Dual antiplatelet therapy (DAPT) using aspirin and P2Y12 receptor inhibitor has been proven to reduce recurrent ischemic events, such as stent thrombosis and myocardial infarction (MI), after percutaneous coronary intervention (PCI), but it is less effective for prevention of ischemic stroke and systemic embolism in patients with atrial fibrillation (AF) when compared with oral anticoagulation therapy (OAC).1) Triple antithrombotic therapy (TAT) with OAC and DAPT has been recommended in treatment guidelines for patients with AF after PCI. However, this approach could increase the risk of excessive major bleeding. In Korea, only DAPT was prescribed in more than 90% of patients with AF after PCI during the era of vitamin K antagonist (VKA) for OAC.2) Discrepancies between guidelines and real-world clinical practice might be associated with bleeding concerns including intracranial hemorrhage and inconvenience to use of VKA such as narrow therapeutic window, drug and dietary interactions, and intra-patient variability requiring frequent monitoring.
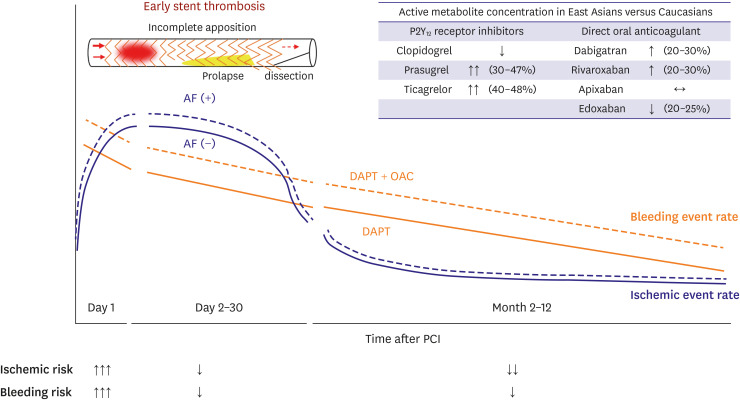
In this edition of the Korean Circulation Journal, Kwon et al.3) showed the patterns of peri-procedural antithrombotic regimens in 27,594 Korean patients with AF who underwent PCI using the claims database of the Health Insurance Review and Assessment (HIRA). The patterns of peri-procedural antithrombotic regimens have changed rapidly toward more use of non-vitamin K antagonist oral anticoagulants (NOAC)-based TAT from DAPT without OAC. These change were possibly due to the introduction and insurance coverage of NOACs in Korea. NOACs reduce the risk of hemorrhagic stroke and all-cause mortality than VKA, and the benefit was more profound in Asian population than in non-Asian populations,1) and NOACs also have pharmacologic advantages over VKA including rapid onset/offset action, fewer drug and dietary interactions, and no need for regular monitoring. When Korean clinicians decided on NOAC-based regimen, percentage of reduced-dose NOACs gradually increased from 57.5% to 81.4%. This pattern might reflect the concerns of major bleeding in using TAT with regular-dose NOACs. Except apixaban, the concentration of active metabolites of NOACs was different according to the races (Figure 1). East Asian patients had more major bleeding risks with relatively low concentrations of NOACs compared with Caucasians.4) An interesting finding of the present study was that the proportion of ticagrelor among P2Y12 receptor inhibitors has been substantially increased. However, it is difficult to deduce from this dataset whether ticagrelor prescription was part of DAPT or TAT. Because factors favoring DAPT in the present study were also high-risk factors for future arterial vascular events requiring potent P2Y12 receptor inhibitors (poly-vascular disease, MI) and high-risk factors for bleeding events (female sex, renal disease, history of intracranial bleeding), ticagrelor might be prescribed as a DAPT in patients with acute MI or complex coronary lesions. According to the Korea Acute Myocardial Infarction Registry-National Institutes of Health in Dual Anti-Platelet Therapy (KAMIR-NIH-DAPT) score, the presence of AF increased the ischemic risks in patients with acute MI. But bleeding hazards were outweighed the ischemic benefits when using OAC additionally to DAPT in this population (Figure 1). Therefore, clopidogrel is a more reasonable choice than ticagrelor for P2Y12 receptor inhibition when considering TAT in AF patients after PCI.5)
The default strategy in current guidelines is a dual antithrombotic therapy (DAT) including NOAC plus clopidogrel after a short period (within 1 week) of TAT based on well-designed randomized controlled trials (RCTs).6) TAT is recommended for up to 1 month in patients with high coronary ischemic risk. The discriminating point from the previous guidelines is the duration of TAT. Current guideline recommendations are deemed feasible when considering the results of recent studies. Ischemic events after PCI might decrease markedly over time with 1 week and 1 month as a turning point,7) and inhibition of factor Xa or thrombin by NOACs have a role in preventing atherothrombosis development and progression.8) Benefits of TAT (DAT + aspirin) for reducing stent thrombosis were mostly within the early phase (1 month) in a sub-study of Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation (AUGUSTUS) trial.9)
Although the present study showed dynamic changes in prescription patterns of antithrombotic regimens in large numbers of Korean patients with AF who underwent PCI, there were several critical limitations in the HIRA database to apply these results to clinical practice. First, one of the most important questions regarding the antithrombotic regimen issue is the optimal duration of TAT, as mentioned above. However, it was not possible to find out dynamic changes of antithrombotic regime within 1 month after PCI. The authors defined the antithrombotic group as the maximum combination in the present study. Therefore, patients who had changed from TAT to DAT or DAPT within 1 month after PCI were regarded as the TAP group. Second, the main advantage of a real-world database over RCT is to evaluate the clinical impact of un-established therapies. However, the present study database could not provide clinical outcomes of each regimen such as off-label reduced-NOAC-based regimen and DAPT with potent P2Y12 receptor inhibitors. Third, information about coronary artery lesions is important to assess the peri-procedural antithrombotic regimen. Except early cessation of DAPT, the major predictors of early stent thrombosis were peri-procedural coronary artery lesion factors including incomplete apposition of stent, plaque prolapse, and flow limiting coronary artery dissection (Figure 1).10) Despite some limitations, the present study could be the starting point for the journey to find the optimal antithrombotic regimen in Korean patients with AF after PCI.
Notes
Funding: This study was supported by research funds from the Basic Science Research Program through the National Research Foundation of Korea (NRF-2018R1D1A1B07040783).
Data Sharing Statement: The data generated in this study is available from the corresponding author upon reasonable request.
The contents of the report are the author's own views and do not necessarily reflect the views of the Korean Circulation Journal.
Go to : 
References
1. Joung B, Lee JM, Lee KH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018; 48:1033–1080. PMID: 30403013.

2. Choi HI, Ahn JM, Kang SH, et al. Prevalence, management, and long-term (6-year) outcomes of atrial fibrillation among patients receiving drug-eluting coronary stents. JACC Cardiovasc Interv. 2017; 10:1075–1085. PMID: 28527773.
3. Kwon S, Jung JH, Choi EK, et al. Impact of non-vitamin K antagonist oral anticoagulants on the change of antithrombotic regimens in patients with atrial fibrillation undergoing percutaneous coronary intervention. Korean Circ J. 2021; 51:409–422.

4. Kim HK, Tantry US, Smith SC Jr, et al. The East Asian paradox: an updated position statement on the challenges to the current antithrombotic strategy in patients with cardiovascular disease. Thromb Haemost. 2020; [Epub ahead of print].

5. Lee SH, Kim HK, Jeong MH, et al. Practical guidance for P2Y12 inhibitors in acute myocardial infarction undergoing percutaneous coronary intervention. Eur Heart J Cardiovasc Pharmacother. 2020; [Epub ahead of print].
6. Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2020; [Epub ahead of print].
7. Kupka D, Sibbing D. De-escalation of P2Y12 receptor inhibitor therapy after acute coronary syndromes in patients undergoing percutaneous coronary intervention. Korean Circ J. 2018; 48:863–872. PMID: 30238704.
8. Kim HK, Tantry US, Gurbel PA, Jeong YH. Another unmet need against residual risk of atherosclerotic cardiovascular disease: can “Thrombin Pathway” be a new target for therapy? Korean Circ J. 2020; 50:817–821. PMID: 32812410.

9. Lopes RD, Leonardi S, Wojdyla DM, et al. Stent thrombosis in patients with atrial fibrillation undergoing coronary stenting in the AUGUSTUS trial. Circulation. 2020; 141:781–783. PMID: 31707833.

10. Nakano M, Yahagi K, Otsuka F, et al. Causes of early stent thrombosis in patients presenting with acute coronary syndrome: an ex vivo human autopsy study. J Am Coll Cardiol. 2014; 63:2510–2520. PMID: 24768883.
Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download