1. Bornholt LJ, Ajersch S, Fisher IH, Markham RH, Ouvrier RA. Cognitive screening for children and adolescents: general limits or ceiling effects? J Child Neurol. 2010; 25(5):567–571. PMID:
20110215.

2. Bornholt LJ, Spencer FH, Fisher IH, Ouvrier RA. Cognitive screening for young children: development and diversity in learning contexts. J Child Neurol. 2004; 19(5):313–317. PMID:
15224702.

3. Epstein HT, Chapter VI. Correlated brain and intelligence development in humans. In : Hahn ME, Jensen C, Dudek BC, editors. Development and Evolution of Brain Size: Behavioral Implications. New York, NY, USA: Academic Press;1979. p. 111–131.
4. Harshman LA, Johnson RJ, Matheson MB, Kogon AJ, Shinnar S, Gerson AC, et al. Academic achievement in children with chronic kidney disease: a report from the CKiD cohort. Pediatr Nephrol. 2019; 34(4):689–696. PMID:
30448874.

5. Shehata G, Eltayeb A. Cognitive function and event-related potentials in children with type 1 diabetes mellitus. J Child Neurol. 2010; 25(4):469–474. PMID:
19762507.

6. Shehata GA, Bateh AA. Cognitive function, mood, behavioral aspects, and personality traits of adult males with idiopathic epilepsy. Epilepsy Behav. 2009; 14(1):121–124. PMID:
18801461.

7. Shehata GA, Elsayh KI, Rafet NH, Mohamed AO, Rageh TA. Study of β-thalassemia biomarkers and their relationship to cognition among children. J Child Neurol. 2010; 25(12):1473–1479. PMID:
20519673.
8. Haavisto A, Korkman M, Holmberg C, Jalanko H, Qvist E. Neuropsychological profile of children with kidney transplants. Nephrol Dial Transplant. 2012; 27(6):2594–2601. PMID:
22140125.

9. Duquette PJ, Hooper SR, Wetherington CE, Icard PF, Gipson DS. Brief report: intellectual and academic functioning in pediatric chronic kidney disease. J Pediatr Psychol. 2007; 32(8):1011–1017. PMID:
17556399.

10. Hartung EA, Kim JY, Laney N, Hooper SR, Radcliffe J, Port AM, et al. Evaluation of neurocognition in youth with CKD using a novel computerized neurocognitive battery. Clin J Am Soc Nephrol. 2016; 11(1):39–46. PMID:
26500247.

11. Falger J, Latal B, Landolt MA, Lehmann P, Neuhaus TJ, Laube GF. Outcome after renal transplantation. Part I: intellectual and motor performance. Pediatr Nephrol. 2008; 23(8):1339–1345. PMID:
18389283.

12. Chen K, Didsbury M, van Zwieten A, Howell M, Kim S, Tong A, et al. Neurocognitive and educational outcomes in children and adolescents with CKD: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2018; 13(3):387–397. PMID:
29472306.
13. Choudhury S, Charman T, Blakemore SJ. Development of the teenage brain. Mind Brain Educ. 2008; 2(3):142–147.

14. Hollenbeck GP, Kaufman AS. Factor analysis of the Wechsler preschool and primary scale of intelligence (WPPSI). J Clin Psychol. 1973; 29(1):41–45.

15. Kang HG, Choi HJ, Han KH, Kim SH, Cho HY, Cho MH, et al. KNOW-Ped CKD (KoreaN cohort study for outcomes in patients with pediatric CKD): design and methods. BMC Nephrol. 2016; 17(1):35. PMID:
27012243.

16. Baek HS, Kang HG, Choi HJ, Cheong HI, Ha IS, Han KH, et al. Health-related quality of life of children with pre-dialysis chronic kidney disease. Pediatr Nephrol. 2017; 32(11):2097–2105. PMID:
28685173.

17. Cho H, Choi HJ, Kang HG, Ha IS, Cheong HI, Han KH, et al. Influence of the method of definition on the prevalence of left-ventricular hypertrophy in children with chronic kidney disease: data from the KNOW-Ped CKD study. Kidney Blood Press Res. 2017; 42(3):406–415. PMID:
28689198.

18. Lee KH, Park E, Choi HJ, Kang HG, Ha IS, Cheong HI, et al. Anemia and iron deficiency in children with chronic kidney disease (CKD): data from the KNOW-Ped CKD Study. J Clin Med. 2019; 8(2):152.

19. Baek HS, Kim SH, Kang HG, Choi HJ, Cheong HI, Ha IS, et al. Dyslipidemia in pediatric CKD patients: results from KNOW-PedCKD (KoreaN cohort study for Outcomes in patients With Pediatric CKD). Pediatr Nephrol. 2020; 35(8):1455–1461. PMID:
32232640.

20. Kang NR, Ahn YH, Park E, Choi HJ, Kim SH, Cho H, et al. Mental health and psychosocial adjustment in pediatric chronic kidney disease derived from the KNOW-Ped CKD study. Pediatr Nephrol. 2019; 34(10):1753–1764. PMID:
31222663.

21. Wechsler D. Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) Technical and Interpretive Manual. San Antonio, TX, USA: Pearson Incorporated;2008.
22. In : Hwang ST, Kim JH, Park KB, Choi JY, Hong SH, editors. Standardization of the K-WAIS-IV. Proceedings of Korean Psychological Association Annual Conference; 2012 Aug 24; Chuncheon, Korea. Seoul: Korean Psychological Association;2012.
23. Kwak KC, Park HW, Kim CT. Korean Wechsler Intelligence Scale for Children-III (K-WISC-III). Seoul, Korea: Seoul Special Education Publishing Co.;2001.
24. Kwak KJ, Oh SW, Kim CT. Korean-Wechsler Intelligence Scale for Children-IV Guide Book for Expert. Seoul, Korea: Hakjisa;2011. p. 11–13.
25. Bawden HN, Acott P, Carter J, Lirenman D, MacDonald GW, McAllister M, et al. Neuropsychological functioning in end-stage renal disease. Arch Dis Child. 2004; 89(7):644–647. PMID:
15210497.
26. Johnson RJ, Warady BA. Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol. 2013; 28(8):1283–1291. PMID:
23553044.

27. Hartung EA, Matheson M, Lande MB, Dell KM, Guay-Woodford LM, Gerson AC, et al. Neurocognition in children with autosomal recessive polycystic kidney disease in the CKiD cohort study. Pediatr Nephrol. 2014; 29(10):1957–1965. PMID:
24828609.

28. Hooper SR, Gerson AC, Butler RW, Gipson DS, Mendley SR, Lande MB, et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol. 2011; 6(8):1824–1830. PMID:
21737850.

29. Mehls O, Lindberg A, Nissel R, Haffner D, Hokken-Koelega A, Ranke MB. Predicting the response to growth hormone treatment in short children with chronic kidney disease. J Clin Endocrinol Metab. 2010; 95(2):686–692. PMID:
20008024.

30. Gerson AC, Butler R, Moxey-Mims M, Wentz A, Shinnar S, Lande MB, et al. Neurocognitive outcomes in children with chronic kidney disease: current findings and contemporary endeavors. Ment Retard Dev Disabil Res Rev. 2006; 12(3):208–215. PMID:
17061289.

31. Hartmann H, Hawellek N, Wedekin M, Vogel C, Das AM, Balonwu K, et al. Early kidney transplantation improves neurocognitive outcome in patients with severe congenital chronic kidney disease. Transpl Int. 2015; 28(4):429–436. PMID:
25557263.

32. Chhabra YK, Sood S, Rathi O, Mahajan S. Effect of renal transplantation on cognitive function in hemodialysis patients: a longitudinal study. Int Urol Nephrol. 2017; 49(11):2071–2078. PMID:
28900874.

33. Lande MB, Gerson AC, Hooper SR, Cox C, Matheson M, Mendley SR, et al. Casual blood pressure and neurocognitive function in children with chronic kidney disease: a report of the children with chronic kidney disease cohort study. Clin J Am Soc Nephrol. 2011; 6(8):1831–1837. PMID:
21700829.

34. Ruebner RL, Laney N, Kim JY, Hartung EA, Hooper SR, Radcliffe J, et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am J Kidney Dis. 2016; 67(4):567–575. PMID:
26476795.
35. Joosten H, Izaks GJ, Slaets JP, de Jong PE, Visser ST, Bilo HJ, et al. Association of cognitive function with albuminuria and eGFR in the general population. Clin J Am Soc Nephrol. 2011; 6(6):1400–1409. PMID:
21566108.

36. Halterman JS, Kaczorowski JM, Aligne CA, Auinger P, Szilagyi PG. Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics. 2001; 107(6):1381–1386. PMID:
11389261.

37. Williams UE, Oparah SK, Soter A. Predictors of cognitive dysfunction among patients with moderate to severe chronic kidney disease. Recent Adv Biol Med. 2017; 3:18–23.

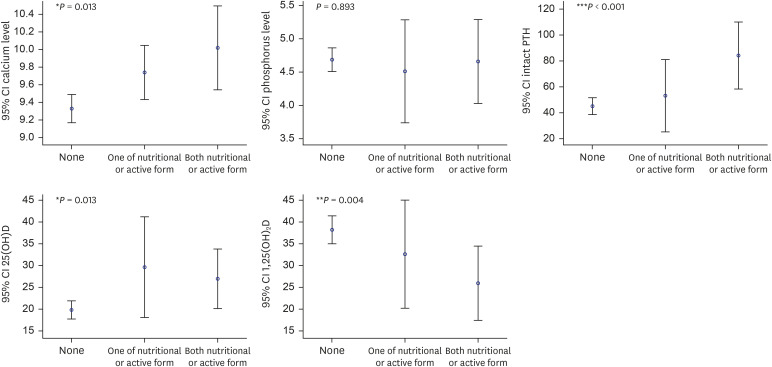
38. Yokoyama JS, Matsuda-Abedini M, Denburg MR, Kumar J, Warady BA, Furth SL, et al. Association between chronic kidney disease–mineral bone disease (CKD-MBD) and cognition in children: Chronic Kidney Disease in Children (CKiD) Study. Kidney Med. 2020; 2(4):398–406. PMID:
32775979.

39. Annweiler C, Dursun E, Féron F, Gezen-Ak D, Kalueff AV, Littlejohns T, et al. ‘Vitamin D and cognition in older adults’: updated international recommendations. J Intern Med. 2015; 277(1):45–57. PMID:
24995480.

40. Li L, Prabhakaran K, Zhang X, Zhang L, Liu H, Borowitz JL, et al. 1α,25-dihydroxyvitamin D3 attenuates cyanide-induced neurotoxicity by inhibiting uncoupling protein-2 up-regulation. J Neurosci Res. 2008; 86(6):1397–1408. PMID:
18183618.

41. Taniura H, Ito M, Sanada N, Kuramoto N, Ohno Y, Nakamichi N, et al. Chronic vitamin D3 treatment protects against neurotoxicity by glutamate in association with upregulation of vitamin D receptor mRNA expression in cultured rat cortical neurons. J Neurosci Res. 2006; 83(7):1179–1189. PMID:
16521124.

42. Dusso AS, Tokumoto M. Defective renal maintenance of the vitamin D endocrine system impairs vitamin D renoprotection: a downward spiral in kidney disease. Kidney Int. 2011; 79(7):715–729. PMID:
21270766.

43. Chung S, Kim M, Koh ES, Hwang HS, Chang YK, Park CW, et al. Serum 1,25-dihydroxyvitamin D better reflects renal parameters than 25-hydoxyvitamin D in patients with glomerular diseases. Int J Med Sci. 2017; 14(11):1080–1087. PMID:
29104461.

44. Shaffi K, Tighiouart H, Scott T, Lou K, Drew D, Weiner D, et al. Low 25-hydroxyvitamin D levels and cognitive impairment in hemodialysis patients. Clin J Am Soc Nephrol. 2013; 8(6):979–986. PMID:
23449769.

45. Liu GL, Pi HC, Hao L, Li DD, Wu YG, Dong J. Vitamin D status is an independent risk factor for global cognitive impairment in peritoneal dialysis patients. PLoS One. 2015; 10(12):e0143782. PMID:
26630385.

46. Jovanovich AJ, Chonchol M, Brady CB, Kaufman JD, Kendrick J, Cheung AK, et al. 25-vitamin D, 1,25-vitamin D, parathyroid hormone, fibroblast growth factor-23 and cognitive function in men with advanced CKD: a veteran population. Clin Nephrol. 2014; 82(5):S1–4. PMID:
25208315.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download