INTRODUCTION
The association between neonatal mortality and time of birth has been well studied.
12345678910111213 The incidence of night, weekend, or holiday births ranged from 27.7%–65% in other countries.
2345813 Some studies have shown an increased risk of early neonatal mortality for nighttime and weekend births,
2589 but the results are not consistent.
37 The reasons for this variation could be attributed to a difference in the physician’s availability and expertise in the neonatal intensive care unit (NICU), and the circadian rhythm affecting human alertness and work performance.
29 This result has raised concern about differences in the quality of care based on the time of birth; however, there have been no studies reporting such data in Korea. Thus, the purpose of this study was to investigate the time of birth and its association with early neonatal mortality and morbidities in Korea. The data were collected from the National Registry data, Korean Neonatal Network (KNN).
14
In this study, we compared the risk-adjusted early neonatal mortality rates and major morbidities between extremely low birth weight infants (ELBWIs) at less than 35 weeks of gestation admitted during off-hours (nighttime, weekend, and public holidays) and those admitted during regular hours to NICUs in Korea from 2013 to 2017. Furthermore, after we sub-grouped institutes based on the NICU care level, which was defined by the mortality rate of infants born at 23–24 weeks (< or ≥ 50%),
1516 we compared the outcomes according to the time of birth between the two groups.
METHODS
Study population
We included ELBWIs born between 23 weeks 0 days and 34 weeks 6 days of gestation, who were enrolled in the database registry of the KNN from January 2013 to December 2017. The database registry of the KNN prospectively registered the clinical information of very low birth weight infants (VLBWIs) admitted to the 70 voluntarily participating NICUs, covering > 70% of VLBWIs in Korea.
14 VLBWIs who were actively resuscitated in the delivery room and admitted to the NICU were registered in the KNN. The KNN registry was approved by the Institutional Review Board of each participating hospital.
We collected data of 3,817 ELBWIs born at 23–34 weeks of gestation during the study period. To reduce skewing of the study outcomes, infants with out-born birth (birth from another institution or home delivery) (n = 138), transferred to another hospital (n = 268), having life-threatening congenital anomalies (n = 103), and missing data regarding the time of birth (n = 14) were excluded. As we sub-grouped institutes by the NICU care level, defined by the mortality rate of infants born at 23–24 weeks, we excluded 74 infants from institutes without preterm deliveries between 23 and 24 weeks of gestation. Thus, the remaining 3,220 infants were included.
Data collection
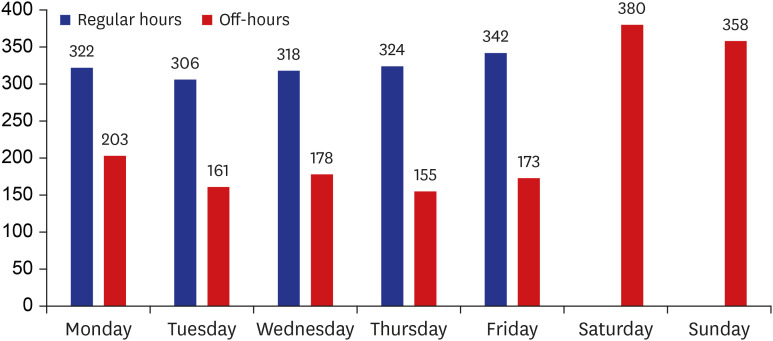
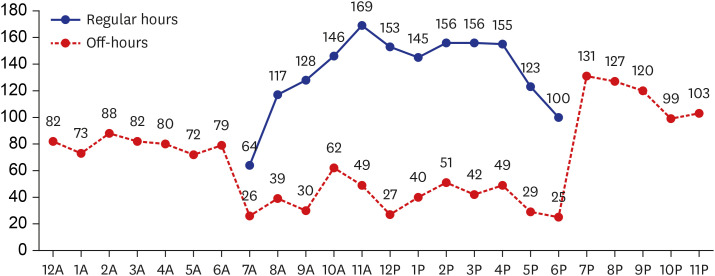
We operationally defined the regular hours and off-hours. Regular-hour birth was defined as birth from 7:00 am to 6:59 pm Monday to Friday, excluding national holidays in the Republic of Korea. Off-hour birth was defined as birth at any time other than the defined regular hours, i.e., from 7:00 pm Monday to Friday to 6:59 am the following day, and from 7:00 am on a weekend or national holiday to 6:59 am the next day.
We also sub-grouped hospitals according to their NICU care level, defined by the mortality of infants born at 23–24 weeks of gestation. The median mortality rate of peri-viable infants born at 23–24 weeks of gestation was approximately 50% in the KNN data, and based on this, there were previous studies comparing of clinical outcome after subgrouping by mortality rate, 50%.
1516 Hospital group I included institutes with < 50% mortality rate, while hospital group II included institutes with a ≥ 50% mortality rate in infants born at 23–24 weeks of gestation.
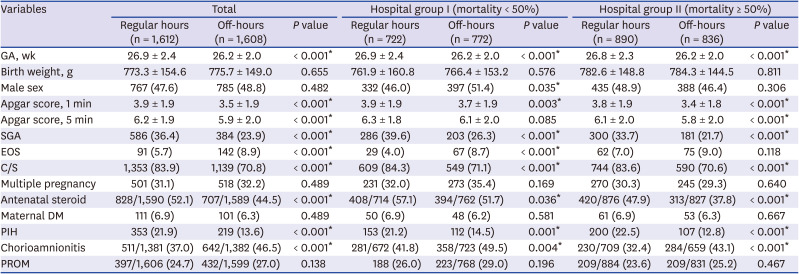
We compared maternal and neonatal variables, including gestational age (GA), birth weight, sex, Apgar scores at 1 and 5 minutes, small for gestational age (SGA), early onset sepsis (EOS), mode of delivery, maternal diabetes, pregnancy-induced hypertension (PIH), chorioamnionitis, premature rupture of membranes (PROM), and antenatal steroid between the regular and off-hour births in hospital groups I and II.
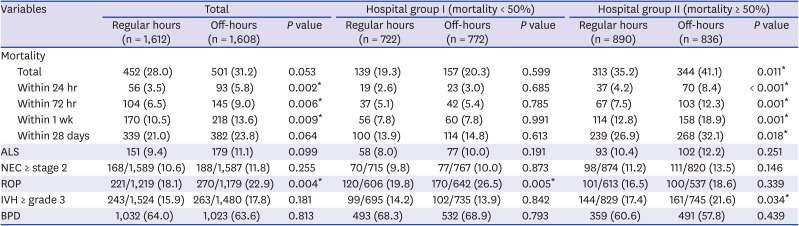
The outcome variable was death of an infant before discharge (within approximately 24 hours, 72 hours, 1 week, and 28 days after birth, and total mortality rates). We also compared various major morbidities, including air leak syndrome (ALS), necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), intraventricular hemorrhage (IVH), and bronchopulmonary disease (BPD) between regular and off-hour births in hospital groups I and II.
Definitions
The following definitions of the aforementioned terminologies were used in this study. SGA was defined as birth weight < 10th percentile for GA with reference to the pediatric growth chart released in 2017 by the Korean Centers for Disease Control and Prevention. EOS was defined as a positive blood culture obtained before postnatal day 7. Chorioamnionitis was confirmed by placental pathology, and PROM was defined as rupture of membranes over 24 hours before the onset of labor. Antenatal steroid was defined as administration of a complete course of steroid to the mother, such as two doses of betamethasone or four doses of dexamethasone every 24 hours within a week of delivery. ALS was defined as radiologic findings of extrapulmonary air requiring chest tube insertion and drainage. NEC was defined as stage ≥ 2 according to the modified Bell criteria.
17 ROP was defined as severe ROP leading to the need for surgery. IVH was defined as grade 3 or 4 according to the classification of Papile et al.
18 BPD was defined as the use of supplemental oxygen or respiratory support at postnatal day 28 or more.
Statistical analysis
The statistical software Statistical Package for the Social Sciences version 25 (SPSS, IBM Corp., Armonk, NY, USA) was used for data analysis. We used the chi-square test to compare the differences in clinical characteristics for categorical variables, while the independent t-test was used to analyze continuous variables. Factors with P value < 0.05 at univariate analysis were included in the logistic regression models to determine the association between time of birth and the risk of neonatal mortality and morbidities. The adjusted odds ratio and 95% confidence interval for each possible risk factor were calculated. A P value < 0.05 was considered statistically significant.
Ethics statement
The KNN registry was approved by the Institutional Review Board (IRB) of each participating hospital. Informed consent was obtained from the parents during enrollment by the NICUs participating in the KNN. All methods were conducted in accordance with the IRB-approved guidelines and protocol.
DISCUSSION
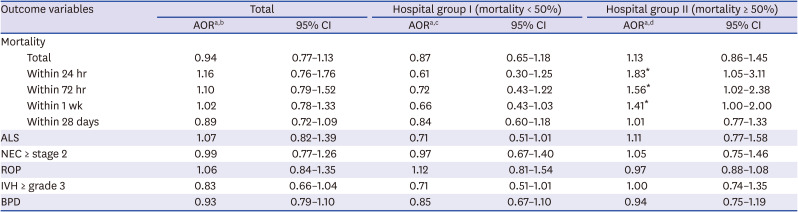
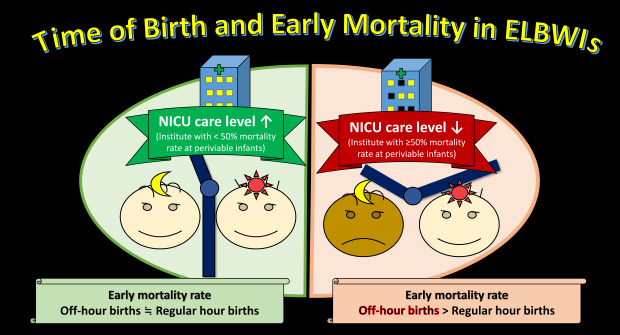
We investigated the number of ELBWIs born at 23 weeks 0 days to 34 weeks 6 days of gestation during regular hours and off-hours in Korea based on KNN data and found that the numbers were similar (50.06% vs. 49.94%). After adjusting for multivariate analysis, we found that lower quality NICUs, i.e., institutes with ≥ 50% mortality rate in infants born at 23–24 weeks' gestation, showed increased early mortality rates in off-hour births than in regular-hour births.
To our knowledge, this is the first study that analyzed mortality by birth time using a national registry in Korea. This study has demonstrated that birth time influences the outcome of ELBWIs admitted to NICUs in Korea. We did not investigate whether the delivery was elective or emergency; however, a previous study found that infants born during regular hours were more likely to have had an elective delivery.
3 This was further associated with infants showing an antenatal diagnosis of growth restriction and maternal PIH. In addition, infants born during off-hours were more likely to have had a less planned birth, as indicated by the lower rates of complete use of antenatal steroids and lower Apgar scores. This is consistent with other literature findings.
19
The results of our study are contradictory to those of some international studies. Abdel-Latif et al.
3 categorized admission time as regular hours (8:00 am to 6:00 pm, Monday to Friday, excluding public holidays). They found that admission to the NICU during off-hours did not have a significant impact on early neonatal mortality. This could be attributed to the even distribution of on-floor NICU resident medical staff working around a structured shift roster, causing less fatigue in the staff. Gould et al.
7 reported that there was no significant difference in the mortality rate among infants born on weekends and those born on weekdays in California, thus concluding that the quality of perinatal care was not compromised during the weekend. However, they did not investigate and control demographic factors that could have affected the results.
On the contrary, Luo and Karlberg
5 reported higher mortality in infants who were born during the night (9:00 pm to 9:00 am). Lee et al.
2 found that the risk-adjusted early neonatal mortality (death within 7 days of NICU admission) odds were 60% higher among inborn infants ≤ 32 weeks of gestation and admitted to NICUs at night (6:00 pm to 8:00 am). Results similar to our study were found in the aforementioned studies even though the definition of “off-hours” varied.
689 The researchers speculated that the following factors could contribute to the increased mortality in nighttime or weekend births: decreased number of neonatologists and house staff (fellows, pediatric residents, clinical assistants, or neonatal nurse practitioners) at night, difference in physician availability and expertise, and variation in circadian rhythm affecting human alertness and work performance.
27 However, we did not have data to compare the availability and experience of the medical staff between the off-hours and regular hours.
We considered the level of neonatal care provided by the birth hospital, which is indicative of the mortality risk in infants born at night, to be influenced by hospital characteristics.
4 In previous studies, wide institutional variations were evident regarding the mortality of infants born at 23–24 weeks' gestation.
1516 After categorizing infants into two groups based on institutional mortality rates of < 50% (hospital group I) and ≥ 50% (hospital group II) in this study, we compared the mortality according to the birth time stratified by the group.
There was little difference in the extent of disadvantage seen between off-hour births and regular-hour births in hospital group I, but early mortality was higher in off-hour births than in regular-hour births in hospital group II. This suggests that birth time was an important factor at the institute with higher mortality rates of periviable extremely preterm infants.
The incidence of ROP and BPD in hospital group I was significantly higher than hospital group II. Since the mortality rate in hospital group I was lower than hospital group II (19.8% vs. 38.1%), it is considered that complications related to long-term treatment and survival, such as BPD and ROP, were more developed in hospital group I.
The inevitable limitation of this study stems from the none of collected data on the differences between these two hospital groups. Therefore, additional information regarding the patient and staff volume, institutional level, staff workload, work shift, and level of hospital care for each group is needed. It is necessary to examine the impact of the level of care and access to diagnostic and therapeutic services, including obstetrics, anesthesiology, and radiology in each group.
Admission is the most vulnerable period for seriously ill infants, and early mortality is associated with this period. There is a difference in early mortality rate between off-hour and regular-hour births depending on the quality of care; therefore, efforts to improve the overall quality of NICU are required and other sensitive indexes for the evaluation of quality of NICU care should be further studied. Also, it should be a priority for perinatal care to identify causal factors of mortality in off-hour births and reduce mortality rates. The early mortality rate in off-hour births can be lowered by expansion and proper allocation of healthcare workers and infrastructure, and close cooperation between obstetricians and neonatologists.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download