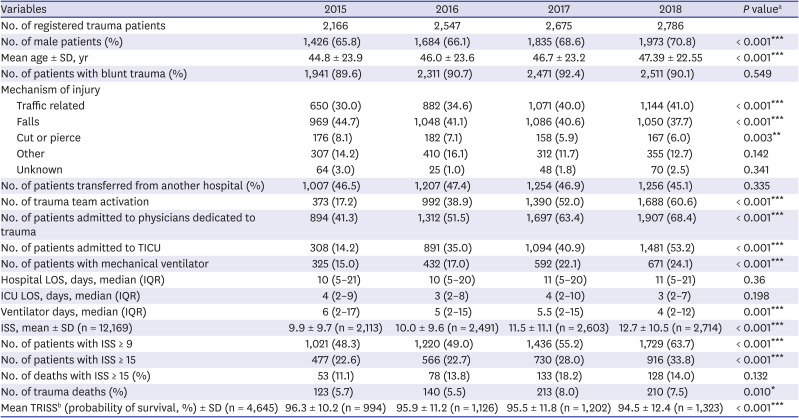
INTRODUCTION
Korea is classified as a high-income country. Nevertheless, its preventable trauma death rate (PTDR) exceeded 30% until the 2010s, and it remains a developing country with regards to the trauma system.
1 The Korean government, therefore, established a plan to design a national trauma system in 2012,
2 with the main goal of establishing 17 trauma centers nationwide. As of 2020, 17 trauma centers have been designated nationwide and 15 have been officially opened and are dedicated to the treatment of trauma patients. These centers are equipped with facilities and equipment with the government's support and receive annual financial support for dedicated personnel.
There have been recent reports on outcomes resulting from performance improvements in trauma care in institutions that opened earlier and have been operating trauma centers for more than 5 years.
34 The most recently published national survey revealed that regional trauma centers had lower PTDRs.
5 Based on these results, it is projected that national trauma outcomes can be improved if the operation of these trauma centers is further established and a system promoting the concentration of severe trauma patients in regional trauma centers is supported.
Since the introduction of trauma centers in Korea 8 years ago, a lack of consensus remains among the trauma centers in terms of operation method and composition of the trauma team for resuscitation. In some trauma centers, trauma patients are still being treated conventionally in the emergency department (ED), and the use of trauma centers remains debatable. In contrast, other trauma centers experience difficulties as the bypass situation continues with an excess of patients. At the time of the establishment of the initial trauma centers, the Korean government and medical community designed guidelines for trauma center implementation, which have been verified by evaluating the introduction of facility equipment and manpower composition. However, the guidelines lack detail and focus solely on early stage implementation. Indeed, detailed evaluation of performance improvement is lacking. Currently, operating trauma centers employ distinct operating methods, and differences exist in the operation methods of trauma teams. Therefore, performance among trauma centers varies. Further, instances of preventable trauma deaths (PTDs) have been reported, leading to social resentment.
67
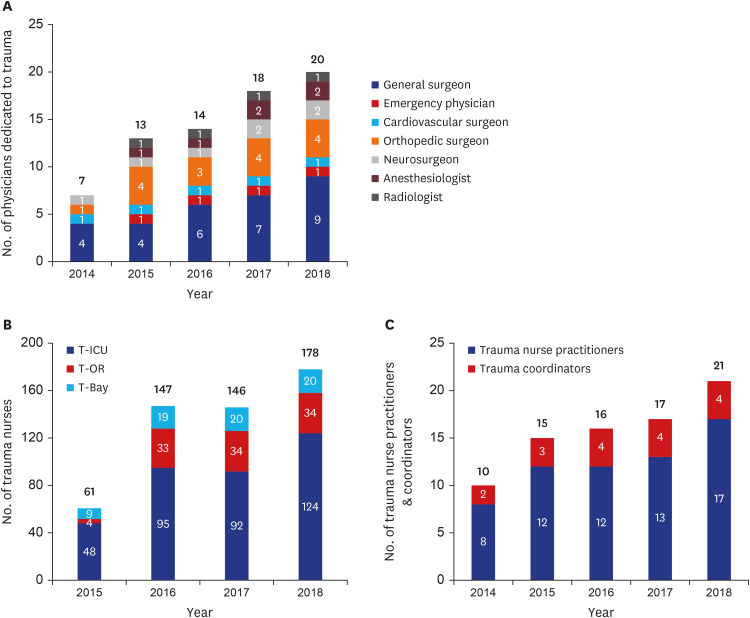
Our trauma center was designated as a regional trauma center in 2013. Following a preparatory process and transitional period, we commenced full operation of the trauma center in 2016. We hired a trauma coordinator, trauma registrar, trauma program manager (TPM), and other relevant personnel. All medical staff were dedicated to trauma patients and received government financial support. The number of beds recruited by dedicated trauma nursing staff was increased to approximate the world standard, working in trauma bays, operating rooms, intensive care units (ICUs), and general wards. In consultation with the government, these facilities received partial financial support. Substantial effort was made to benchmark a level I trauma center in terms of the composition and operation of the trauma team. Surgeons were recruited in a timely manner to provide definitive care to trauma patients. Since its establishment, we have implemented performance improvement activities by selecting audit filters from the American College of Surgeons Committee on Trauma (ACSCOT) and World Health Organization (WHO) Trauma Quality Improvement Program (TQIP) guidelines
89 in addition to the guidelines suggested by the Korean Ministry of Health and Welfare, in accordance with the operating standards and guidelines of the US level I trauma center. This study aimed to review our performance improvement activities and outcomes relative to performance improvement plans of domestic trauma centers, which may still employ controversial operational methods.
Go to :

Methods
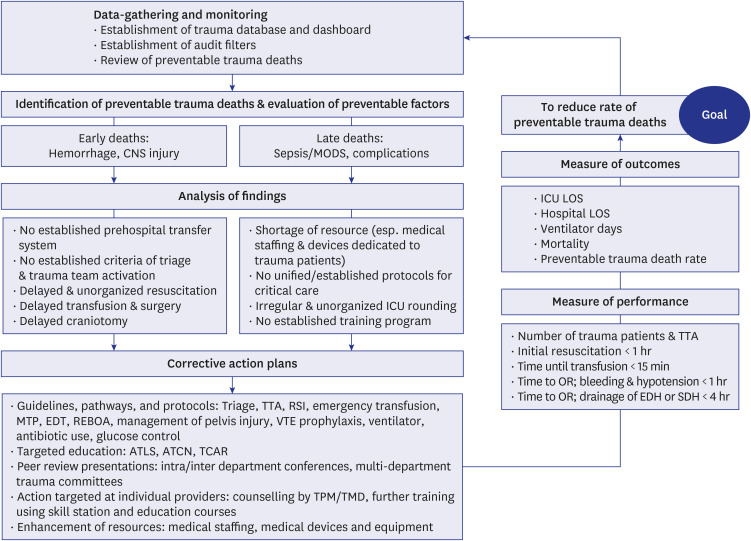
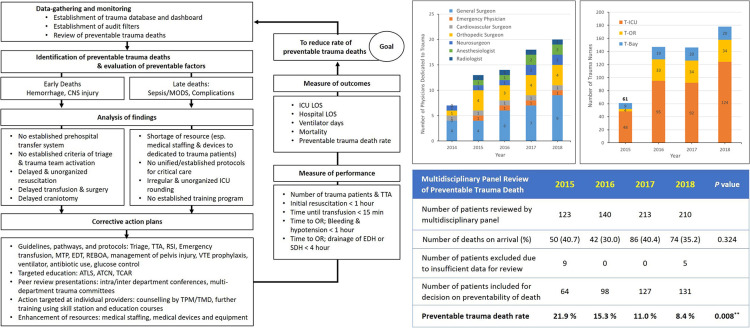
Corrective strategies for performance improvement (“closing the loop”)
We established strategies for performance improvement and patient safety (PIPS) from 2015 when the establishment of the trauma center was in full operation. As described by the ACSCOT and WHO TQIP guidelines,
89 the following corrective strategies were established and proceeded according to the loop closure principle, which is the basis of performance improvement activities (
Fig. 1).
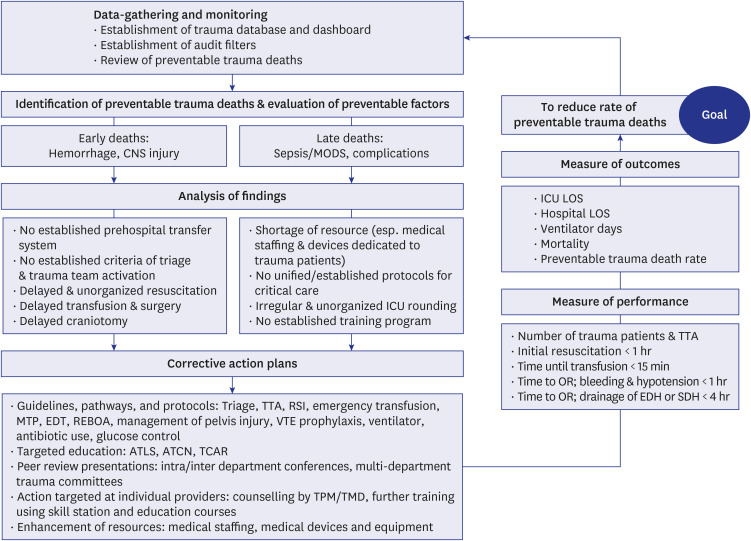 | Fig. 1
Flow chart outlining components of our PIPS program initiated in 2015 and study design according to principles of “closing the loop.”
PIPS = performance improvement and patient safety, CNS = central nervous system, MODS = multiple organ dysfunction syndrome, ICU = intensive care unit, TTA = trauma team activation, RSI = rapid sequence intubation, MTP = massive transfusion protocol, EDT = emergency department thoracotomy, REBOA = resuscitative endovascular balloon occlusion of the aorta, VTE = venous thromboembolism, ATLS = Advanced Trauma Life Support, ATCN = Advanced Trauma Care for Nurses, TCAR = Trauma Care After Resuscitation, TPM = trauma program manager, TMD = trauma medical director, LOS = length of stay, OR = operation room, EDH = epidural hemorrhage, SDH = subdural hemorrhage.

|
Data-gathering and monitoring
We first recruited trauma coordinators and data registrars to collect, register, and monitor data. We established a trauma database based on the Korea Trauma Data Bank (KTDB) dictionary (benchmarked from NTDB) and added “dashboards” for checking the audit filters that originated based on our own needs. The majority of these PIPS programs were computerized to enable in-depth analysis and sharing of the results by all members concurrently.
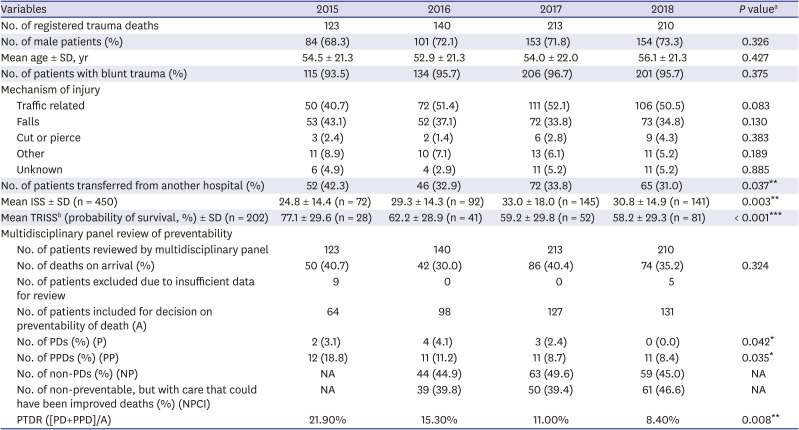
Identification of PTDs, evaluation of preventable factors, and analysis of findings
We have performed panel reviews of trauma deaths since 2015 and established a multidisciplinary panel team comprising at least two general surgeons, an emergency physician, a cardiovascular surgeon, and a neurosurgeon. Opportunities for improvement (OFIs) were analyzed simultaneously at the meeting in which the preventability of trauma deaths was determined. Extensive effort has been made to improve the quality of trauma resuscitation and critical care based on these results, with the beginning of the quality improvement (QI) process as follows. As a result, preventable factors such as bleeding and central nervous system (CNS) injury due to early death, sepsis/multi-organ dysfunction syndrome (MODS), and complications during later stages were identified as urgent prerequisites. Specifically, the main preventable factors in trauma death due to bleeding were delayed initial resuscitation, delayed transfusion, and prolonged time to operation room (OR) for bleeding and hypotension. In case of CNS injury, the main preventable factor was delayed surgery for drainage of epidural hemorrhage (EDH) or subdural hemorrhage (SDH). Appropriate treatment for sepsis/MODS complications was also identified as a preventable factor. Manpower and equipment for initial resuscitation were insufficient and unsuitable to provide adequate care for multiple trauma patients. Resuscitation was not systematic, lacked teamwork, and was often delayed for more than an hour.
Corrective action plans
Guidelines, pathways, and protocols
To reduce pre-hospital trauma deaths, triage criteria, and trauma team activation criteria based on the Field Triage Decision Scheme
10 were prepared to facilitate the direct transfer of severe cases to the trauma center. These guidelines were provided to paramedics and our trauma bay to promote the active admission of severe trauma patients by involving these personnel in gate-keeping for trauma-dedicated medical staff. For patients who visited the trauma bay, paramedics were required to contact the medical/nursing staff prior to arrival and provide instructions to await the patients' arrival.
To avoid deaths occurring in the trauma bay, guidelines were first established or reorganized. We first formed a trauma resuscitation team consisting of a general surgeon, an emergency physician, and a cardiovascular surgeon as the team leader. We unified protocols such as rapid sequence intubation (RSI), emergency transfusion using universal blood emergency transfusion protocol,
11 massive transfusion protocol, resuscitative endovascular balloon occlusion of aorta (REBOA), management of pelvic bone fracture,
12 and ED thoracotomy (EDT).
13 Trauma team configuration for action in a trauma bay was established, and staff therein were trained repeatedly to enhance initial treatment ability. The emergency and massive transfusion protocols were established to prevent early death due to bleeding. Guidelines were established to prevent delays until hemostasis or intervention. For patients with clear hemorrhagic shock, a pathway was established for allowing access to the operating room or angiography room within 1 hour. For EDH and SDH that require craniotomy, a protocol aiming to transfer patients to the operating room within 4 hours was established to reduce the mortality due to CNS injury.
To reduce late-stage preventable deaths due to sepsis/MODS or complications, several guidelines for intensive care were established and distributed. Guidelines to conduct regular rounds by a multidisciplinary team including pharmacists and dietitians were also established. Guidelines for venous thromboembolism (VTE) prophylaxis, ventilator application and weaning, antibiotic use, prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption (PADIS), airway management, glucose control, and feeding in the ICU were modified. All guidelines and protocols were evaluated periodically to ensure compliance and were updated in the manuals accordingly.
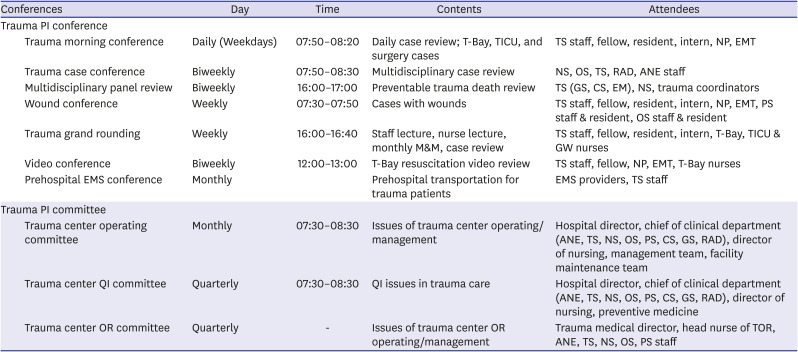
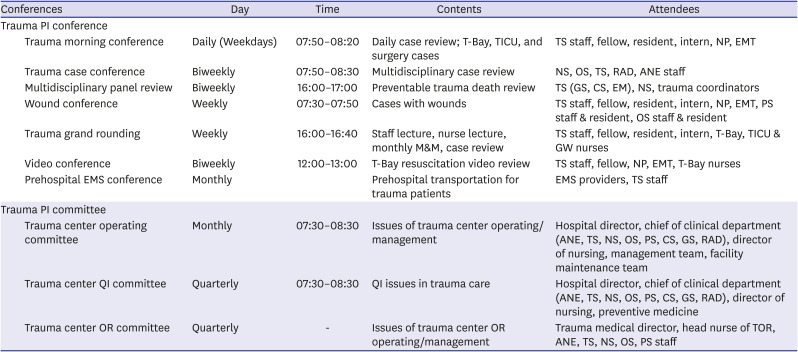
Targeted education
Educational activities were conducted to create an appropriate transfer system for the proper classification of injured patients and to enable direct transfer from the scene to the trauma center. We conducted official meetings for review of trauma cases with local paramedics and offered educational courses. Our team members underwent training courses for trauma resuscitation and critical care, such as Advanced Trauma Life Support (ATLS), Advanced Trauma Care for Nurses (ATCN), and Trauma Care After Resuscitation (TCAR). Staff occasionally traveled abroad to attend the courses. Educational programs and conferences comprising trauma-dedicated medical staff were held regularly to educate nurses in the ICU, OR, and ward by identifying the educational needs that were required in each department (
Table 1).
Table 1
Trauma conference and committee meeting for performance improvement in Ajou Trauma Center
|
Conferences |
Day |
Time |
Contents |
Attendees |
|
Trauma PI conference |
|
|
|
|
|
Trauma morning conference |
Daily (Weekdays) |
07:50–08:20 |
Daily case review; T-Bay, TICU, and surgery cases |
TS staff, fellow, resident, intern, NP, EMT |
|
Trauma case conference |
Biweekly |
07:50–08:30 |
Multidisciplinary case review |
NS, OS, TS, RAD, ANE staff |
|
Multidisciplinary panel review |
Biweekly |
16:00–17:00 |
Preventable trauma death review |
TS (GS, CS, EM), NS, trauma coordinators |
|
Wound conference |
Weekly |
07:30–07:50 |
Cases with wounds |
TS staff, fellow, resident, intern, NP, EMT, PS staff & resident, OS staff & resident |
|
Trauma grand rounding |
Weekly |
16:00–16:40 |
Staff lecture, nurse lecture, monthly M&M, case review |
TS staff, fellow, resident, intern, T-Bay, TICU & GW nurses |
|
Video conference |
Biweekly |
12:00–13:00 |
T-Bay resuscitation video review |
TS staff, fellow, NP, EMT, T-Bay nurses |
|
Prehospital EMS conference |
Monthly |
|
Prehospital transportation for trauma patients |
EMS providers, TS staff |
|
Trauma PI committee |
|
|
|
|
|
Trauma center operating committee |
Monthly |
07:30–08:30 |
Issues of trauma center operating/management |
Hospital director, chief of clinical department (ANE, TS, NS, OS, PS, CS, GS, RAD), director of nursing, management team, facility maintenance team |
|
Trauma center QI committee |
Quarterly |
07:30–08:30 |
QI issues in trauma care |
Hospital director, chief of clinical department (ANE, TS, NS, OS, PS, CS, GS, RAD), director of nursing, preventive medicine |
|
Trauma center OR committee |
Quarterly |
- |
Issues of trauma center OR operating/management |
Trauma medical director, head nurse of TOR, ANE, TS, NS, OS, PS staff |

Peer review presentations
Reviews of videos depicting the resuscitation process in trauma bays were conducted every 2 weeks for the personnel participating in trauma resuscitation to identify the points of improvement. Case presentations, topic reviews, and morbidity and mortality conferences were conducted periodically with orthopedic surgery, plastic surgery, neurosurgery, anesthesiology, radiology, and nursing departments (
Table 1).
Enhancement of resources
The construction of a free-standing trauma center and designation of new trauma bays dedicated solely to trauma patients have solved the physical and structural problems arising from previous EDs in the treatment of severe trauma patients. Even after patients with severe trauma were properly transferred to the trauma center, the existing practice of contacting the medical faculty in charge after inconsistent decision-making by interns and residents was eliminated, thereby securing the resources necessary to attenuate trauma deaths. To operate the trauma center independent of the main building and emergency medical center, it was necessary to secure a large number of medical staff exclusively for the trauma center. We benchmarked the manpower composition of a developed trauma center in the United States that was outfitted similar to ours. We, however, customized this composition to suit the requirements of our medical working environment. We put in place obligatory guidelines, made staffing appointments of dedicated personnel, and obtained financial support from the government. This was made possible by procuring recommendations and after seeking consultations with the government on difficult to operate in-house areas under the existing domestic medical environment. Additionally, measures were taken to improve the financial performance of the center, such as a medical fee 1.5–2 times that of the existing fee for procedures and services performed for severe trauma patients. These efforts have made it possible to ensure the security and smooth operation of all human resources.
The final outcome of this survey (PTDR) was determined according to the WHO TQIP guidelines. First, the trauma coordinators and registrars collected the necessary data for the review, checked the required checklist and audit filters, and requested reviews from individual reviewers. The contents reviewed by individual reviewers were presented at a multidisciplinary panel review held every 2 weeks. Following discussion, preventability was determined, and OFIs were discussed. Results were collected by the QI team. The final decision and OFIs were organized under the leadership of the trauma medical director (TMD) and TPM. A corrective action plan was prepared and implemented. Feedback was provided to other departments and hospitals via the trauma QI committee.
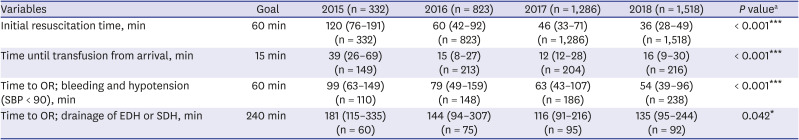
Measurement of PIPS activities and outcomes
In addition to the basic characteristics of trauma patients, the number of hospitalized patients after the establishment of the trauma center facilities, changes in medical staffing, and the number of treatments and operations by trauma specialists were analyzed. Trauma center performance-related statistics, especially trauma resuscitation-related performance in the T-bay, i.e., the number of trauma team members recruited, number of patients in the T-bay, initial resuscitation time in the T-bay (min), time until transfusion from arrival at the T-bay (min), time to OR for patients with bleeding and hypotension (SBP < 90 mmHg), and time to OR for drainage of EDH or SDH were investigated. In addition, mechanical ventilation duration, ICU length of stay (LOS), hospital LOS, crude mortality, and mortality under risk adjustment using various injury severity scoring (ISS) systems were extracted and analyzed for outcome follow-up and comparison.
Data collection and statistical analysis
In this study, we enrolled all trauma admissions recorded in the trauma registry from 2015 to 2018 for a comparative analysis of the PIPS program implemented in our trauma center. The registry registered patients with one or more S or T codes as per the Korean Standard Classification of Diseases (KCD) 7th edition (almost identical to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems) in their diagnosis while exiting the ED or hospital (excluding patients with a code for frostbite, addiction, intoxication, drowning, burns, other and unspecified effects of external causes, or complications regarding surgical and medical care). We evaluated differences in performance and resultant outcomes in trauma care between 2015 and 2018 using the Mann-Whitney U test for continuous variables and χ2 or Fisher's exact test for categorical variables. All statistical analyses were performed using IBM SPSS software (v 25; IBM Corp., Armonk, NY, USA). Differences with a P value of < 0.05 were considered statistically significant.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Ajou University (IRB No. AJIRB-MED-MDB-20-291). The need for obtaining informed consent was waived by the board due to the observational nature of the study.
Go to :

DISCUSSION
Although Korea has made substantial progress in various medical fields, the trauma system is underdeveloped. Jung et al.
5 reported that the nationwide PTDR in Korea in 2015 was 30.5%, highlighting the need for improving the national trauma system. On investigating PTDs in 2006, Kim et al.
14 identified that 51.1% of ED-related issues and 21.8% of pre-hospital-related issues were directly related to deaths in the treatment process; they also highlighted that 58.8% of EDs faced problems with 25.4% of pre-hospital transfers and triages.
1 As such, failure of the pre-hospital transfer system and initial resuscitation commonly accounted for a large proportion of preventable deaths in Korea. Fortunately, several recent reports, including this one, have demonstrated that several Korean regional trauma centers have been successfully established and have contributed to the improvement of local trauma performance.
35 Nevertheless, differences exist in the quality and extent of trauma care at the 15 regional trauma centers that have officially been operating. According to Jung et al.,
5 initial trauma centers have reported good outcomes, but trauma centers that have just commenced operating or have yet to open face difficulties in securing manpower and establishing relevant systems.
The authors' hospital was designated as a regional trauma center at the end of 2013. Following a preparation process, a trauma system was installed via new independent buildings and personnel reinforcement from 2015. Although the official opening was in June 2016, we started developing and applying our QI program in 2015 by referring to the ACSCOT and WHO TQIP guidelines. As the purpose of trauma QI was to reduce the PTDR, mortality conferences were held regularly to select places and elements where the most urgent problems occurred, and a QI program was established based on literature reviews and discussions. Our hospital encountered similar problems as other aforementioned trauma centers in Korea, and we performed performance improvement activities for initial resuscitation.
To function as a trauma center, we focused on increasing the trauma volume and reducing deaths due to bleeding. A trauma hotline was established for smooth communication via conferences with paramedics, and medical consulting was sought for emergency procedures and triage. Paramedics in the field, headquarters of the firefighting department, and trauma surgeons were contacted directly. Direct transfer to the trauma center was recommended, and relevant education was provided to circumvent the need to stop at a local hospital. As a result, the number of patients who visited the trauma center and the number of trauma team activations increased. Trauma surgeons and trauma bay nurses completed the basic ATLS and ATCN education modules and were repeatedly trained to reduce the time spent in the resuscitation room, thereby strengthening the capabilities of the trauma resuscitation team. Further, analysis of resuscitation process-related issues was performed via video conferences. Efforts were made to reduce the resuscitation time.
In this process, protocols such as RSI protocol and EDT indication were established, and OR resuscitation indications were set via continuous conferences with anesthesiologists and operating rooms and communicated to enable rapid movement to the operating room. In addition, for rapid transfusion in bleeding patients with low blood pressure, O Rh (+) blood was placed in the resuscitation room for the first time in Korea to enable an immediate commencement of transfusion.
11 The time to transfusion was significantly shortened, and a more efficient protocol for massive transfusion was designed. Through consultation with the blood bank, balanced transfusion was implemented. In addition, via inter/multi-department conferences and committees involving neurosurgeons, orthopedic surgeons, plastic surgeons, anesthesiologists, and nursing staff, guidelines were established and disagreements were resolved. Further, designated treatments and clinical pathways were reorganized and integrated. This protocol reorganization and improved initial resuscitation promoted a reduction in deaths due to bleeding and time until craniotomy, thereby increasing patient survival.
In addition, efforts were made to increase the number of nursing staff. ICU medical attention guidelines were re-established and applied in a cohesive manner with medical and nursing staff during ICU rounding. For example, VAP prophylaxis guidelines, ventilator application, evacuation and management guidelines, PADIS guidelines, surviving sepsis campaigns, and VTE prophylaxis protocols were established, and relevant educational material was provided. As a result, although the total number of patients and the number of severely ill patients increased, the number of ventilator days was reduced. As the trauma volume increased, resuscitation and the quality of ICU medical attention improved, which naturally led to a decrease in treatment errors and contributed to the reduction in preventable mortality.
The literature on the trauma system in the US and Western Europe highlights the need to focus on studies related to patient survival rates and PIPS programs. According to Shafi et al.,
15 improving the overall outcome of trauma patients had a greater impact on the mortality rate of adult trauma patients admitted to level 1 or 2 trauma centers than the provision of specialized treatment. Davenport et al.
16 reported that several multidisciplinary professional trauma services and PIPS programs at a trauma center in the UK facilitated improvements in trauma outcomes and reduced the mortality of severely injured patients. Similar improvements were noted in a study by DiRusso et al.,
17 in which the overall mortality and mortality of severely injured patients improved, hospital LOS decreased, and even cost reduction was observed, whereby full-time trauma critical care surgeons were added, and quality control and education were conducted for trauma care-oriented management following level 1 trauma center verification. Based on this evidence, we have been striving to introduce and establish PIPS activities from the time of the establishment of the trauma center. To put it concretely, based on the existing guidelines, corrective strategies were established and OFIs were identified through data-gathering and monitoring. New guidelines, pathways, and protocols tailored to suit varied requirements were established, delivered, and shared through targeted education, peer review presentations, etc. Moreover, we tried to secure resources and maintain them to ensure that these corrective action plans were properly implemented at an appropriate time. Consequently, although the number of patients admitted to the trauma center as well as the proportion of severely ill patients increased, the trauma team was actively functioning, and the resuscitation time, stay time, time to blood transfusion and to surgery, number of ventilator days, etc., decreased. Thus, the final goal of reducing the PTDR was achieved. In this study, we report encouraging results showing improvements in trauma outcomes.
This study had several limitations. First, bias may have existed due to the characteristics of retrospective reviews based on medical records and databases. Second, as the QI program was not fully installed from the beginning, a proportion of data for each year may have been missing, which may have biased the comparisons. Third, as the QI programs did not commence at a uniform timepoint, precise comparisons by year are limited due to various confounding factors not covered in the text. Fourth, because the investigations of preventable death were conducted by our panel discussion, bias may have existed in the judgment of preventable deaths. However, no changes were observed in the composition of the panel for the multidisciplinary review during the study period, and decisions were made after final review by a super-panel, TMD, and TPM to reduce bias. In addition, we attempted to reduce the subjectivity of opinions among reviewers by employing a structured review form including audit filter lists in a checklist format. Fifth, DOA patients were excluded from the PTDR. A panel review was conducted for all the trauma deaths that occurred here after admission, but due to emotional and social barriers in Korea, autopsies were not performed extensively, and detailed records of the mechanisms of accidents or situations were lacking.
18 As such, the exact cause of death could not be determined, so the data were excluded from PTDR calculation. To improve this, policies are being proposed to encourage autopsies to be performed when the causes of the accident or death are unknown and to link the records of paramedics in the pre-hospital stage with hospital and trauma center records.
Despite these limitations, this study is the first report on the PIPS program conducted by a government-led trauma center in Korea. Based on the ACSCOT and WHO TQIP guidelines, several QI indicators required for gold-standard trauma centers were introduced by benchmarking. Our data analysis indicated that the trauma outcomes improved over time. The volume of trauma patients, especially those with severe trauma, and the number of trauma team activations increased accordingly, and the overall quality indicators from initial resuscitation to ICU medical attention also improved. As a result, the PTDR was reduced. Our study demonstrates that in countries or regions such as Korea that lack an established trauma system, trauma centers should be installed with the support of local or central governments, and the established trauma centers should utilize existing QI indicators to ensure the provision of gold standard care. Establishing improvement activities will facilitate the reduction in the preventable death rate of trauma patients.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download