests for post-PCI patients.
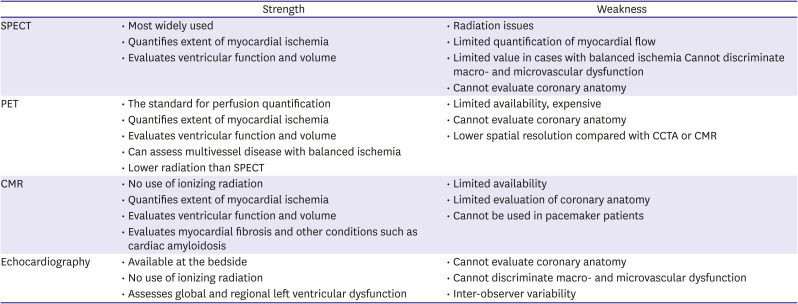
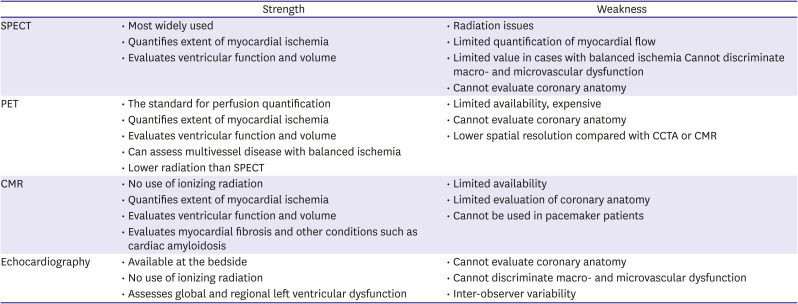
Single-photon emission computed tomography, positron emission tomography, echocardiography, and cardiac magnetic resonance are well-established modalities for coronary artery disease (
Table 1)
3)4)5)6)7) and have been used to evaluate patients with suspected coronary artery disease and guide treatment strategies.
8) The common purpose of these cardiac imaging tests is to identify the presence of myocardial ischemia and can also be used to define residual ischemia after PCI. Previous studies reported that residual ischemia was present after PCI in about one-third of patients from non-invasive imaging tests, and these patients were associated with worse clinical outcomes.
9)10) Therefore, it is important to acknowledge these imaging tests and recognize their collective ability to non-invasively evaluate PCI results by confirming the degree of resolution of ischemia both after PCI and during patient follow-up. However, these non-invasive cardiac imaging tests have limited value in evaluating coronary anatomy and residual anatomical disease severity, including stented segments, and cannot be used in a cardiac catheterization laboratory immediately after PCI. As suboptimal results of PCI, which can originate from stent deployment itself and remaining residual disease, do not always translate to the presence of residual myocardial ischemia, non-invasive cardiac imaging tests have inborn limitations to evaluate the subtle problems after PCI. In contrast to non-invasive cardiac imagings, invasive physiologic assessment can be performed immediately after the procedure, assess the appropriateness of PCI, and reveal the cause of sub-optimal PCI results.
1) Therefore, post-PCI physiologic assessment can detect hidden problems after PCI, even though there is no residual ischemia, thereby allowing physicians to maximize the benefits of PCI in a cardiac catheterization laboratory.
Table 1
Strength and weakness of non-invasive cardiac imaging
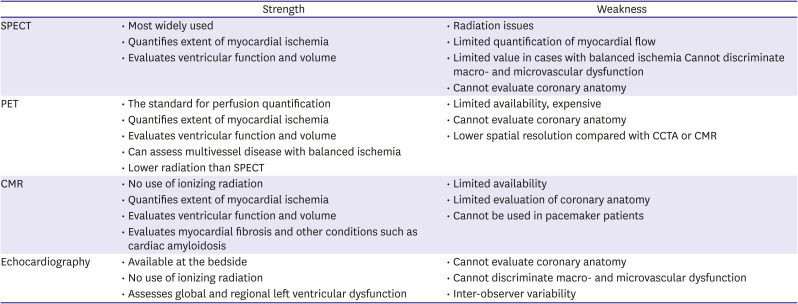
|
Strength |
Weakness |
|
SPECT |
• Most widely used |
• Radiation issues |
|
• Quantifies extent of myocardial ischemia |
• Limited quantification of myocardial flow |
|
• Evaluates ventricular function and volume |
• Limited value in cases with balanced ischemia Cannot discriminate macro- and microvascular dysfunction |
|
• Cannot evaluate coronary anatomy |
|
PET |
• The standard for perfusion quantification |
• Limited availability, expensive |
|
• Quantifies extent of myocardial ischemia |
• Cannot evaluate coronary anatomy |
|
• Evaluates ventricular function and volume |
• Lower spatial resolution compared with CCTA or CMR |
|
• Can assess multivessel disease with balanced ischemia |
|
|
• Lower radiation than SPECT |
|
|
CMR |
• No use of ionizing radiation |
• Limited availability |
|
• Quantifies extent of myocardial ischemia |
• Limited evaluation of coronary anatomy |
|
• Evaluates ventricular function and volume |
• Cannot be used in pacemaker patients |
|
• Evaluates myocardial fibrosis and other conditions such as cardiac amyloidosis |
|
|
Echocardiography |
• Available at the bedside |
• Cannot evaluate coronary anatomy |
|
• No use of ionizing radiation |
• Cannot discriminate macro- and microvascular dysfunction |
|
• Assesses global and regional left ventricular dysfunction |
• Inter-observer variability |