This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Epidemiological data are crucial in designing policies for the control of human immunodeficiency virus (HIV) infections. There is a lack of data on the epidemiology of HIV in Korean correctional facilities such as jails and prisons.
Methods
Clinical characteristics of the study population were collected through a medical record review.
Results
The number of people with HIV infection were 83 and the HIV infection prevalence in correctional facilities of Korea was 0.15%. Among them, 10 (12.0%) were diagnosed with the infection when they were incarcerated. The number of drug users was 38 (45.8%). Syphilis-HIV coinfection was observed in 21 (25.3%) patients. Individuals from the group comprising the drug users were more likely to belong to the lesbian, gay, bisexual, transgender, queer (LGBTQ) community, and had a higher incidence of psychological disorders (31.6% vs. 11.1%, P = 0.029; 50.0% vs. 28.9%, P = 0.049, respectively).
Conclusion
Inmates of correctional facilities showed a five times higher prevalence of HIV infection in Korea, nearly half of whom were drug users.
Keywords: HIV, Prevalence, Prisons, Drug Users, Republic of Korea, Epidemiology
INTRODUCTION
Human immunodeficiency virus (HIV) infection in correctional facilities (jails and prisons) is a major health care issue.
1 The prevalence of HIV infection among people in correctional facilities is three to five times higher than that among the general population because many inmates engage in high-risk behaviors such as injection drug use or sex work.
2 Although mandatory HIV screening among inmates is conducted in the Republic of Korea, clinical information about these individuals is insufficient. Due to the limitation on the access to data on inmates, there is a lack of information on the HIV infection prevalence among jail inmates in Korea.
Local data on the prevalence and characteristics of people living with HIV (PLHIV) in correctional facilities are crucial to determine the implementation of specific methods and scale of policies. This study aimed to describe the characteristics of PLHIV in Korean correctional facilities.
METHODS
Study design
This study is a cross-sectional study in nature. All HIV-positive inmates with available records at October 6, 2020 (n = 58) from a total of 52 correctional facilities (jails and prisons) in Korea were included in this study. In Korea, all individuals admitted into jails or prisons undergo mandatory HIV and syphilis screening at the time of admission. Blood test results are recorded on a unified electronic health record system (called Boramee) across the country and is reported to the Korea Correctional Service governed by the Ministry of Justice.
Clinical information such as sex, age, age at diagnosis of HIV infection, nationality, sexual orientation, drug use, concomitant diseases including syphilis, hepatitis B virus (HBV)/hepatitis C virus (HCV) infections, tuberculosis, and psychiatric diseases was collected. For syphilis, when an inmate enters the correctional facility, he/she is asked about syphilis diagnosis or treatment history and got qualitative Rapid Plasma Reagin (RPR) test. When the result is positive, further treponemal tests are done for diagnosis. For tuberculosis, every inmate is asked about his/her history of tuberculosis. Also, chest X-ray is taken and read by board-certified radiologists. The number of inmates diagnosed with HIV infections at the time of incarceration was noted. The study population was divided into two groups according to drug use. The clinical characteristics of these two groups were compared.
Statistical analysis
An independent samples t-test was used to compare the mean values of continuous variables, and Pearson's χ2 test or Fisher's exact test was used for categorical variables. A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 26.0 (IBM Corp., Armonk, NY, USA).
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Boramae Medical Center (IRB No.: 30-2020-239). The board waived the requirement for informed consent due to the retrospective nature of this study, causing insignificant levels of harm to the study population.
RESULTS
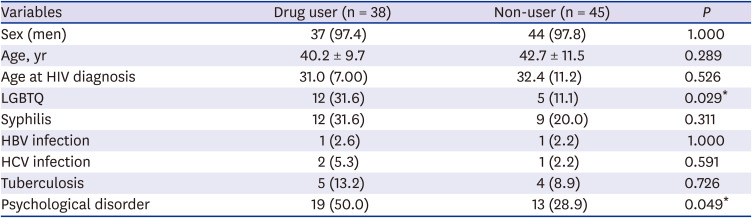
Of the 55,000 inmates, 83 had HIV infection. There were 81 (97.6%) men, and the average age was 41.6 years (
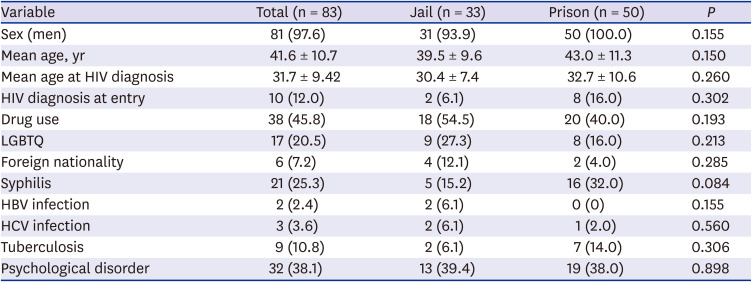
Table 1). With respect to the type of facility, 33 (39.8%) were incarcerated in jails and 50 (60.2%) were incarcerated in prisons. The average age at diagnosis of HIV infection was 31.7 years, and 10 (12.0%) inmates were diagnosed when they were incarcerated. The number of drug users was 38 (45.8%); however, we could not define the nature of the drugs due to a lack of records. The number-of LGBTQ patients was 17 (20.5%). Syphilis-HIV coinfection was observed in 21 (25.3%) patients. Regarding nationality, 5 patients had a foreign nationality, and 1 patient was from North Korea. Thirty-two patients (37.3%) were diagnosed with psychological disorders. Among them, 13 (15.5%) were diagnosed with depression, 5 (6.0%) with panic disorder, and 4 (4.8%) with schizophrenia. Regards to the category of facilities, syphilis-HIV coinfection was more frequent as 32.0% in prison group than 15.2% in jail group, but it did not show statistical difference. The number of HIV diagnosis at entry was identified were more prevalent in prison as 16.0% than 6.1% in jail, without significant difference, either. The study population's tuberculosis was diagnosed as latent or treated at the time of data collection. There was no active tuberculosis at the time study.
Table 1
Characteristics relevant to HIV infection in Korean prison and jail inmates
|
Variable |
Total (n = 83) |
Jail (n = 33) |
Prison (n = 50) |
P
|
|
Sex (men) |
81 (97.6) |
31 (93.9) |
50 (100.0) |
0.155 |
|
Mean age, yr |
41.6 ± 10.7 |
39.5 ± 9.6 |
43.0 ± 11.3 |
0.150 |
|
Mean age at HIV diagnosis |
31.7 ± 9.42 |
30.4 ± 7.4 |
32.7 ± 10.6 |
0.260 |
|
HIV diagnosis at entry |
10 (12.0) |
2 (6.1) |
8 (16.0) |
0.302 |
|
Drug use |
38 (45.8) |
18 (54.5) |
20 (40.0) |
0.193 |
|
LGBTQ |
17 (20.5) |
9 (27.3) |
8 (16.0) |
0.213 |
|
Foreign nationality |
6 (7.2) |
4 (12.1) |
2 (4.0) |
0.285 |
|
Syphilis |
21 (25.3) |
5 (15.2) |
16 (32.0) |
0.084 |
|
HBV infection |
2 (2.4) |
2 (6.1) |
0 (0) |
0.155 |
|
HCV infection |
3 (3.6) |
2 (6.1) |
1 (2.0) |
0.560 |
|
Tuberculosis |
9 (10.8) |
2 (6.1) |
7 (14.0) |
0.306 |
|
Psychological disorder |
32 (38.1) |
13 (39.4) |
19 (38.0) |
0.898 |
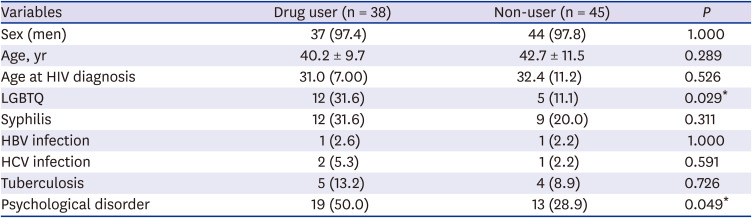
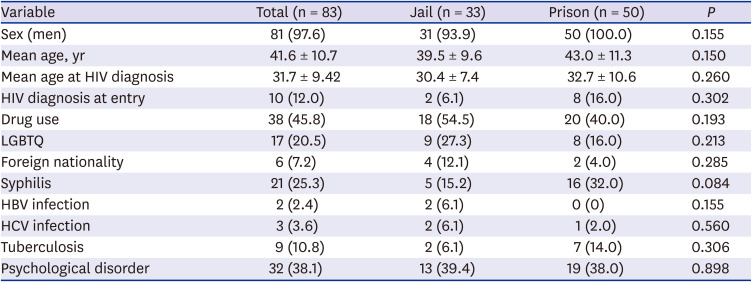
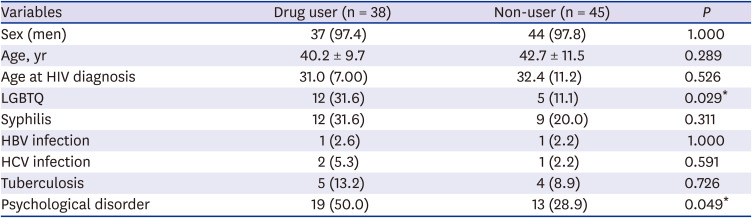
When comparing drug users and non-users (
Table 2), a higher proportion of LGBTQ individuals were among drug users than among non-users (31.6% vs. 11.1%,
P = 0.029). A higher proportion of drug users had psychological disorders (50.0% vs. 28.9%,
P = 0.049). Among other bloodborne infections, drug users had a higher proportion of syphilis than non-users, but the difference was not significant. The number of hepatitis B and hepatitis C patients was insignificant at 1–2 individuals; hence, our study was limited in terms of the ability to compare this aspect between groups.
Table 2
Comparison of people living with HIV infection according to drug usage
|
Variables |
Drug user (n = 38) |
Non-user (n = 45) |
P
|
|
Sex (men) |
37 (97.4) |
44 (97.8) |
1.000 |
|
Age, yr |
40.2 ± 9.7 |
42.7 ± 11.5 |
0.289 |
|
Age at HIV diagnosis |
31.0 (7.00) |
32.4 (11.2) |
0.526 |
|
LGBTQ |
12 (31.6) |
5 (11.1) |
0.029*
|
|
Syphilis |
12 (31.6) |
9 (20.0) |
0.311 |
|
HBV infection |
1 (2.6) |
1 (2.2) |
1.000 |
|
HCV infection |
2 (5.3) |
1 (2.2) |
0.591 |
|
Tuberculosis |
5 (13.2) |
4 (8.9) |
0.726 |
|
Psychological disorder |
19 (50.0) |
13 (28.9) |
0.049*
|
DISCUSSION
This study elucidated basic clinical data on the characteristics of incarcerated PLHIV in the Republic of Korea. We confirmed 83 PLHIV among all inmates in Korea. Although difficult to define due to continuous admissions and releases, approximately 54,000 inmates are incarcerated in Korea everyday.
3 Thus, the prevalence of HIV infection in correctional facilities in Korea is 0.15%. Compared to the overall HIV infection prevalence of approximately 0.027% in Korea,
4 this value is more than 5 times higher. The high prevalence of HIV infection observed in our study is consistent with those of other countries.
5 High-risk behaviors such as sharing of used needles, unprotected sex, sexual violence, and lack of access to comprehensive HIV prevention programs are possible causes of the high prevalence of HIV among this population.
Drug users were found in almost half of the study population. This rate is high, especially considering that all categories of drugs including marijuana are illegal in Korea. It was reported that about 5.8% (1,996/34,697) of all prisoners (both PLHIV and non-PLHIV, excluding jail inmates) were drug users in 2019. Compared to the results of our study as the prevalence among PLHIV in prison (40%, 20/50), the prevalence of drug users of PLHIV prisoner is much higher than non-PLHIV prisoner. Injection drug users are the dominant risk group for an HIV infection.
5 These results suggest that drug users should receive special attention in terms of HIV prevention and control strategies of Korea.
The proportion of LGBTQ individuals was 20.5% of the PLHIV in our results, which is lower than the previous report of 60.1% in the Korea HIV/AIDS Cohrs Study.
6 It is possible that the proportion of LGBTQ in our study has been underestimated because this information was obtained through interviews with officials in correctional facilities at the time of admission. Regarding syphilis, a previous study using national claims database showed that almost half of Korean PLHIV had syphilis coinfection (48.3%).
7 The prevalence of syphilis coinfection was lower as 31.6% in drug users and 20.0% in non-users in our results. The lower prevalence of syphilis coinfection among the inmate population might provide insights because needle sharing is a well-known transmission route of HIV infection, while syphilis is rarely transmitted through a needle.
8 However, we could not identify if the category of drug was injectable drug or if drug users had significantly less syphilis coinfection through this study. In addition, about half of the drug users claimed that they had concurrent psychiatric diseases, which comprises a higher proportion than the proportion of non-drug users. While this could be due to psychiatric side-effects of drugs, it is also possible that this reflects their drug-seeking behaviors for sedative or stimulative effects.
Although the number of new HIV infections has been decreasing since 1996 globally,
9 that of the Republic of Korea has increased steadily.
4 The diagnosis rate estimated in Korea is about 64%, which is lower than the Joint United Nations Programme on HIV and AIDS (UNAIDS) target of 90%.
10 This study is valuable and meaningful as it is the first Korean study to describe the status of HIV infections among the high-risk group of incarcerated individuals in correctional facilities. Individuals who are incarcerated are tested and receive antiretroviral treatment if he or she is infected with HIV in Korea. However, a more systematic screening that includes records of intravenous drug usage and coinfection with HBV or HCV will enable the establishment of an evidence-based HIV infection prevention and treatment plan in the future. In addition, ensuring that prisoners have access to HIV care (medications) after release can be a key strategy in risk reduction for the entire population, as former inmates may continue their high-risk lifestyle.
This study is limited in its retrospective nature. Vital clinical information can be missed in records, and variables were underestimated. We could not find the treatment progress in this study, however we believe that it is worthy as an insightful description of the people infected with HIV in correctional facilities in Korea.
In conclusion, inmates of correctional facilities in Korea showed a higher prevalence of HIV infection than the general community, among whom a higher prevalence was observed among drug users. A substantial proportion of HIV patients were diagnosed with the infection only at the time of admission.