2. Barberis I, Myles P, Ault SK, Bragazzi NL, Martini M. History and evolution of influenza control through vaccination: from the first monovalent vaccine to universal vaccines. J Prev Med Hyg. 2016; 57(3):E115–20. PMID:
27980374.
5. Doyle JD, Chung JR, Kim SS, Gaglani M, Raiyani C, Zimmerman RK, et al. Interim estimates of 2018–19 seasonal influenza vaccine effectiveness—United States, February 2019. MMWR Morb Mortal Wkly Rep. 2019; 68(6):135–139. PMID:
30763298.
6. Kissling E, Rose A, Emborg HD, Gherasim A, Pebody R, Pozo F, et al. Interim 2018/19 influenza vaccine effectiveness: six European studies, October 2018 to January 2019. Euro Surveill. 2019; 24(8):1900121.

7. Korea Centers for Disease Control and Prevention. 2018–2019 Influenza Management Guideline. Cheongju: Korea Centers for Disease Control and Prevention;2018.
8. Yun JW, Noh JY, Song JY, Chun C, Kim Y, Cheong HJ. The Korean influenza national immunization program: history and present status. Infect Chemother. 2017; 49(4):247–254. PMID:
29299891.



9. Jackson ML, Nelson JC. The test-negative design for estimating influenza vaccine effectiveness. Vaccine. 2013; 31(17):2165–2168. PMID:
23499601.


10. Grohskopf LA, Sokolow LZ, Broder KR, Walter EB, Fry AM, Jernigan DB. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2018–19 influenza season. MMWR Recomm Rep. 2018; 67(3):1–20.

11. World Health Organization. Recommended composition of influenza virus vaccines for use in the 2018–2019 northern hemisphere influenza season. Wkly Epidemiol Rec. 2018; 93(12):133–141. PMID:
29569429.

12. World Health Organization. Recommended composition of influenza virus vaccines for use in the 2019–2020 northern hemisphere influenza season. Wkly Epidemiol Rec. 2019; 94:141–150.
13. Orenstein WA, Bernier RH, Dondero TJ, Hinman AR, Marks JS, Bart KJ, et al. Field evaluation of vaccine efficacy. Bull World Health Organ. 1985; 63(6):1055–1068. PMID:
3879673.


15. Jung JE, Lee HR, Choi YH, Kim G. Immunization Program against Influenza in Korea; The 2018–2019 Influenza Season. Cheongju: Korea Centers for Disease Control and Prevention;2019. p. 2241–2249.
19. Japan Pediatric Society. Changes in the immunization schedule recommended by the Japan Pediatric Society. Updated 2020. Accessed October 27, 2020.
https://www.jpeds.or.jp.
20. Park SY, Kim JH, Cho EH, Kim WJ. Establishment of surveillance system and network for the evaluation of influenza vaccine effectiveness and estimation of influenza vaccine effectiveness in preventing influenza. Weekly Health and Disease: KCDC. 2020; 13(18):1207–1216.
21. Foppa IM, Haber M, Ferdinands JM, Shay DK. The case test-negative design for studies of the effectiveness of influenza vaccine. Vaccine. 2013; 31(30):3104–3109. PMID:
23624093.

22. Flannery B, Kondor RJ, Chung JR, Gaglani M, Reis M, Zimmerman RK, et al. Spread of antigenically drifted influenza A(H3N2) viruses and vaccine effectiveness in the United States during the 2018–2019 season. J Infect Dis. 2020; 221(1):8–15. PMID:
31665373.


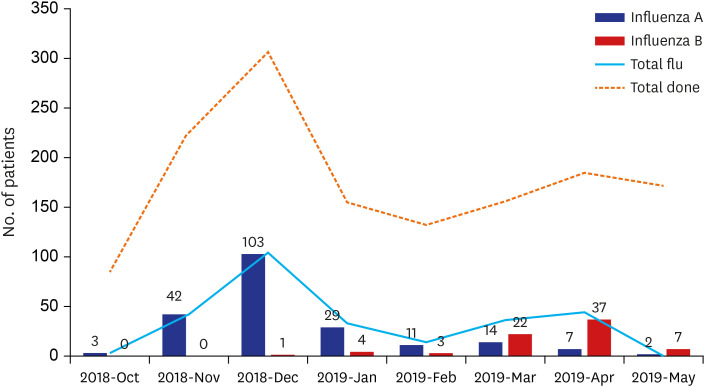
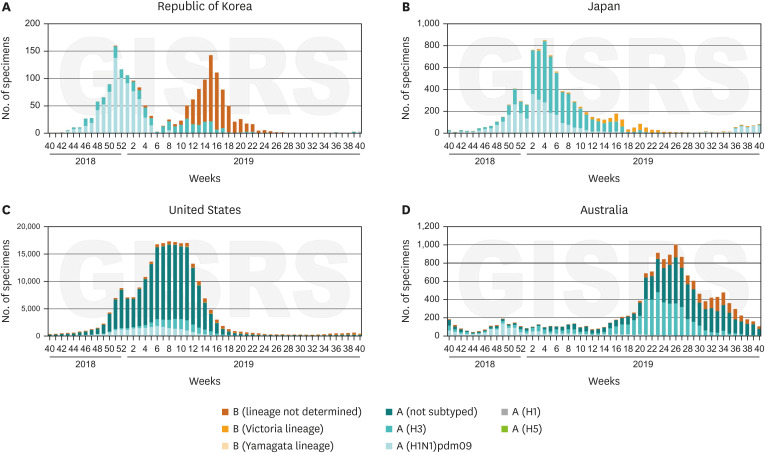
23. Park KS, Park SJ, Kwon DH, Lee DH. Influenza Sentinel Surveillance Report in the Republic of Korea, 2018–2019. Public Health Wkly Rep. 2019; 12(49):2224–2232.
24. Hammond A, Hundal K, Laurenson-Schafer H, Cozza V, Maharjan B, Fitzner J, et al. Review of the 2018–2019 influenza season in the northern hemisphere. Wkly Epidemiol Rec. 2019; 94(32):345–365.
25. Kim HM, Lee NJ, Kim MS, Park JH, Han MG. Korea influenza laboratory surveillance report in 2018–2019 season. Public Health Wkly Rep. 2019; 12(49):2238–2240.
26. Bosaeed M, Kumar D. Seasonal influenza vaccine in immunocompromised persons. Hum Vaccin Immunother. 2018; 14(6):1311–1322. PMID:
29485353.



27. Castrucci MR. Factors affecting immune responses to the influenza vaccine. Hum Vaccin Immunother. 2018; 14(3):637–646. PMID:
28617077.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download