INTRODUCTION
Since the use of ultrasonography by emergency physicians (EPs) in the 1980s, point-of-care ultrasound (POCUS) has been increasingly used worldwide in the diagnosis and treatment of patients visiting the emergency department (ED).
12345 In 2001, in the United States, the Model of Clinical Practice of Emergency Medicine was created for a more integrated and representative presentation of the core content of emergency medicine (EM), and bedside ultrasonography was included as an integral diagnostic procedure of the EM model.
6 It has been reported that over 95% of training hospitals in the United States have been teaching POCUS since the early 2000s.
789
In Korea, ultrasonography was introduced in the 1980s, but it was mainly performed by radiologists and cardiologists.
10 In 2002, emergency abdominal ultrasonography and emergency echocardiography were included as one of the essential techniques for residents training in EM
11; however, there were no detailed standards for education and application methods, and POCUS was not used widely in practice until the early 2000s. A study on the status of ultrasonography performed by EP at 46 emergency medical institutions in Seoul and near metropolitan areas of Korea was conducted in 2010.
12 In this study, the frequency of ultrasonography for clinical indications such as multiple trauma, cardiac arrest, right-sided abdominal pain, and renal colic was 53%, and only 36% of institutions had additional ultrasonography training programs except bedside teaching.
In the recent decade, the spread of ultrasound devices has increased in emergency centers in Korea, and ultrasonography education has become more accessible through various ultrasonography workshops and conferences.
1314 In addition, as emergency ultrasonography is covered by national insurance, the use of ultrasound has increased dramatically.
15 However, there have been no nationwide studies on the use of POCUS in emergency medical centers in Korea. In addition, no studies have investigated the perception of POCUS by individual physicians based at emergency medical centers other than representatives of each institution. Therefore, we aimed to investigate the current status, education, perceptions, and barriers to using POCUS in emergency medical centers in Korea through a national survey.
RESULTS
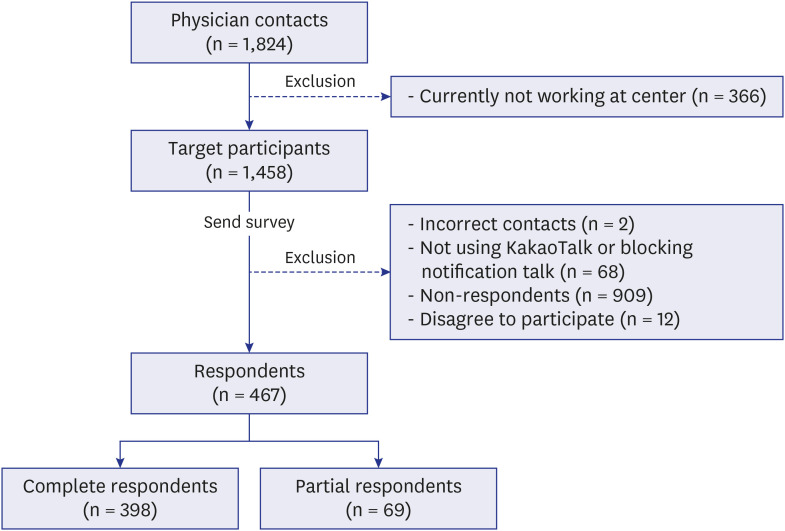
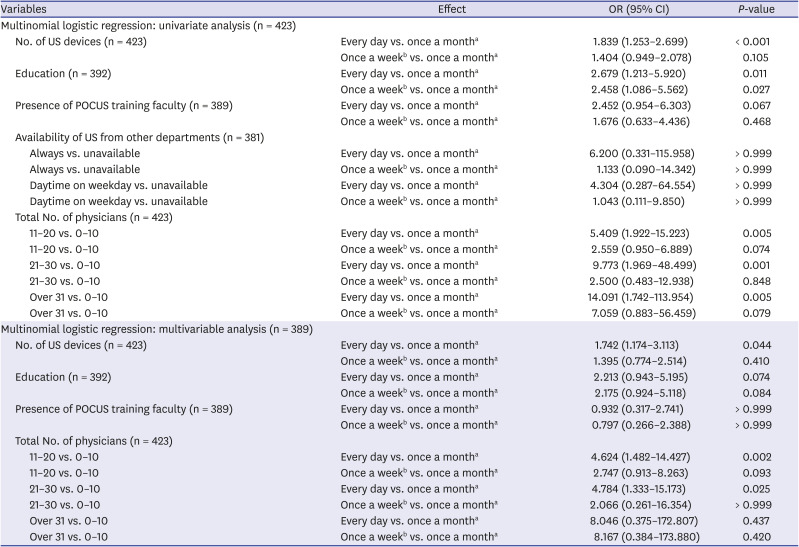
Of the total 1,824 contacts, 366 physicians who were not working in emergency medical centers were excluded as of October 2020. Surveys were sent to 1,458 target physicians. Two incorrect contacts, 68 who did not use KakaoTalk Messenger or blocked the notification talk, and 12 who disagreed to participate in the study were excluded. Excluding 909 non-respondents, the final respondents were 467, of which 398 were complete and 69 were partial. The response rate was 32.0% (
Fig. 1).
Fig. 1
Survey flow.
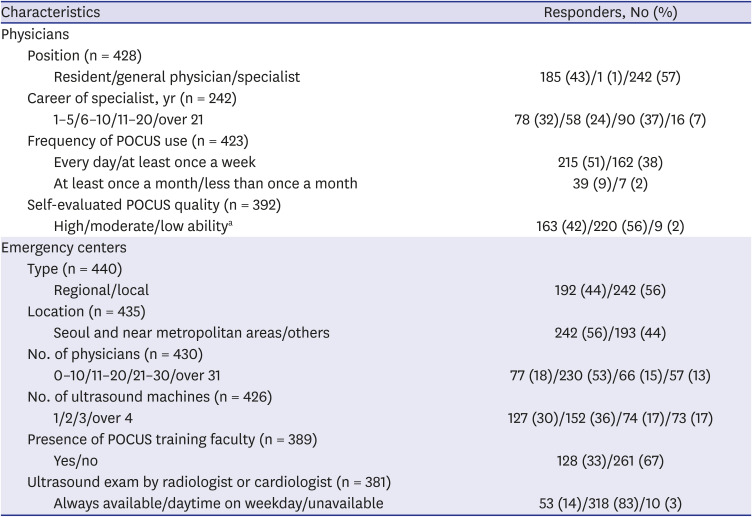
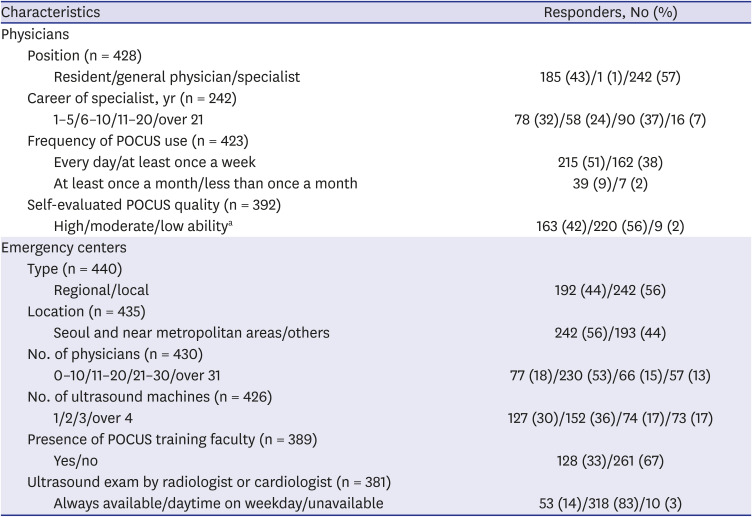
Study responders
A total of 185 (43%) responders were residents, and 242 (57%) were EM specialists, excluding one general physician. As for the careers of the specialist physicians, 136 (56%) served within 10 years, and 16 physicians had more than 20 years of experience. There were 192 physicians (44%) working in regional emergency medical centers and 242 (56%) working in local emergency medical centers. Regarding the number of physicians affiliated with the emergency medical center, more than half of the respondents answered 11 to 20. In terms of the number of ultrasound devices within the center, 65% had one or two units and 17% had more than four units. When asked about the presence or absence of a person in charge of quality assurance or of training in POCUS, only 33% gave an affirmative answer (
Table 1).
Table 1
Characteristics of the survey responders and institutions
|
Characteristics |
Responders, No (%) |
|
Physicians |
|
|
Position (n = 428) |
|
|
|
Resident/general physician/specialist |
185 (43)/1 (1)/242 (57) |
|
Career of specialist, yr (n = 242) |
|
|
|
1–5/6–10/11–20/over 21 |
78 (32)/58 (24)/90 (37)/16 (7) |
|
Frequency of POCUS use (n = 423) |
|
|
|
Every day/at least once a week |
215 (51)/162 (38) |
|
|
At least once a month/less than once a month |
39 (9)/7 (2) |
|
Self-evaluated POCUS quality (n = 392) |
|
|
|
High/moderate/low abilitya
|
163 (42)/220 (56)/9 (2) |
|
Emergency centers |
|
|
Type (n = 440) |
|
|
|
Regional/local |
192 (44)/242 (56) |
|
Location (n = 435) |
|
|
|
Seoul and near metropolitan areas/others |
242 (56)/193 (44) |
|
No. of physicians (n = 430) |
|
|
|
0–10/11–20/21–30/over 31 |
77 (18)/230 (53)/66 (15)/57 (13) |
|
No. of ultrasound machines (n = 426) |
|
|
|
1/2/3/over 4 |
127 (30)/152 (36)/74 (17)/73 (17) |
|
Presence of POCUS training faculty (n = 389) |
|
|
|
Yes/no |
128 (33)/261 (67) |
|
Ultrasound exam by radiologist or cardiologist (n = 381) |
|
|
|
Always available/daytime on weekday/unavailable |
53 (14)/318 (83)/10 (3) |
Current practice
Most of the respondents (96%) stated that they used an ultrasound device when working in an emergency center. Regarding the frequency of POCUS use, 215 (51%) used it every day, followed by 162 (38%) at least once a week, and 39 (9%) at least once a month. In the case of residents, 92% used POCUS at least once a week.
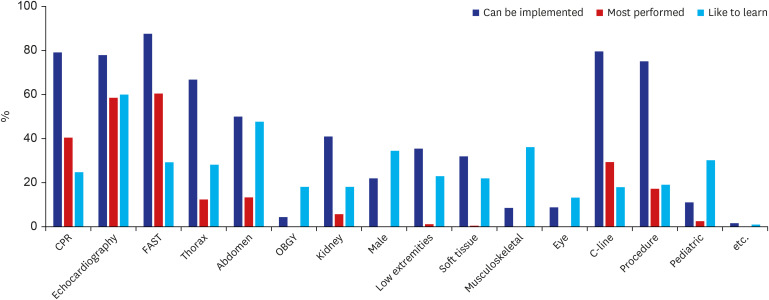
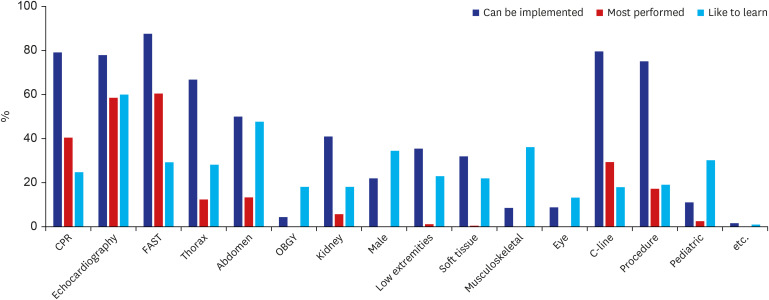
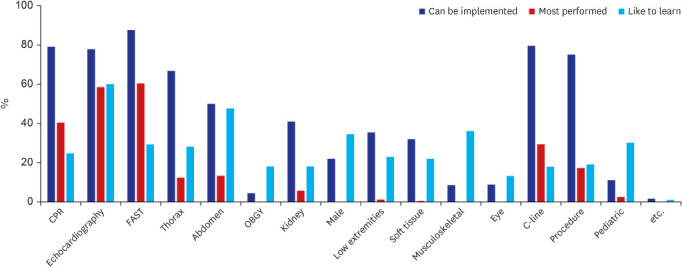
More than 70% of the total 407 respondents answered that various types of ultrasound scans, such as focused assessment with sonography for trauma (FAST), echocardiography, thoracic ultrasound, and ultrasound used for central line insertion, procedures, and cardiopulmonary resuscitation (CPR) can be implemented. In contrast, ultrasound scans for ocular, musculoskeletal, and obstetrics and gynecology were reported by less than 10% of the respondents. The most frequently performed test was FAST (68%), followed by echocardiography (66%), ultrasound for the evaluation of the activity of the heart during CPR (46%), and for central line insertion (33%). The types of ultrasound scan that the physicians were keen to learn about were as follows (in decreasing order of frequency): echocardiography (70%), abdominal scan (56%), musculoskeletal scan (42%), male genitalia scan (40%), and pediatric scan (35%). Regarding the self-assessed POCUS quality, 42% responded that they were skilled, and only 2% reported low skill levels (
Table 1,
Fig. 2).
Fig. 2
Current application types of POCUS and POCUS type that physicians wanted to learn.
POCUS = point-of-care ultrasound, CPR = cardiopulmonary resuscitation, FAST = focused assessment with sonography for trauma, Thorax = thoracic ultrasonography, Abdomen = abdominal ultrasonography, OBGY = obstetrics and gynecological ultrasonography, Kidney = renal and urinary ultrasonography, Male = male genitalia ultrasonography, Low extremities = lower extremities vascular ultrasonography, Soft tissue = soft tissue ultrasonography, Musculoskeletal = musculoskeletal ultrasonography, Eye = ocular ultrasonography, C-line = ultrasonography for central line insertion, Procedure = ultrasonography for the ultrasound-guided procedure, Pediatric = pediatric ultrasonography.
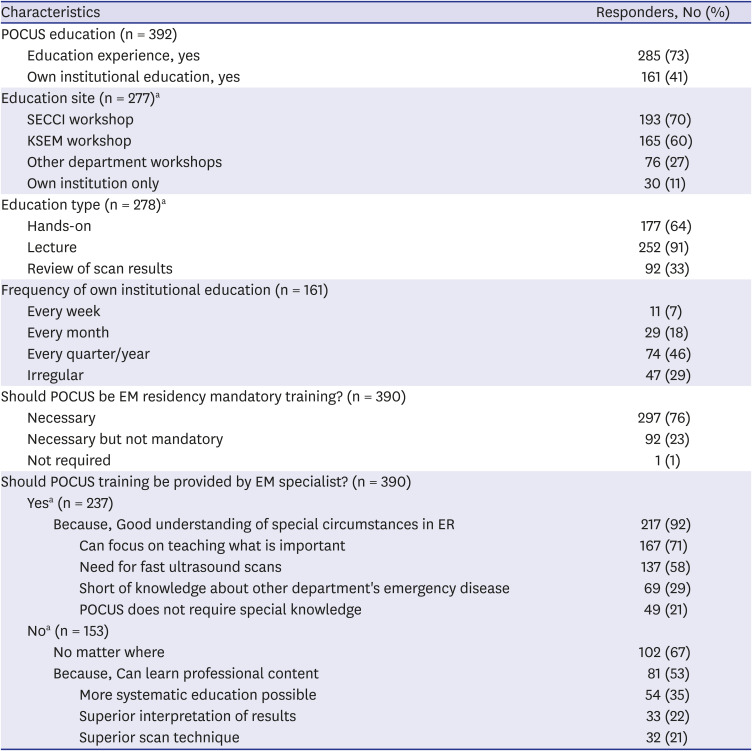
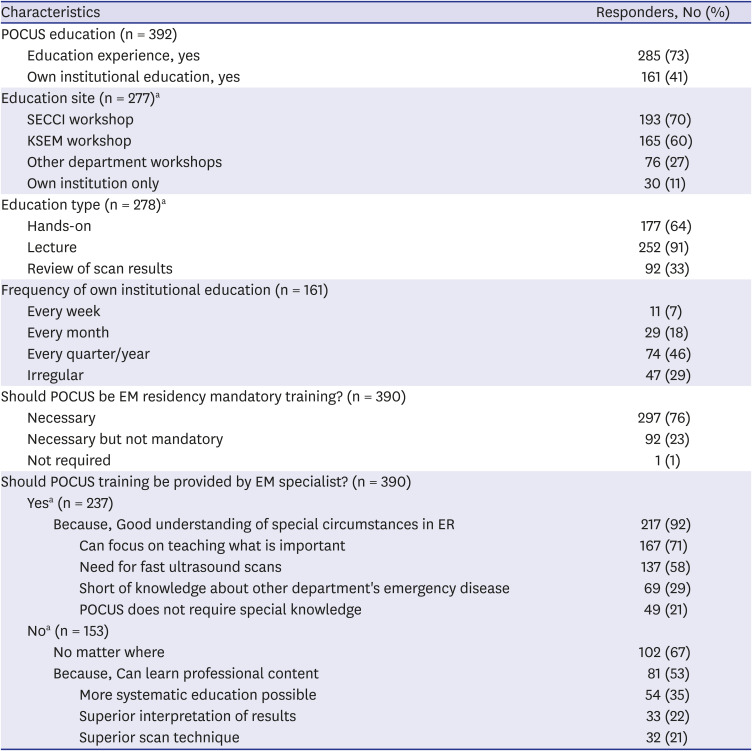
Education
Of the 392 participants, 73% received POCUS education, and 41% were educated at their own medical institution. Among those who received POCUS education, 70% were educated through external imaging society workshops (the Society of Emergency and Critical Care Imaging), followed by KSEM workshops with 60%, other department workshops with 27%, and 11% answered that they only received institutional training. Among the education methods, lectures had the highest frequency at 91%, followed by hands-on sessions at 64%, and scan result review at 33%. In the case of their own institutional education, the frequency of training was 46% for every quarter/year, 29% for irregular sessions, and 7% of respondents stated that they received weekly POCUS education.
When asked about whether POCUS should be included in mandatory residency education in EM, all but one respondent replied that it was necessary and 24% said that it was necessary but should not be mandatory. Sixty-one percent of respondents thought that POCUS training should be performed by EM specialists because they have a good understanding of the special circumstances of ED and can focus on teaching what is important. Some physicians responded that POCUS training should be rendered by experts in other departments because they can provide more professional and systematic education in their respective specialties (
Table 2).
Table 2
POCUS education status and perception
|
Characteristics |
Responders, No (%) |
|
POCUS education (n = 392) |
|
|
Education experience, yes |
285 (73) |
|
Own institutional education, yes |
161 (41) |
|
Education site (n = 277)a
|
|
|
SECCI workshop |
193 (70) |
|
KSEM workshop |
165 (60) |
|
Other department workshops |
76 (27) |
|
Own institution only |
30 (11) |
|
Education type (n = 278)a
|
|
|
Hands-on |
177 (64) |
|
Lecture |
252 (91) |
|
Review of scan results |
92 (33) |
|
Frequency of own institutional education (n = 161) |
|
|
Every week |
11 (7) |
|
Every month |
29 (18) |
|
Every quarter/year |
74 (46) |
|
Irregular |
47 (29) |
|
Should POCUS be EM residency mandatory training? (n = 390) |
|
|
Necessary |
297 (76) |
|
Necessary but not mandatory |
92 (23) |
|
Not required |
1 (1) |
|
Should POCUS training be provided by EM specialist? (n = 390) |
|
|
Yesa (n = 237) |
|
|
|
Because, Good understanding of special circumstances in ER |
217 (92) |
|
|
|
Can focus on teaching what is important |
167 (71) |
|
|
|
Need for fast ultrasound scans |
137 (58) |
|
|
|
Short of knowledge about other department's emergency disease |
69 (29) |
|
|
|
POCUS does not require special knowledge |
49 (21) |
|
Noa (n = 153) |
|
|
|
No matter where |
102 (67) |
|
|
Because, Can learn professional content |
81 (53) |
|
|
|
More systematic education possible |
54 (35) |
|
|
|
Superior interpretation of results |
33 (22) |
|
|
|
Superior scan technique |
32 (21) |
Billing and report
Most of the physicians working in the emergency center responded that they bill the patient after the ultrasound examination, but 16% of the physicians answered that they did not charge. About half of the respondents said that they had a standard format for recording POCUS results. Scan results were recorded in most cases (95%), but 52% of respondents said they were recorded only in the text.
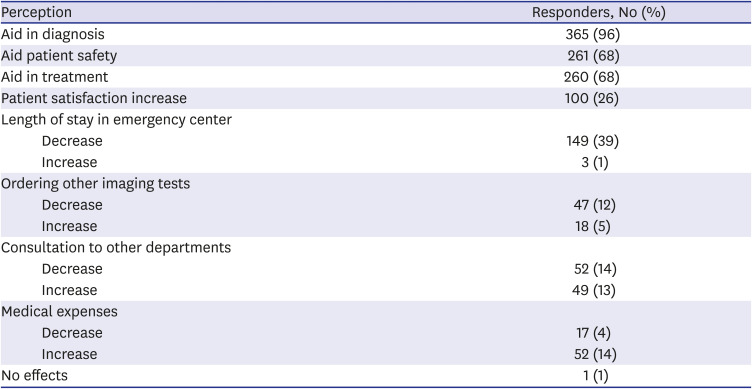
Perception regarding POCUS
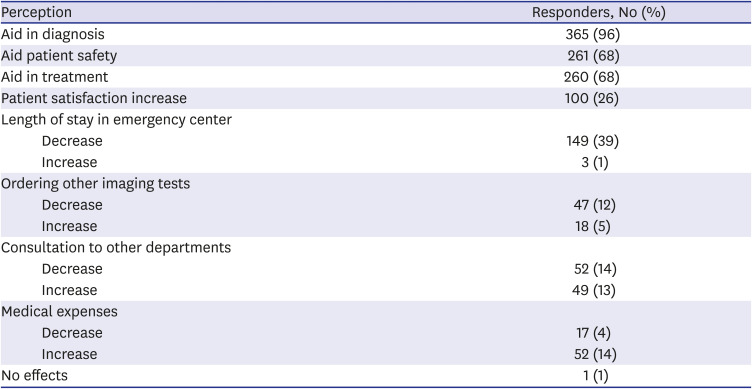
When asked about the necessity of POCUS, 97% of the respondents answered that it was needed, and 88% expected its usage to increase further in the future. About half of the respondents said that the percentage of making a definite diagnosis with POCUS alone was over 60%. Regarding the impact of POCUS, most people answered that POCUS is helpful for diagnosis, and 68% were of the view that it is helpful for patient safety and effective treatment. When POCUS was performed, they thought that the length of stay in the ED and the need for other imaging modalities would be reduced, but that the medical expenses would increase (
Table 3).
Table 3
Perception of the impact of POCUS (n = 382)
|
Perception |
Responders, No (%) |
|
Aid in diagnosis |
365 (96) |
|
Aid patient safety |
261 (68) |
|
Aid in treatment |
260 (68) |
|
Patient satisfaction increase |
100 (26) |
|
Length of stay in emergency center |
|
|
Decrease |
149 (39) |
|
Increase |
3 (1) |
|
Ordering other imaging tests |
|
|
Decrease |
47 (12) |
|
Increase |
18 (5) |
|
Consultation to other departments |
|
|
Decrease |
52 (14) |
|
Increase |
49 (13) |
|
Medical expenses |
|
|
Decrease |
17 (4) |
|
Increase |
52 (14) |
|
No effects |
1 (1) |
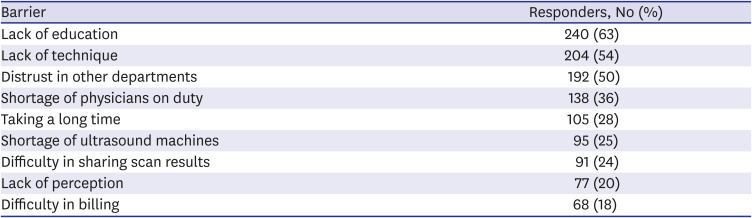
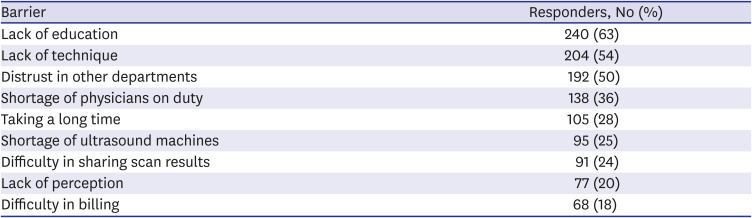
Barriers
As for barriers to using POCUS, lack of education (63%) received the highest response, followed by lack of techniques (54%), and lack of trust from other department in POCUS results by EM physicians (50%). Other responses suggested that ultrasound scanning takes a long time and is difficult to apply due to the shortage of physicians on duty (
Table 4).
Table 4
Barriers using POCUS (n = 381)
|
Barrier |
Responders, No (%) |
|
Lack of education |
240 (63) |
|
Lack of technique |
204 (54) |
|
Distrust in other departments |
192 (50) |
|
Shortage of physicians on duty |
138 (36) |
|
Taking a long time |
105 (28) |
|
Shortage of ultrasound machines |
95 (25) |
|
Difficulty in sharing scan results |
91 (24) |
|
Lack of perception |
77 (20) |
|
Difficulty in billing |
68 (18) |
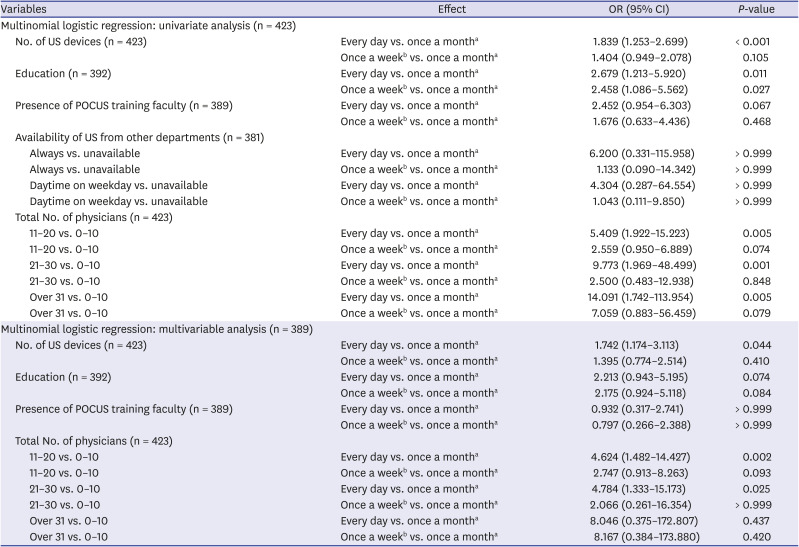
Factors affecting the frequency of use of POCUS
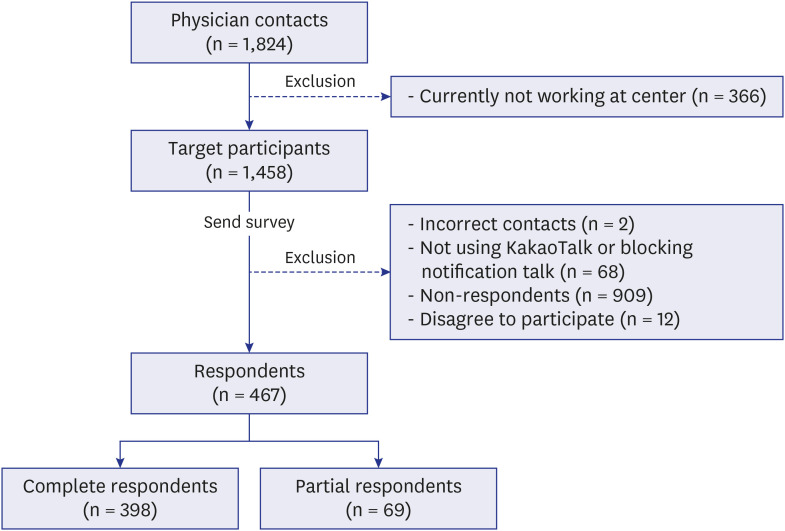
The number of ultrasound devices, education, presence of POCUS training faculty, and the total number of physicians in the emergency center were analyzed as factors that significantly influenced the frequency of POCUS use in univariate multinomial logistic regression. Multivariate multinomial logistic regression analysis revealed that the greater the number of ultrasound devices and the total number of physicians in the emergency center, the more likely they were to use POCUS every day (type 3
P < 0.05). In other words, as the number of ultrasound devices in the emergency center increased, the number of people who used ultrasound every day was significantly greater than the number who used it less than once a month (odds ratio [OR], 1.742, 95% confidence interval [CI], 1.174–3.113, adjusted
P = 0.044). In addition, when the number of physicians in the emergency center was 11–20 and 21–30, there were significantly more people using ultrasound every day than when there were fewer than 10 physicians (11–20: OR, 4.624, 95% CI, 1.482–14.427, adjusted
P = 0.002; 21–30: OR, 4.784, 95% CI, 1.333–15.173, adjusted
P = 0.025) (
Table 5).
Table 5
Factors affecting the frequency of use of POCUS
|
Variables |
Effect |
OR (95% CI) |
P-value |
|
Multinomial logistic regression: univariate analysis (n = 423) |
|
|
|
|
No. of US devices (n = 423) |
Every day vs. once a montha
|
1.839 (1.253–2.699) |
< 0.001 |
|
Once a weekb vs. once a montha
|
1.404 (0.949–2.078) |
0.105 |
|
Education (n = 392) |
Every day vs. once a montha
|
2.679 (1.213–5.920) |
0.011 |
|
Once a weekb vs. once a montha
|
2.458 (1.086–5.562) |
0.027 |
|
Presence of POCUS training faculty (n = 389) |
Every day vs. once a montha
|
2.452 (0.954–6.303) |
0.067 |
|
Once a weekb vs. once a montha
|
1.676 (0.633–4.436) |
0.468 |
|
Availability of US from other departments (n = 381) |
|
|
|
|
|
Always vs. unavailable |
Every day vs. once a montha
|
6.200 (0.331–115.958) |
> 0.999 |
|
|
Always vs. unavailable |
Once a weekb vs. once a montha
|
1.133 (0.090–14.342) |
> 0.999 |
|
|
Daytime on weekday vs. unavailable |
Every day vs. once a montha
|
4.304 (0.287–64.554) |
> 0.999 |
|
|
Daytime on weekday vs. unavailable |
Once a weekb vs. once a montha
|
1.043 (0.111–9.850) |
> 0.999 |
|
Total No. of physicians (n = 423) |
|
|
|
|
|
11–20 vs. 0–10 |
Every day vs. once a montha
|
5.409 (1.922–15.223) |
0.005 |
|
|
11–20 vs. 0–10 |
Once a weekb vs. once a montha
|
2.559 (0.950–6.889) |
0.074 |
|
|
21–30 vs. 0–10 |
Every day vs. once a montha
|
9.773 (1.969–48.499) |
0.001 |
|
|
21–30 vs. 0–10 |
Once a weekb vs. once a montha
|
2.500 (0.483–12.938) |
0.848 |
|
|
Over 31 vs. 0–10 |
Every day vs. once a montha
|
14.091 (1.742–113.954) |
0.005 |
|
|
Over 31 vs. 0–10 |
Once a weekb vs. once a montha
|
7.059 (0.883–56.459) |
0.079 |
|
Multinomial logistic regression: multivariable analysis (n = 389) |
|
|
|
|
No. of US devices (n = 423) |
Every day vs. once a montha
|
1.742 (1.174–3.113) |
0.044 |
|
Once a weekb vs. once a montha
|
1.395 (0.774–2.514) |
0.410 |
|
Education (n = 392) |
Every day vs. once a montha
|
2.213 (0.943–5.195) |
0.074 |
|
Once a weekb vs. once a montha
|
2.175 (0.924–5.118) |
0.084 |
|
Presence of POCUS training faculty (n = 389) |
Every day vs. once a montha
|
0.932 (0.317–2.741) |
> 0.999 |
|
Once a weekb vs. once a montha
|
0.797 (0.266–2.388) |
> 0.999 |
|
Total No. of physicians (n = 423) |
|
|
|
|
|
11–20 vs. 0–10 |
Every day vs. once a montha
|
4.624 (1.482–14.427) |
0.002 |
|
|
11–20 vs. 0–10 |
Once a weekb vs. once a montha
|
2.747 (0.913–8.263) |
0.093 |
|
|
21–30 vs. 0–10 |
Every day vs. once a montha
|
4.784 (1.333–15.173) |
0.025 |
|
|
21–30 vs. 0–10 |
Once a weekb vs. once a montha
|
2.066 (0.261–16.354) |
> 0.999 |
|
|
Over 31 vs. 0–10 |
Every day vs. once a montha
|
8.046 (0.375–172.807) |
0.437 |
|
|
Over 31 vs. 0–10 |
Once a weekb vs. once a montha
|
8.167 (0.384–173.880) |
0.420 |
Non-use of ultrasound devices
Among 19 (4%) who answered that they did not use ultrasound, 17 knew what POCUS was, and 11 responded that POCUS should be implemented in the emergency room (ER). Most ultrasound non-users answered that the reason is the shortage of ultrasound devices and distrust in other departments about the scan result, followed by the lack of scanning skills and the difficulty of billing.
DISCUSSION
POCUS has become a widely available and essential tool in EM practice. We investigated the current practice and perception of POCUS in emergency centers in Korea through a national survey. The response rate of this survey was 32%, but it included physicians affiliated with 155 centers, 96% of 164 emergency medical centers in Korea, and physicians from all EM residency training centers. In this survey, the respondents were residents and specialists at a ratio of 4:6, and residency grades were distributed almost evenly, making it suitable for analyzing overall opinions. We found that 96% of the respondents used ultrasound, and half of them used ultrasound every day. In addition, all emergency centers were equipped with ultrasound devices, and 35% of the centers had more than three units. Therefore, it was evident that the use and spread of ultrasound increased significantly from the results of the survey 10 years ago in Korea.
12 This might be owing to the impact of health insurance coverage for POCUS in emergency and intensive care units since 2019, following the government's efforts to enhance Korean National Insurance Coverage.
15
In this survey, the FAST scan showed the greatest frequency for both the tests that can be performed and the tests that are performed most often. In Lee et al.'s study,
12 which surveyed the status and activities of EP-performed ultrasonography in Seoul and near metropolitan cities in Korea 10 years ago, the frequency of applying ultrasound for chest pain was about 36%, but in this survey, 64% responded that echocardiography was the most used. The frequency of an echocardiography scan significantly increased. In addition, when a central line insertion or procedure was conducted, ultrasound could be implemented in more than 80% of the respondents. In addition, 30% of respondents chose this scan as the most frequently performed scan, and this was nearly twice as high as that 10 years ago (16%). It is believed that this may be due to several studies showing that ultrasound-guided procedures are safer for patients and have higher success rates, indicating that it was also due to improved accessibility to the ultrasound.
1516 The rate for selecting abdominal ultrasonography as the most commonly used test was as low as 15%, which may reflect the reality of Korean emergency centers where the use of other imaging modalities such as computerized tomography is relatively easy, and is possible under wide insurance coverage.
None of the respondents selected a musculoskeletal scan and male genitalia scan in the questionnaire asking for frequently performed tests, and only 3% chose a pediatric scan, but these scans were ranked 3rd, 4th, and 5th in the tests they wanted to learn. Considering the frequency of patients visiting the ED, it can be seen that musculoskeletal and pediatric scans are not yet actively applied in emergency centers in Korea. Nevertheless, many physicians want to learn these scans, and this may reflect the desire to learn various aspects of an ultrasound in addition to the currently widely applied ultrasound scans in a situation where the role of EPs in the ED is increasing. In particular, the usefulness and advantage of pediatric ultrasonography can be attributed to the lack of the risk of radiation exposure and the fact that sedation is not required.
In addition, about 73% of the respondents received ultrasound education, and 41% received ultrasound education at their own institutions. Although POCUS education in Korea has increased, 24% of residents and 30% of specialists answered that they had never received POCUS training. In addition, 67% said that there was no person in charge of POCUS training. The barriers to education (lack of education, lack of technique, distrust by other departments about the results, and lack of awareness) accounted for about 60% of the questions about the barriers to POCUS use. Several studies have shown that the use of ultrasound is increasing with the presence of the person in charge of POCUS training and the increase in POCUS education, and its improvement is needed to expand POCUS.
1217 However, among those who received ultrasonography training at their own institutions, 25% answered that they receive ultrasonography training every week or every month, indicating that some emergency centers are actively performing ultrasonography training.
Respondents were aware of the importance of POCUS as evidenced by their opinions that POCUS is necessary for resident education (99%), medical practice (97%), and that its frequency of use will increase in the future (88%). In addition, over 70% responded that POCUS should be mandatory in residency training in EM and 61% believed that EM specialists should be in charge of POCUS training. In a recent study on ultrasound education in United States medical schools, 72% of ultrasound directors were from the ED, so it can be seen that the role of EPs is increasingly important in ultrasound use and education in medical practice.
18 However, some respondents reported that they should receive POCUS training via experts from other departments, and 50% answered “distrust from other departments about scan results” as a barrier to ultrasound use. Therefore, more professional, systematic ultrasonography training with stringent protocols is needed for EPs.
Our study found that the number of ultrasound devices and the total number of physicians in the emergency center were found to be factors that influenced the frequency of POCUS use. The participants of this study were physicians working in secondary or tertiary emergency medical institutions where the ER was overcrowded. Therefore, if the number of ultrasound devices available and sufficient medical staff to work are secured, the frequency of ultrasound application may increase. Bobbia et al.
19 also reported that human resources and infrastructure have the greatest effect on the availability of ultrasound. In our study, some respondents reported shortage of physicians on duty, taking a long time to scan, and shortage of ultrasound devices as obstacles for POCUS use. Therefore, it was shown that increasing the accessibility of ultrasonography by improving these factors is a paramount factor that can increase the use of ultrasonography.
The unique feature of this study is that the survey was conducted using KakaoTalk, a mobile messenger. This messenger is the most widely used mobile messenger in Korea
18 and was adopted in this study to increase the response rate of questionnaires and speed up the response time. The survey was sent twice, and it was completed within 2 weeks, reaching the expected response rate. Because the screen of a mobile phone is small, adjustments were needed to make the questionnaire efficient and presentable, but because of its easy accessibility, it can be used for many surveys in future.
Through this study, we were able to clearly evaluate the current status of the use, education, and perception of POCUS among Korean EPs. Most physicians who participated in the survey were aware of the need for POCUS, and it was found that the frequency of POCUS use was higher than that in the previous study. However, lack of education and infrastructure still emerged as a barrier to the use of POCUS. In addition, this study found that physicians in emergency medical centers believed that POCUS education was necessary and that the demand for mandatory POCUS education for EM residents was high. To address this, it is thought that there should be discussions on the introduction of an EM residency credential system for POCUS in the future and that it is necessary to cultivate POCUS education by a personnel in the institution. Furthermore, research on POCUS education and objective evaluation of the scan results is considered necessary.
There are several potential limitations of this survey-based study. First, our results may be prone to selection bias, as it is more likely that physicians interested in POCUS or who possess specialized knowledge of POCUS have responded to the questionnaire. Therefore, the frequency of use and scope of POCUS suggested by the results of the survey might have been overestimated. Second, although attempts were made to contact all physicians working in the emergency center, we could not obtain all the physicians' contact details. A sampling bias may occur because a total of 1,470 people does not represent all EPs in Korea. Third, as a result of our study, it was inferred that the number of ultrasound devices and physicians in emergency centers influenced the frequency of ultrasound use. However, as each emergency center comprises patients with different demographics, such as age and co-morbidity, and differs in patient volume, the results of our study must be interpreted in the light of these factors.
In conclusion, it was found that most Korean EPs currently working in emergency centers perform various types of ultrasound scans such as FAST, echocardiography, thoracic ultrasound, ultrasound-guided central line insertion, and CPR procedures. Nevertheless, POCUS education is still a big barrier to its use, and it is necessary to introduce a credential system for POCUS education and EM residency training in the future. In addition, to further promote the use of POCUS, it would be helpful to improve accessibility by placing and appointing a sufficient number of ultrasound devices and physicians in emergency centers.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download