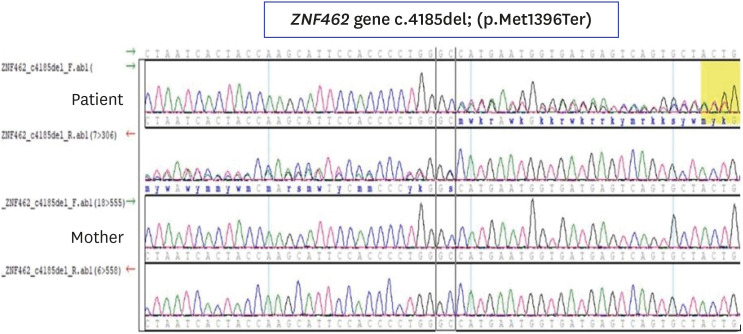
1. González-Tarancón R, Salvador-Rupérez E, Miramar Gallart MD, Barroso E, Díez García-Prieto I, Pérez Delgado R, et al. A novel mutation in the ZNF462 gene c.3306dup; p.(Gln1103Thrfs*10) is associated to Weiss-Kruszka syndrome. A case report. Acta Clin Belg. 2020; 1–4.
2. Kruszka P. Weiss-Kruszka syndrome. In : Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mirzaa G, editors. GeneReviews®. Seattle, WA: University of Washington;1993.
3. Nagase T, Nakayama M, Nakajima D, Kikuno R, Ohara O. Prediction of the coding sequences of unidentified human genes. XX. The complete sequences of 100 new cDNA clones from brain which code for large proteins in vitro. DNA Res. 2001; 8(2):85–95. PMID:
11347906.

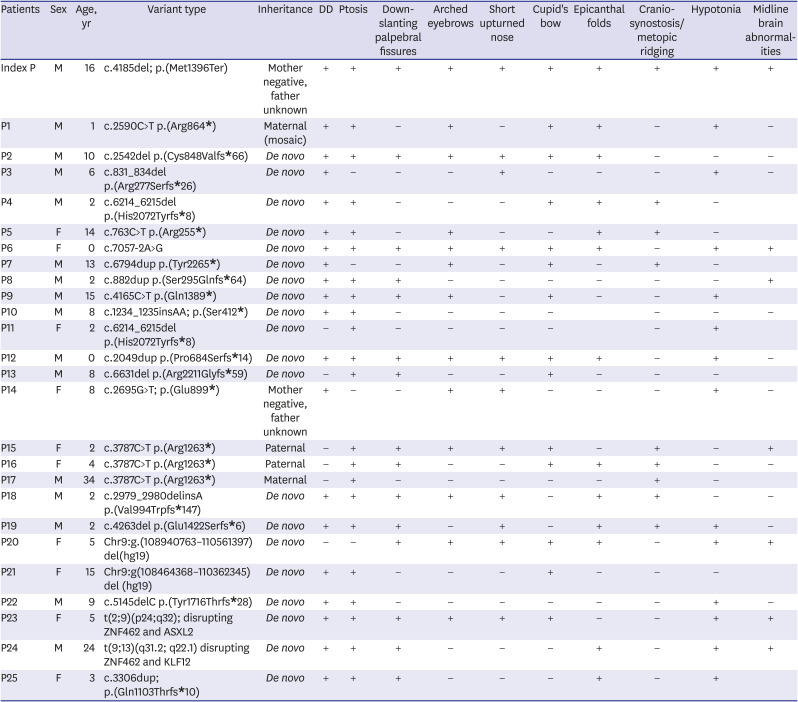
4. Weiss K, Wigby K, Fannemel M, Henderson LB, Beck N, Ghali N, et al. Haploinsufficiency of ZNF462 is associated with craniofacial anomalies, corpus callosum dysgenesis, ptosis, and developmental delay. Eur J Hum Genet. 2017; 25(8):946–951. PMID:
28513610.

5. Uliana V, Percesepe A. Reverse phenotyping comes of age. Mol Genet Metab. 2016; 118(4):230–231. PMID:
27211610.

6. Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17(5):405–424. PMID:
25741868.

7. Cosemans N, Vandenhove L, Maljaars J, Van Esch H, Devriendt K, Baldwin A, et al. ZNF462 and KLF12 are disrupted by a de novo translocation in a patient with syndromic intellectual disability and autism spectrum disorder. Eur J Med Genet. 2018; 61(7):376–383. PMID:
29427787.

8. Kruszka P, Hu T, Hong S, Signer R, Cogné B, Isidor B, et al. Phenotype delineation of ZNF462 related syndrome. Am J Med Genet A. 2019; 179(10):2075–2082. PMID:
31361404.
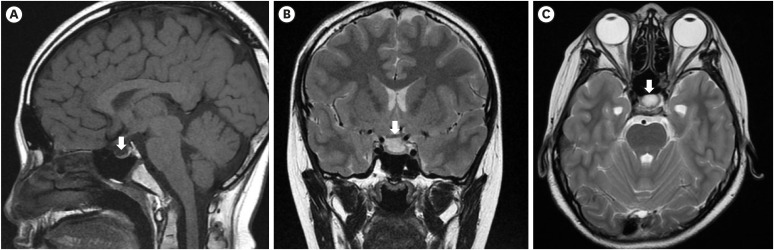
9. Nowick K, Gernat T, Almaas E, Stubbs L. Differences in human and chimpanzee gene expression patterns define an evolving network of transcription factors in brain. Proc Natl Acad Sci U S A. 2009; 106(52):22358–22363. PMID:
20007773.

10. De Marinis L, Bonadonna S, Bianchi A, Maira G, Giustina A. Primary empty sella. J Clin Endocrinol Metab. 2005; 90(9):5471–5477. PMID:
15972577.

11. Lee SS, Han AL, Ahn MB, Kim SH, Cho WK, Cho KS, et al. Growth without growth hormone in combined pituitary hormone deficiency caused by pituitary stalk interruption syndrome. Ann Pediatr Endocrinol Metab. 2017; 22(1):55–59. PMID:
28443260.

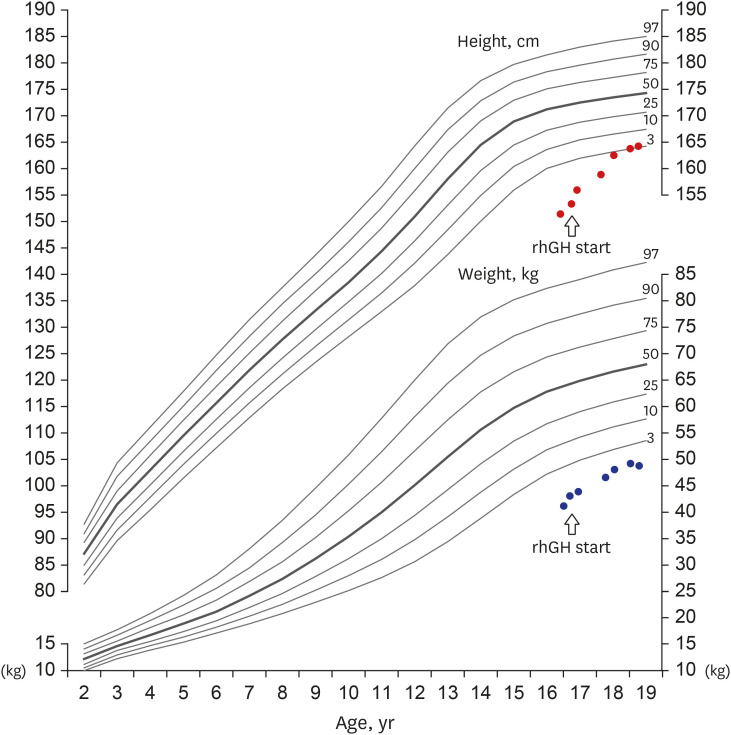
12. Son HW, Lee JE, Oh SH, Keum C, Chung WY. Effects of long-term growth hormone therapy in a girl with Floating-Harbor syndrome. Ann Pediatr Endocrinol Metab. 2020; 25(2):126–131. PMID:
32615693.

13. Chiloiro S, Giampietro A, Bianchi A, Tartaglione T, Capobianco A, Anile C, et al. Diagnosis of endocrine disease: primary empty sella: a comprehensive review. Eur J Endocrinol. 2017; 177(6):R275–85. PMID:
28780516.

14. Hayakawa K, Konishi Y, Matsuda T, Kuriyama M, Konishi K, Yamashita K, et al. Development and aging of brain midline structures: assessment with MR imaging. Radiology. 1989; 172(1):171–177. PMID:
2740500.

15. Al-Naama N, Mackeh R, Kino T. C
2H
2-type zinc finger proteins in brain development, neurodevelopmental, and other neuropsychiatric disorders: systematic literature-based analysis. Front Neurol. 2020; 11:32. PMID:
32117005.

16. Krishna SS, Majumdar I, Grishin NV. Structural classification of zinc fingers: survey and summary. Nucleic Acids Res. 2003; 31(2):532–550. PMID:
12527760.






 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download