DISCUSSION
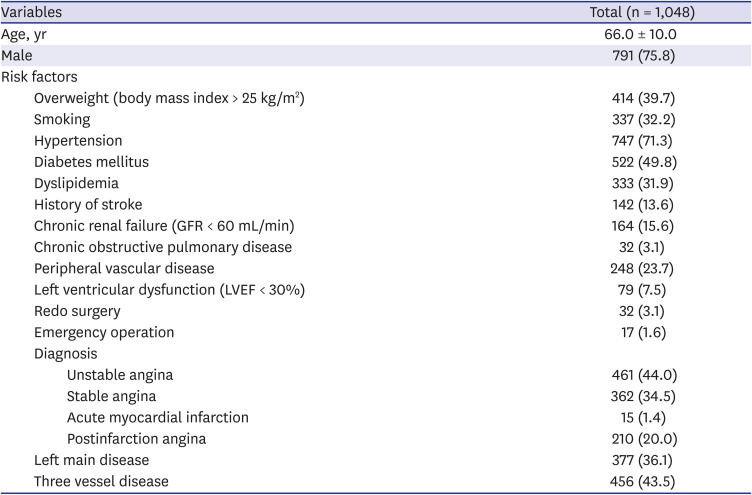
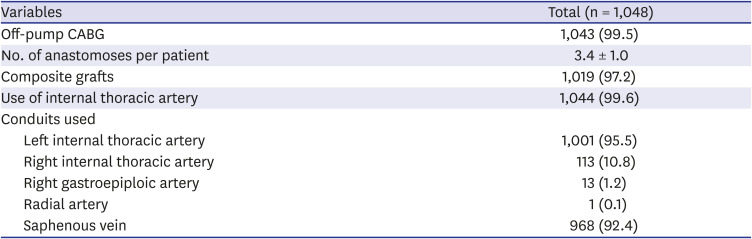
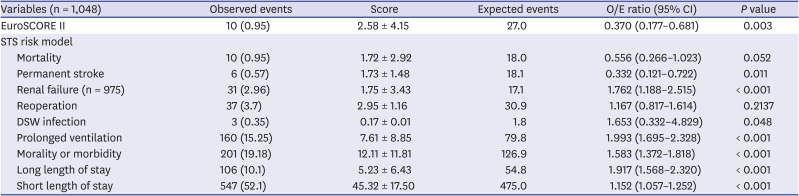
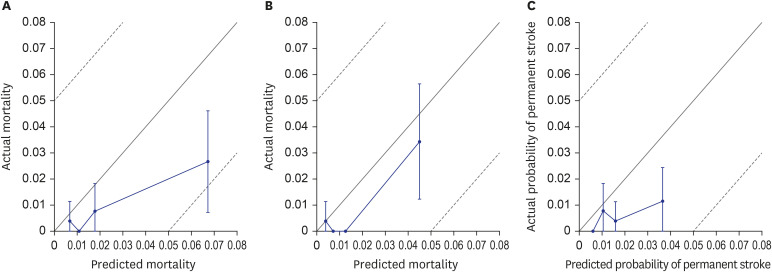
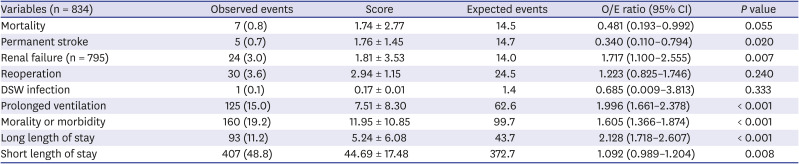
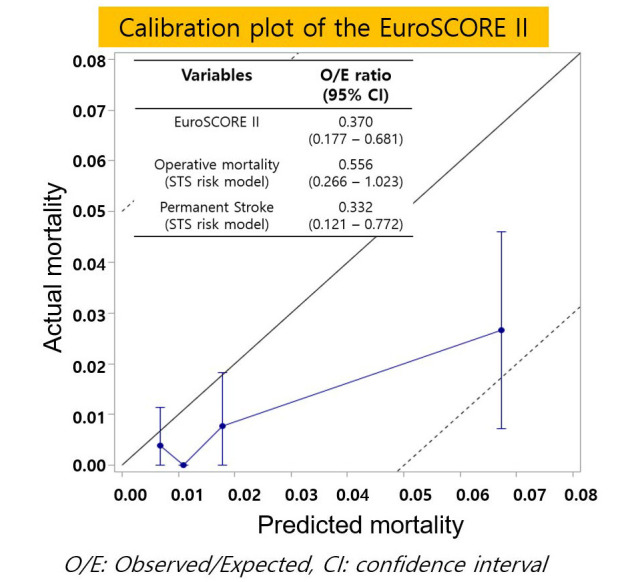
This study reported two main findings. First, preexisting risk prediction scoring systems, the EuroSCORE II and the STS risk model, overpredict the mortality for patients undergoing anaortic OPCAB. Second, the STS risk model overpredicts the occurrence rate of permanent stroke for patients undergoing anaortic OPCAB.
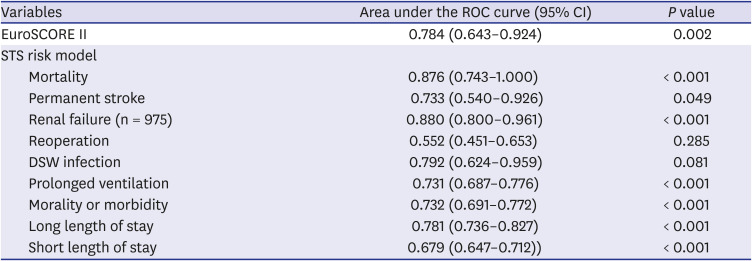
Currently, the EuroSCORE II and STS risk models are widely used risk prediction scoring systems. EuroSCORE II predicts operative mortality after all cardiac surgeries, and the STS risk model predicts 9 early clinical outcomes, including mortality and permanent stroke, after six common cardiac procedures. These two systems showed good calibration and discrimination in the validation data.
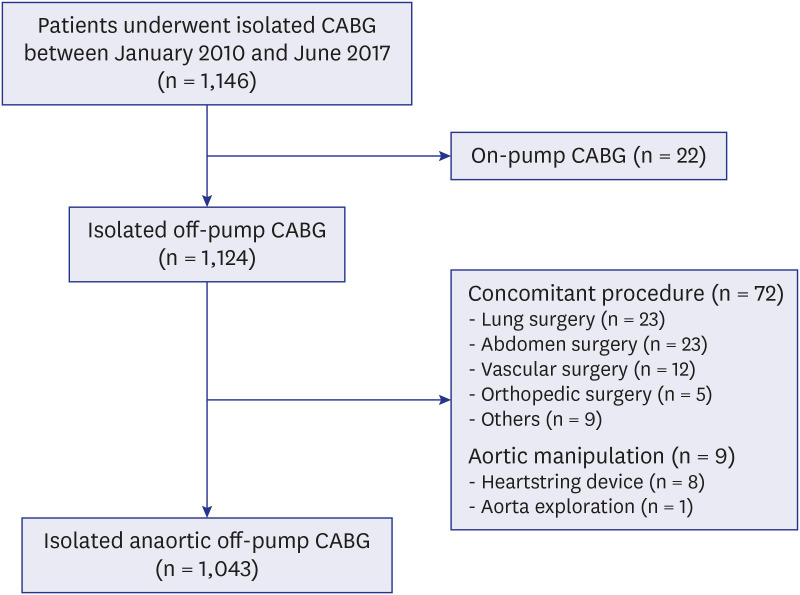
13 However, these risk prediction scoring systems have not been considered to calculate scores for aortic manipulation or used for CPB. Therefore, we evaluated whether the preexisting risk prediction scoring systems can appropriately predict the perioperative risk for patients undergoing anaortic OPCAB.
In this study, the EuroSCORE II and STS risk model (for subgroups) overpredicted the operative mortality for patients undergoing anaortic OPCAB. Although the advantage of OPCAB for mortality remains controversial,
1112 our study showed the possibility that anaortic OPCAB has an advantage in terms of early mortality compared to conventional CABG. These results might be due to anaortic OPCAB being performed by a highly experienced surgeon, reduced occurrence of permanent stroke, and intrinsic features of not using CPB.
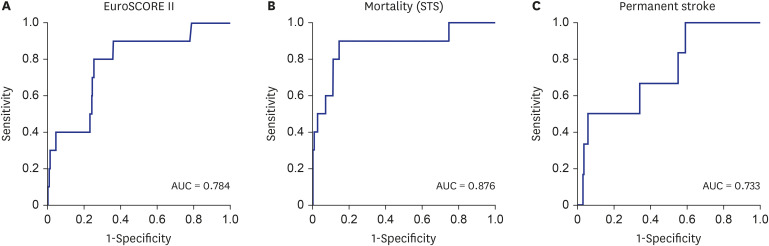
Although the EuroSCORE II and STS risk model overpredicted the operative mortality for patients undergoing anaortic OPCAB, the STS risk model (1.67%) calculated a predicted mortality that was closer to the actual mortality (0.95%) than the EuroSCORE II (2.51%). In addition, the STS risk model showed the better discrimination power for mortality. There are two possible factors that could affect this result. First, the two systems have different model designs. The STS score was developed using patients who only underwent isolated CABG, but the EuroSCORE II was developed using patients who underwent all kinds of cardiac surgery, and the operation type was considered a risk factor. The STS risk model calculated the predicted values based on 65 risk factors, but EuroSCORE II calculated the value based on 18 risk factors. Second, the latest STS risk model was developed for patients who underwent cardiac surgery between July 2011 and June 2014, and EuroSCORE II was developed for patients who underwent cardiac surgery in 2010. These differences may have allowed the STS risk model to calculate a more accurate prediction for operative mortality.
Anaortic OPCAB has theoretical benefits regarding the occurrence of stroke because this technique can prevent damage caused by CPB and aortic manipulation, such as emboli caused by gaseous or fat particles or atherosclerotic embolization.
1314 Some previous studies showed a decrease in the risk of stroke after OPCAB,
1516 and recently, a meta-analysis by Zhao and colleagues
4 showed that anaortic OPCAB could decrease the risk for postoperative stroke, especially in high-risk patients. In this study, the STS risk model significantly overpredicted the occurrence rate of permanent stroke with an O/E ratio of 0.337. This result suggests that anaortic OPCAB could have a protective effect on permanent stroke compared to conventional CABG.
Although the present study suggested that anaortic OPCAB may have advantages in operative mortality and permanent stroke, previous studies demonstrated controversial results.
111217181920 Comparable early results had been shown irrespective of applying cardiopulmonary bypass machine from previous large-scale multicenter studies.
11121718 In addition, similar or favorable 5-year outcomes after on-pump CABG compared with off-pump CABG were recently reported from the CORONARY and ROOBY trial.
1920 However, those previous studies have limitations regarding surgical expertise of attending surgeon,
121718 and have not reported the extent of aortic manipulation and the proportion of an aortic OPCAB.
11121718 In this regard, well designed randomized study comparing the conventional CABG and anaortic OPCAB should be performed.
Unexpectedly, the STS risk model underpredicted the occurrence rate of acute renal failure, prolonged ventilation, and mortality or morbidity. There are some possible explanations for these results. First, our institutional factor could affect the clinical results. Our postoperative protocols included performing early angiography for most of our patients, which might lead to a higher incidence of acute renal failure than the predicted value. Relatively long operation time might be taken as a teaching hospital and could lead a higher incidence of prolonged ventilation. Also, our postoperative strategy of extubation during the next daytime might also affect the prolongation of intubation. Second, the STS risk model for predicting prolonged ventilation is likely inaccurate for Asians. When the latest STS risk model was developed, only 2.8% of patients (12,076/439,092) were Asian people.
3 The Asians included in the model development may not represent the Asians living in Asia since they lived in different lifestyles. Third, the intrinsic features of anaortic OPCAB including volume loading to stabilize the vital signs during posterior vessel revascularization might affect the clinical outcomes. Further studies should be performed to demonstrate the relation between the anaortic OPCAB and acute renal failure or prolonged ventilation.
In terms of hospital stay, the criteria to discriminate short and long stays were different from the definitions of the STS risk model because of the different health insurance systems between the USA and South Korea. The value of 16 days, which is the criterion for long stays, corresponded to the top 75%, and 13 days, which is the criterion for short stays corresponded to the bottom 25%. According to a previous study performed using STS NCD in 2002, 52.5% (260,908/496,797) of patients had a short stay, and 5.2% (26,008/496,797) of patients had a long stay.
21 This means that our criteria using quartiles (bottom 25% and top 75%) for short and long stays may be too low. If the criteria were set similarly to the values of the previous study, the occurrence of short stays would increase, and the occurrence of long stays would decrease. The present study has several limitations. First, the present study was a retrospective observational study from a single institution and it had an institutional factor. And most of the surgeries were performed by a highly experienced surgeon for anaortic OPCAB. Therefore, this could limit the generalization of these results to all surgeons and hospitals. A multicenter study involving many surgeons performing both on-pump and off-pump CABG will be required to evaluate the performance of the preexisting risk models for anaortic OPCAB.
Second, the number of events was too small to evaluate the calibration of the models, especially for deep sternal wound infection, using the Hosmer-Lemeshow test. Therefore, the risk-adjusted ratio was mainly used for the calibration of the models, and there were some differences between the risk-adjusted ratios and Hosmer-Lemeshow tests.
In conclusion, the preexisting risk prediction scoring systems for CABG, the STS risk model and EuroSCORE II, overpredicted the risk of mortality and stroke rate for anaortic OPCAB. These findings suggest the possibility that anaortic OPCAB can lower the operative mortality and occurrence of postoperative stroke than conventional CABG.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download