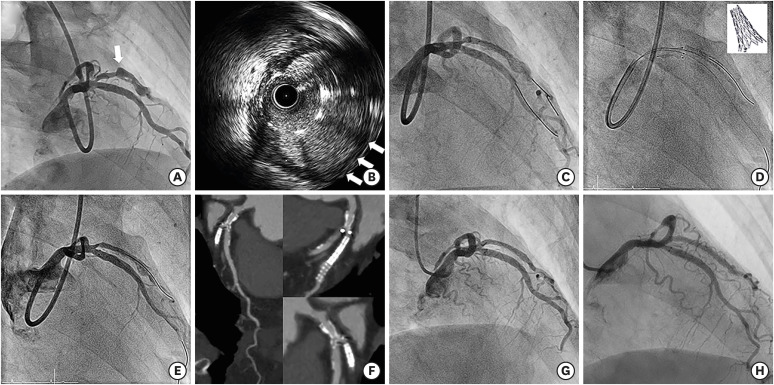
A 56-year-old female was admitted for unstable angina. She had a history of acute myocardial infarction treated with a stent (Cypher 2.5×23 mm) in a diagonal branch (Dx) 5 years ago. As shown in Figure 1, coronary angiography revealed a large thrombotic aneurysmal change at the stent site. There was a true-bifurcation lesion (Medina 0, 1, 1)1) on the left anterior descending artery (LAD) and Dx ostium (Supplementary Videos 1 and 2). Since complicated coronary aneurysms are associated with worse clinical outcomes,2) we decided to treat both the aneurysm and the bifurcation lesions. With a 7-Fr guiding catheter for the left coronary artery, LAD and Dx were crossed with 0.014-inch guidewires. After predilation, intravascular ultrasound was conducted, revealing aneurysmal change from the proximal edge, but not beyond the distal edge, of the stent (Supplementary Video 3). Thus, to cover the aneurysm's entry point, a stent-graft (Graftmaster 2.8×19 mm; Abbott, Abbott Park, IL, USA) was implanted at the proximal portion of the previous stent. Immediate after stent-graft implantation, there was remaining flow to the aneurysm (Supplementary Video 4). However, the aneurysm was completely regressed in a 4-month follow-up computed tomography (Supplementary Video 5). It suggested that covering the aneurysm's entry point strategy could be a promising treatment method for a coronary stent-induced aneurysm. For the true bifurcation, a dedicated bifurcation stent (AXXESS 3.5×11 mm, Biosensors, Singapore) was implanted in the LAD and Dx to avoid carina shifting. The Dx ostium was treated with drug-coated balloon angioplasty. The final angiogram revealed excellent results for the true-bifurcation lesion and the aneurysm (Supplementary Video 6). Two-year and 7-year follow-up angiograms revealed complete regression of aneurysmal change without complications (Supplementary Videos 7 and 8).
Notes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest: Dr. Samady is on Advisory Board for Philips, Abbott Vascular and has had grant funding from Medtronic, Gilead, and NIH. He is equity holder and co-founder of Covanos, and equity holder in SIG. The other authors have no financial conflicts of interest.
Data Sharing Statement: The data required to reproduce these findings cannot be shared since this manuscript contains images of a single patient.
References
1. Lassen JF, Burzotta F, Banning AP, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention. 2018; 13:1540–1553. PMID: 29061550.

2. Alfonso F, Pérez-Vizcayno MJ, Ruiz M, et al. Coronary aneurysms after drug-eluting stent implantation: clinical, angiographic, and intravascular ultrasound findings. J Am Coll Cardiol. 2009; 53:2053–2060. PMID: 19477355.
SUPPLEMENTARY MATERIALS
Supplementary Video 1
A true-bifurcation lesion (Medina 0,1,1) on the left anterior descending artery and ostial of the diagonal branch.
Supplementary Video 2
Different projection of the true-bifurcation lesion at initial coronary angiography.
Supplementary Video 3
Aneurysmal change from the proximal edge, but not beyond the distal edge, of the stent on intravascular ultrasound image.
Figure 1
(A) Coronary angiography revealed a large thrombotic aneurysmal change in the previous stent site with a true-bifurcation lesion (Medina 0, 1, 1) on the left anterior descending artery. A white arrow indicates an aneurysm originating at the proximal edge of the previous stent. (B) Intravascular ultrasound revealed a large aneurysm at the previous stent site (white arrows). (C) A stent-graft was successfully implanted without complication and the flow to aneurysm portion was decreased. (D) The true-bifurcation lesion was treated with a dedicated bifurcation stent. (E) Final angiography revealed successful results. (F) Stent patency was confirmed at the 4-month follow-up coronary computed tomography. Complete regression of the previous large aneurysm was shown at (G) 2-year follow-up, and (H) 7-year follow-up coronary angiography.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download