Abstract
Background
Radiotherapy is often used for treating patients with gastric mucosa-associated lymphoid tissue (MALT) lymphomas who fail to respond to Helicobacter pylori eradication. However, non-gastric intestinal MALT lymphoma is rare, and no standard therapeutic strategies have been established. This study was designed to assess the long-term prognosis of non-gastric intestinal MALT lymphoma treated with radiotherapy and to compare the outcomes with that of post-radiotherapy gastric MALT lymphoma.
Methods
The study included 34 patients with stage I EA gastrointestinal MALT lymphoma according to the Ann Arbor classification who underwent definitive radiotherapy. The primary site was the rectum in 3, the duodenum in 1, and the stomach in 30 patients. The radiotherapy dose was 1.5‒2.0 Gy (median, 1.5 Gy) and the total dose was 30‒40 Gy (median, 30 Gy). The clinical target volume (CTV) was defined as the volume of the entire organ with the lymphoma. Adjacent lymph node areas were not routinely included in the CTV.
Results
Complete response (CR) was achieved in all patients. There were no local recurrences, and two cases of recurrence were observed at other sites. The 5-year overall survival rates for non-gastric and gastric MALT lymphomas were 100% and 94.7%, respectively, and the 5-year disease-free survival rates were 100% and 95.7%, respectively. None of the patients died of the current illness.
The gastrointestinal tract is the most common extranodal site of non-Hodgkin’s lymphoma (NHL). Primary gastrointestinal NHL is a rare disease accounting for 10–15% of all NHLs and 30–40% of extranodal NHLs. The gastrointestinal tract may present with a diverse group of lymphoid neoplasms, most of which are of B-cell lineage [1, 2]. Marginal zone lymphoma (MZL) is an indolent, mature B-cell neoplasm. Extranodal MZL of the mucosa-associated lymphoid tissue (MALT) type, in addition to nodal MZL and splenic MZL, is a type of MZL recognized by the World Health Organization (WHO) [3]. Due to the accumulation of B-cells associated with chronic inflammation, MALT lymphoma develops in organs that normally lack lymphoid tissue such as the stomach, lung, ocular adnexa, and salivary glands. This chronic inflammation is attributable to either chronic infection or autoimmune processes [4].
Non-gastric intestinal MALT lymphoma is a rare disease, and in the absence of established standard treatment guidelines, radiotherapy (RT), chemotherapy, surgery, and immunotherapy have all been performed for management [5].
A systematic review revealed that 77.5% of 1408 stage I/II low-grade gastric MALT lymphoma patients treated with Helicobacter pylori (H. pylori) eradication achieved complete response (CR). Therefore, eradication of H. pylori is now considered the first-line treatment for gastric MALT lymphoma [6]. However, the standard treatment for residual disease after eradication of H. pylori has not been established, and RT, chemotherapy, surgery, and endoscopic resection have been performed [7].
Moderate-dose RT is an effective treatment for gastric and non-gastric intestinal MALT lymphoma, with only mild adverse events [8, 9]. However, the long-term prognosis after RT is unclear due to limited published case reports [10, 11].
This study was therefore designed to assess the long-term prognosis of non-gastric intestinal MALT lymphoma after RT and to compare the outcomes with that of post-RT gastric MALT lymphoma.
In this retrospective study, we reviewed the medical records of 36 patients who received definitive RT for primary gastrointestinal MALT lymphoma between January 2000 and March 2019 at the Yokohama City University Medical Center. All patients had a confirmed histopathological diagnosis aided by necessary immunostaining for a panel of markers such as CD20, CD10, and CD79a. All patients had stage I EA disease according to the Ann Arbor classification [12] and stage I disease according to Lugano staging of primary gastrointestinal malignant lymphomas [13].
Two patients with gastric MALT lymphoma received induction chemotherapy before RT and were excluded from the analysis. This was because the purpose of this study was to compare the results of RT alone for non-gastric MALT lymphoma with those for gastric MALT lymphoma.
Of the 34 patients, 3 had rectal, 1 had duodenal, and 30 had gastric MALT lymphoma. In general, the treatment strategy followed the guidelines for MALT lymphoma [14, 15].
In all the cases of gastric MALT lymphoma, the presence of H. pylori infection was assessed using multiple methods, such as the urea breath test and the H. pylori antibody test. Among the positive cases, only those that did not respond to eradication therapy and had evidence of residual were treated using RT.
The follow-up time was defined from the date of first RT to the date of death or final confirmation of survival. The median follow-up of the study cohort was 60.5 months (range, 9–136 mo).
Gastrointestinal endoscopy and computed tomography (CT) were performed for pretreatment staging in all patients. 18F-fluorodeoxy glucose- positron emission tomography (FDG-PET) was also performed for staging in 24 patients. Post treatment evaluations were performed every 3 to 6 months, and comprised provisional medical history and physical examination, laboratory tests, gastrointestinal endoscopy, and CT or PET-CT. At each follow-up visit, treatment-related toxicities were assessed and scored according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events version 4.0.
This retrospective study protocol was approved by the Medical Ethics Committee of the Yokohama City University Medical Center (approval no: B170700047) and was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients provided written informed consent for treatment.
All patients received definitive RT. RT was delivered five days per week at daily doses ranging from 1.5 to 2.0 Gy. A total irradiation dose ranging from 30 to 40 Gy (median, 30 Gy) was used. All patients were treated with three-dimensional conformal radiotherapy (3D-CRT). The gross tumor volume (GTV) was defined as the volume corresponding to the lymphoma lesion itself, and the clinical target volume (CTV) was defined as the entire organ with the lymphoma. Adjacent lymph node areas were not routinely included in the CTV. The planning target volume (PTV) was set with an appropriate margin on the CTV, and the irradiation field was set with a leaf margin of 7 mm on the PTV. X-rays at 15 MV were used for treatment. For patients treated after 2017, image-guided RT was performed daily.
During RT, for simulation and treatment, all patients were immobilized in the supine position. For patients with gastric MALT lymphoma, irradiation was performed after fasting for at least 3 hours. Planning CT images were obtained using a LightSpeed RT Scanner (GE Healthcare, Chicago, IL, USA) with a 2.5-mm slice thickness under shallow breathing. During planning for 3D-CRT, contouring of the GTV, CTV, PTV, and organs at risk was performed by radiation oncologists. Dose distributions were calculated using Pinnacle 3 software (Philips, Amsterdam, Netherlands).
The following definitions were used in this study: overall survival (OS) was defined as the period from the first day of RT to the day of death regardless of cause; disease-specific survival was defined as the period from the first day of RT to the day of death due to lymphoma; disease-free survival (DFS) was defined as the period from the first day of RT to the day when a recurrent lesion was confirmed locally or at another site, or the day of death regardless of cause.
As non-gastric MALT lymphoma is a rare disease and it was difficult to collect a sufficient number of cases for statistical comparison with gastric MALT lymphoma, statistical analysis between the two groups was not performed. The Kaplan–Meier method was used to estimate the cumulative incidence of disease recurrence and mortality rate in the two groups. The JMP pro version 15.0 software package (SAS Institute, Tokyo, Japan) was used to calculate the survival rate and create the Kaplan–Meier curve.
This study included 16 men and 18 women, with a median age of 66 years. The performance status of all patients was 0 at the start of RT. At the end of RT, all patients were in complete remission. The detailed characteristics of the two groups are presented in Table 1.
None of the patients with non-gastric intestinal MALT lymphoma were infected with H. pylori. Of the 14 patients with gastric MALT lymphoma who were infected with H. pylori, first-line eradication treatment was successful in 4. Of the remaining 10 patients, second-line eradication therapy was successful in only 5. Several antibiotic regimens have been used for eradication therapy, such as proton pump inhibitors (PPIs) with clarithromycin and amoxicillin as first-line eradication therapy, and PPI with metronidazole and amoxicillin for second-line eradication therapy. Twenty-six patients with gastric MALT lymphoma and 4 patients with non-gastric intestinal MALT lymphoma underwent chromosomal analysis, but no characteristic t(11,18) mutations were detected.
The 5-year OS rates were higher in the non-gastric intestinal MALT lymphoma group than in the gastric MALT lymphoma group (100% vs. 94.7%, Fig. 1). No patients with non-gastric intestinal MALT lymphoma relapsed or died during the observation period. The 5-year DFS rate was higher in the non-gastric intestinal MALT lymphoma group than in the gastric MALT lymphoma group (100% vs. 95.7%, Fig. 2). There was no death of current illness in any of the 34 patients.
There was no recurrence within the entire organ with the lymphoma lesion and adjacent lymph node areas. Two patients with gastric MALT lymphoma had recurrences outside the irradiation field. The details of the two patients who relapsed are shown in Table 2. Of the two relapses, one was MALT and the other was diffuse large B-cell lymphoma (DLBCL). One patient with DLBCL histology at the time of recurrence died. However, the cause of death was respiratory failure.
No radiation-related grade 2 or higher adverse events were noted, and no secondary radiation-induced carcinomas were observed.
There is no universal standard treatment for gastrointestinal MALT lymphoma [5, 7]. The first choice for gastric MALT lymphoma management is H. pylori eradication therapy [14-16]. The significance of eradication therapy for non-gastric intestinal MALT lymphomas is unclear, but there have been reports that rectal MALT lymphomas were eliminated following eradication therapy [17, 18]. The H. pylori positivity rate among patients with gastric MALT lymphoma in this study was lower than that in previous studies [19]. This was possibly because the patients included in this study were only those who received RT after failure to achieve CR by eradication therapy, and patients with CR after eradication therapy were not included.
RT, chemotherapy, and surgery have been used for gastric MALT lymphoma that does not respond to eradication therapy or that recurs after eradication therapy [7]. RT, chemotherapy, surgery, and endoscopic resection have been used for non-gastric intestinal MALT lymphoma [5, 10, 20, 21]. RT is an effective treatment method for gastric and non-gastric intestinal MALT lymphoma with favorable outcomes, with mild, tolerable adverse events reported. Prescription doses, such as 30 Gy/20 Fr, 30 Gy/15 Fr, and 34 Gy/17 Fr, are frequently used for gastric and non-gastric intestinal MALT lymphomas [8, 10, 22]. Recently, there have been reports of low-dose RT using intensity-modulated radiation therapy (IMRT) [23]. Past reports of non-gastric intestinal MALT lymphomas are limited and an appropriate prescribed dose has not yet been established; however, higher doses are more often used for rectal MALT lymphomas than gastric MALT lymphomas [10]. Of the 30 gastric MALT lymphoma patients included in our study, 29 received 30 Gy/20 Fr and one received 40 Gy/20 Fr. Of the 4 non-gastric intestinal MALT lymphoma patients included in our study, 3 received 30 Gy/20 Fr and 1 received 30 Gy/15 Fr. There was no significant difference from the past studies. In our study, local control within the irradiation field was achieved in all patients, which is a good outcome as compared with previous studies.
Several previous studies have evaluated the outcomes of RT for extranodal MALT lymphomas. The 5- and 10-year OS rates were 92–95% and 72–87%, respectively, and the 5- and 10-year DFS rates were 74–82% and 57–76%, respectively [8, 24]. Data on the survival rate of gastrointestinal MALT lymphoma alone are not available. These previous studies suggested that non-gastric MALT lymphomas have a poorer prognosis than gastric MALT lymphomas [8, 24]. On the other hand, in our study, none of the patients with non-gastric intestinal MALT lymphoma developed recurrence or died. Long-term recurrence-free cases have been reported after RT for rectal and duodenal MALT lymphomas [10, 11, 22]. Our study suggests that non-gastric intestinal MALT lymphoma has a similar prognosis to gastric MALT lymphoma. The results of this study, in which non-gastric MALT lymphoma was treated using a total dose of 30 Gy, are comparable or better than those of previous studies. As 25 Gy is frequently used for orbital MALT lymphoma [8] and the irradiation dose for gastric MALT lymphoma can be low [23, 25], the irradiation dose to the duodenum and rectum may be reduced.
As the irradiation dose for MALT lymphoma is approximately 30 Gy to a maximum of 40 Gy, adverse events, such as gastritis and enteritis, can be sufficiently controlled [9]. However, MALT lymphoma often develops in young people, and the risk of carcinogenesis cannot be ignored. Although there are reports of cancer [24], no carcinogenic cases were observed in our study. As the rectum is close to the gonads, care must be exercised in preserving fertility when RT is used for rectal MALT lymphoma. There have been reports of pregnancy and birth following RT for rectal MALT lymphoma [26], and it is possible to achieve both a cure and preservation of fertility by devising irradiation techniques.
To the best of our knowledge, this is the first study to compare the prognosis of radiotherapy for gastric and non-gastric intestinal MALT lymphomas and to demonstrate that the prognosis of non-gastric intestinal MALT lymphoma is not inferior. Although there are limitations due to the small cohort size and observational study design conducted at a single center, the current study suggests that RT for non-gastric intestinal MALT lymphoma results in long-term relapse-free survival. As non-gastric intestinal MALT lymphoma is a rare disease, it is difficult to match the number of cases of gastric MALT lymphoma for statistical analysis and prospective trials may be difficult; therefore, additional studies, such as interventional clinical trials, are necessary for conclusive results.
RT for non-gastric MALT lymphoma provided good local control and long-term survival outcomes, similar to those for post-RT gastric MALT lymphoma. A total irradiation dose of 30 Gy is sufficient for both gastric and non-gastric intestinal MALT lymphomas.
REFERENCES
1. Olszewska-Szopa M, Wróbel T. 2019; Gastrointestinal non-Hodgkin lymphomas. Adv Clin Exp Med. 28:1119–24. DOI: 10.17219/acem/94068. PMID: 31414733.

2. Weindorf SC, Smith LB, Owens SR. 2018; Update on gastrointestinal lymphomas. Arch Pathol Lab Med. 142:1347–51. DOI: 10.5858/arpa.2018-0275-RA. PMID: 30407861.

3. Swerdlow SH, Campo E, Pileri SA, et al. 2016; The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 127:2375–90. DOI: 10.1182/blood-2016-01-643569. PMID: 26980727. PMCID: PMC4874220.

4. Thieblemont C, Bertoni F, Copie-Bergman C, Ferreri AJ, Ponzoni M. 2014; Chronic inflammation and extra-nodal marginal-zone lymphomas of MALT-type. Semin Cancer Biol. 24:33–42. DOI: 10.1016/j.semcancer.2013.11.005. PMID: 24333758.

5. Wöhrer S, Kiesewetter B, Fischbach J, et al. 2014; Retrospective comparison of the effectiveness of various treatment modalities of extragastric MALT lymphoma: a single-center analysis. Ann Hematol. 93:1287–95. DOI: 10.1007/s00277-014-2042-z. PMID: 24633660.

6. Zullo A, Hassan C, Cristofari F, et al. 2010; Effects of Helicobacter pylori eradication on early stage gastric mucosa-associated lymphoid tissue lymphoma. Clin Gastroenterol Hepatol. 8:105–10. DOI: 10.1016/j.cgh.2009.07.017. PMID: 19631287.

7. Thieblemont C, Dumontet C, Bouafia F, et al. 2003; Outcome in relation to treatment modalities in 48 patients with localized gastric MALT lymphoma: a retrospective study of patients treated during 1976-2001. Leuk Lymphoma. 44:257–62. DOI: 10.1080/1042819021000035680. PMID: 12688342.

8. Goda JS, Gospodarowicz M, Pintilie M, et al. 2010; Long-term outcome in localized extranodal mucosa-associated lymphoid tissue lymphomas treated with radiotherapy. Cancer. 116:3815–24. DOI: 10.1002/cncr.25226. PMID: 20564130.

9. Aleman BM, Haas RL, van der Maazen RW. 2010; Role of radiotherapy in the treatment of lymphomas of the gastrointestinal tract. Best Pract Res Clin Gastroenterol. 24:27–34. DOI: 10.1016/j.bpg.2009.12.002. PMID: 20206106.

10. Amouri A, Chtourou L, Mnif L, et al. 2009; MALT lymphoma of the rectum: a case report treated by radiotherapy. Cancer Radiother. 13:61–4. DOI: 10.1016/j.canrad.2008.11.001. PMID: 19101191.
11. Isomoto H, Kamihira S, Matsuo E, et al. 2003; A case of mucosa- associated lymphoid tissue lymphoma of the ampulla of Vater: successful treatment with radiation therapy. Eur J Gastroenterol Hepatol. 15:1037–41. DOI: 10.1097/00042737-200309000-00016. PMID: 12923379.
12. Rosenberg SA, Boiron M, DeVita VT Jr, et al. 1971; Report of the Committee on Hodgkin's Disease Staging Procedures. Cancer Res. 31:1862–3.
13. Rohatiner A, d'Amore F, Coiffier B, et al. 1994; Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 5:397–400. DOI: 10.1093/oxfordjournals.annonc.a058869. PMID: 8075046.

14. Zucca E, Copie-Bergman C, Ricardi U, et al. 2013; Gastric marginal zone lymphoma of MALT type: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 24(Suppl 6):vi144–8. DOI: 10.1093/annonc/mdt343. PMID: 24078657.

15. Dreyling M, Thieblemont C, Gallamini A, et al. 2013; ESMO Consensus conferences: guidelines on malignant lymphoma. part 2: marginal zone lymphoma, mantle cell lymphoma, peripheral T-cell lymphoma. Ann Oncol. 24:857–77. DOI: 10.1093/annonc/mds643. PMID: 23425945.

16. Nakamura S, Sugiyama T, Matsumoto T, et al. 2012; Long-term clinical outcome of gastric MALT lymphoma after eradication of Helicobacter pylori: a multicentre cohort follow-up study of 420 patients in Japan. Gut. 61:507–13. DOI: 10.1136/gutjnl-2011-300495. PMID: 21890816.
17. Nosaka K, Shono T, Yonemura Y, et al. 2014; Regression of primary rectal MALT lymphoma after Helicobacter pylori eradication. Rinsho Ketsueki. 55:948–52. PMID: 25186484.
18. De Sanctis V, Marignani M, Angeletti S, et al. 2012; Anti-Helicobacter pylori therapy in primary MALT lymphoma of rectum. Tumori. 98:e105–10. DOI: 10.1177/030089161209800423. PMID: 23052174.

19. Salar A. 2019; Gastric MALT lymphoma and Helicobacter pylori. Med Clin (Barc). 152:65–71. DOI: 10.1016/j.medcli.2018.09.006. PMID: 30424932.

20. Kajihara Y. 2018; Mucosa-associated lymphoid-tissue (MALT) lymphoma of the rectum. QJM. 111:573. DOI: 10.1093/qjmed/hcy036. PMID: 29474645.

21. Tokura T, Nishikawa S, Umehara M, et al. 2015; A case of MALT lymphoma of the rectum treated with intersphincteric resection (ISR). Gan To Kagaku Ryoho. 42:2265–7. PMID: 26805332.
22. Hayakawa T, Nonaka T, Mizoguchi N, et al. 2017; Radiotherapy for mucosa-associated lymphoid tissue (MALT) lymphoma of the rectum: a case report. Clin J Gastroenterol. 10:431–6. DOI: 10.1007/s12328-017-0769-5. PMID: 28815477.

23. Schmelz R, Miehlke S, Thiede C, et al. 2019; Sequential H. pylori eradication and radiation therapy with reduced dose compared to standard dose for gastric MALT lymphoma stages IE & II1E: a prospective randomized trial. J Gastroenterol. 54:388–95. DOI: 10.1007/s00535-018-1517-4. PMID: 30327875.
24. Teckie S, Qi S, Lovie S, et al. 2015; Long-term outcomes and patterns of relapse of early-stage extranodal marginal zone lymphoma treated with radiation therapy with curative intent. Int J Radiat Oncol Biol Phys. 92:130–7. DOI: 10.1016/j.ijrobp.2015.01.040. PMID: 25863760.

25. Pinnix CC, Gunther JR, Milgrom SA, et al. 2019; Outcomes after reduced-dose intensity modulated radiation therapy for gastric mucosa-associated lymphoid tissue (MALT) lymphoma. Int J Radiat Oncol Biol Phys. 104:447–55. DOI: 10.1016/j.ijrobp.2019.02.002. PMID: 30769175. PMCID: PMC6839887.

26. Hatayama Y, Aoki M, Kawaguchi H, et al. 2017; Safe and successful birth following pelvic radiotherapy for rectal mucosa-associated lymphoid tissue lymphoma: a case report. J Med Case Rep. 11:26. DOI: 10.1186/s13256-016-1193-z. PMID: 28143501. PMCID: PMC5286565.

Fig. 1
The Kaplan–Meier curves for disease-free survival of the 4 non-gastric intestinal and 30 gastric MALT lymphoma patients.
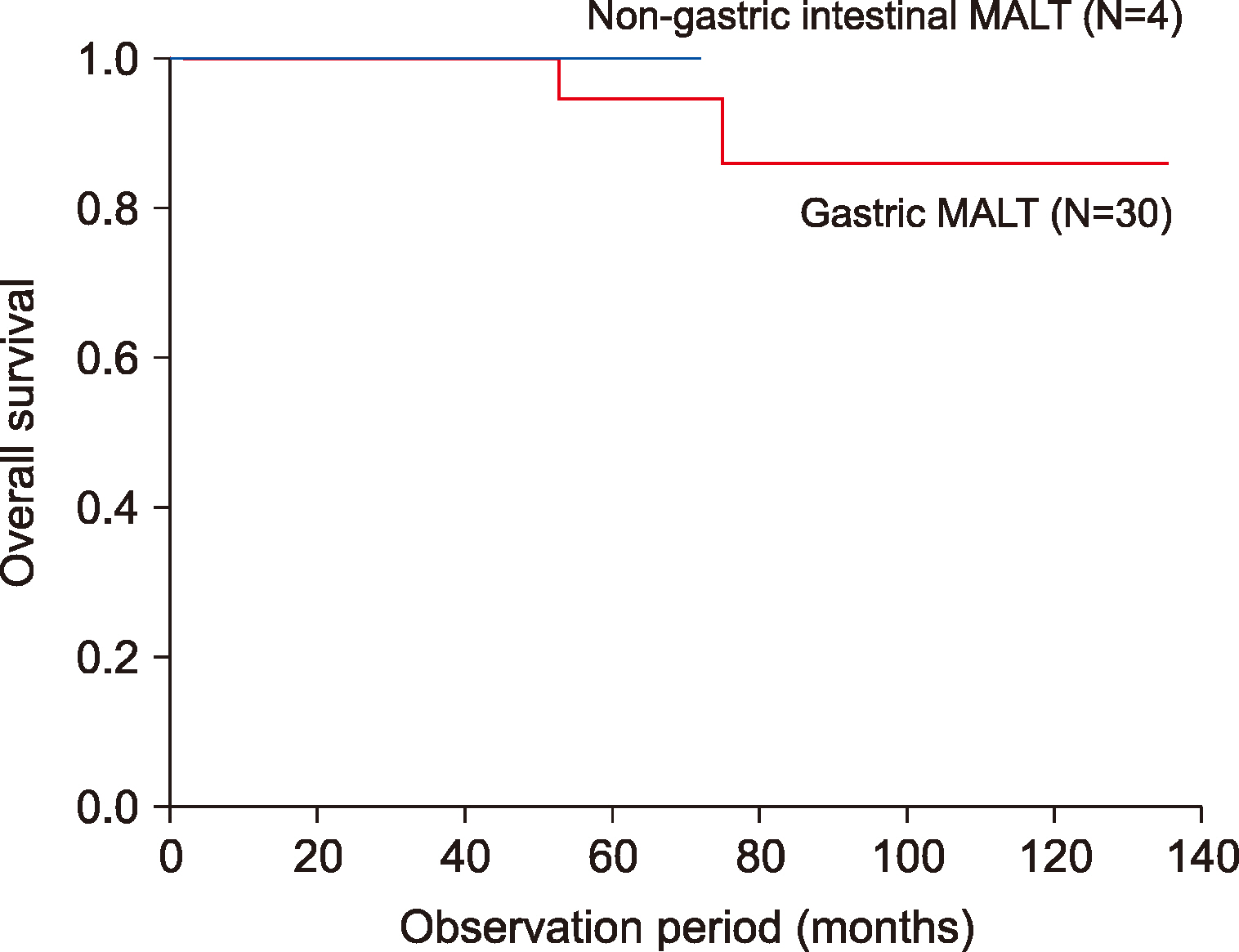
Fig. 2
The Kaplan–Meier curves for overall survival of the 4 non-gastric intestinal and 30 gastric MALT lymphoma patients.
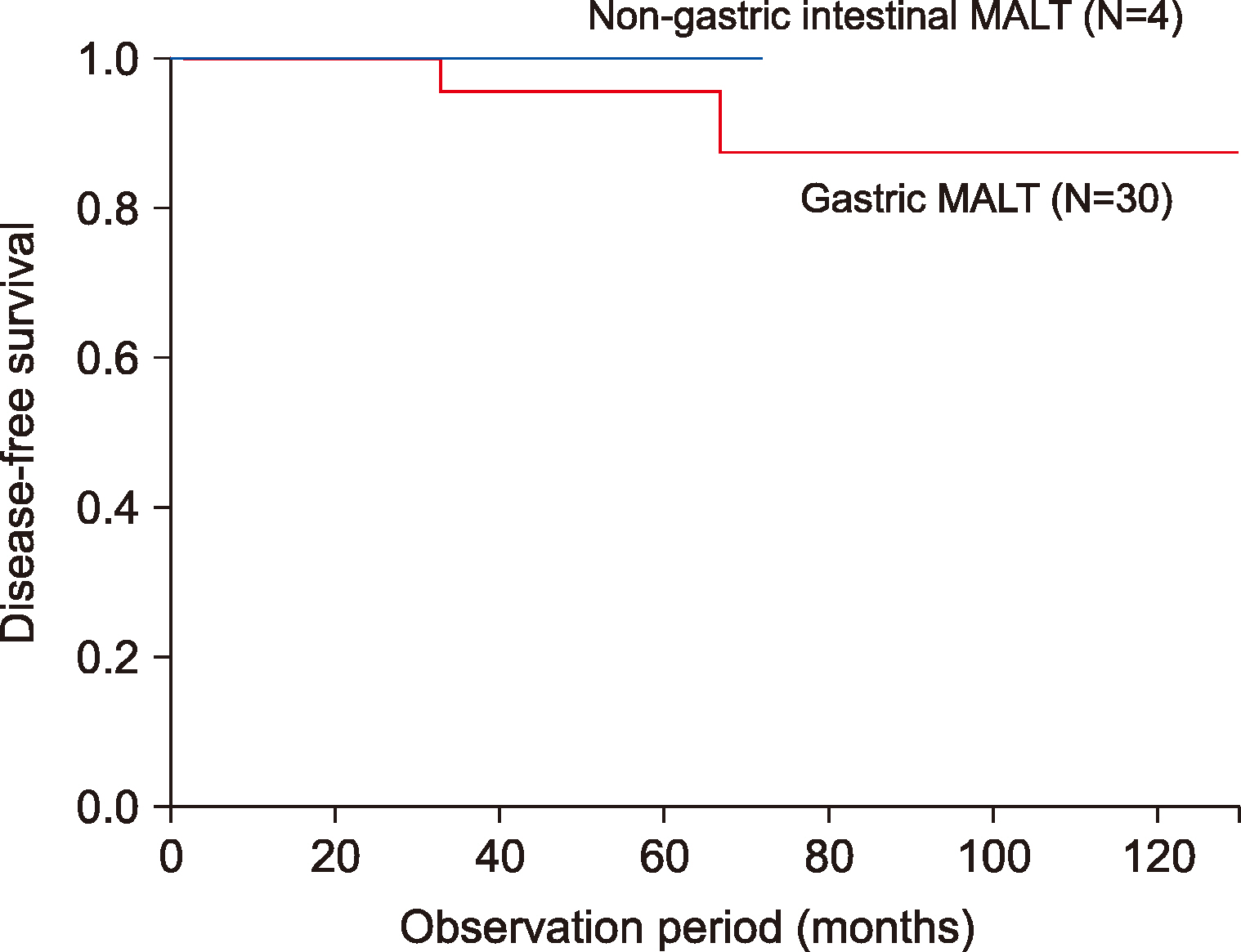
Table 1
Patient characteristics.
Table 2
Details of cases with recurrence.




 PDF
PDF Citation
Citation Print
Print


 XML Download
XML Download