This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Studies have reported on the usefulness of whole spine magnetic resonance imaging (MRI) in evaluating specific diseases such as spinal tuberculosis, spinal trauma, spondyloarthropathies, and multiple myeloma. In studies concerning degenerative spinal disease, sample sizes were small and some did not provide information on how symptomatic coexisting lesions were treated. We evaluated the types and prevalence of coexisting spine lesions found on whole spine T2 sagittal screening performed at the time of routine cervical and lumbar spine MRI and evaluated the efficacy of such screening in degenerative diseases of the cervical and lumbar spine.
Methods
We reviewed 1,757 and 2,266 consecutive cases where whole spine T2 sagittal screening had been performed with routine cervical and lumbar spine MRI, respectively, in patients with cervical and lumbar spinal degenerative diseases. Coexisting spine lesions were documented and statistical analysis was performed to investigate significant differences according to sex, age, and initial diagnosis. Electronic medical records were reviewed to determine whether additional interventions were necessary following such findings.
Results
We reviewed 1,252 and 1,689 consecutive cases of routine cervical and lumbar spine MRI respectively, with whole spine T2 sagittal screening. Of the 1,252, 419 (33.5%) patients with cervical spinal degenerative disease had coexisting lesions in the thoracolumbar spine. Patients with ligament ossification disease of the cervical spine showed a higher prevalence of coexisting spine lesions. Sixty of the 419 (14.3%) patients with coexisting spine lesions warranted additional intervention or surgical treatment. Four hundred and eighty-one of 1,689 (28.5%) patients with lumbar degenerative disease had coexisting spine lesions in the cervicothoracic spine. Forty-eight of the 481 (10.0%) patients with coexisting spine lesions warranted additional intervention. In both patient groups, older patients showed a significantly higher prevalence of coexisting spine lesions than younger patients.
Conclusion
Considering the minimal extra time and cost in performing whole spine screening, its application to routine spine MRI can be considered in evaluating cervical and lumbar spinal degenerative diseases.
Keywords: Coexisting Spine Lesion, Whole Spine MRI, Spinal Degenerative Disease
INTRODUCTION
Magnetic resonance imaging (MRI) is a useful, if not essential, imaging modality in evaluating spinal diseases. It provides valuable information concerning the spinal cord, nerve roots, intervertebral discs and ligamentous structures within the spine, with a high degree of sensitivity and specificity.
1234
Conventional spine MRI is performed focusing on a specific region-cervical, thoracic, or lumbar-depending on the patient's symptoms. Recent advances in MRI have made it possible to perform screening of the whole spine in addition to conventional region-specific imaging, with minimal increase in time and cost.
5 Studies have reported on the usefulness of whole spine MRI in evaluating specific diseases such as spinal tuberculosis, spinal trauma, spondyloarthropathies, and multiple myeloma.
6789 In studies concerning the usefulness of whole spine sagittal MRI screening in evaluating patients with degenerative spinal disease, sample sizes were small and some did not provide information on how symptomatic coexisting lesions were treated. At our institution, we have been performing routine whole spine T2 sagittal MRI screening, in addition to region specific imaging, since 2009. Some studies have reported that “tandem spinal stenosis,” stenosis in at least 2 distinct regions of the spine, can be seen in up to 60% of patients with spinal stenosis.
10 In such patients, addressing only one region of the spine may not provide sufficient symptom relief.
In this study, we evaluated the types and prevalence of coexisting spine lesions found on whole spine T2 sagittal screening performed at the time of routine cervical and lumbar spine MRI and evaluated the efficacy of such screening in degenerative diseases of the spine. More specifically, we sought to identify cases where surgical intervention was needed for coexisting lesions which would have not been addressed on conventional cervical or lumbar spine MRI.
METHODS
From January 2009 to August 2015, we reviewed 1,757 and 2,266 consecutive cases of routine cervical and lumbar spine MRI respectively, where whole spine T2 sagittal screening had been performed in patients with degenerative spinal diseases. Patients with a known history of previous spine surgery, spinal trauma, spinal infection and spinal tumors (both primary and secondary) were excluded.
Primary diagnoses were categorized into disc herniation/degeneration or spondylosis, degenerative spinal stenosis, and ligament ossification disease. Coexisting spine lesions were documented and statistical analysis was performed to investigate significant differences according to sex, age, and initial diagnosis. Electronic medical records were reviewed to determine whether additional interventions were necessary following such findings.
MRI was performed with both 1.5 and 3.0 Tesla scanners using a dual coil (neurovascular and spine coils combined) for whole spine imaging (Philips Achieva; Amsterdam, Netherlands).
Statistical analysis was performed using SPSS software (SPSS version 18.0; SPSS, Inc., Chicago, IL, USA). The χ2 test was used to compare categorical variables. P values lesser than 0.05 were considered statistically significant.
We reviewed cases where additional intervention was needed for concomitant cervical, thoracic or lumbar lesions and reviewed the outcome of such patients.
Ethics statement
Institutional Review Board (IRB) of Seoul National University College of Medicine approval was obtained before initiating this study (IRB 20-2017-4, IRB 20-2017-5). Informed consent was waived by the IRB for study.
RESULTS
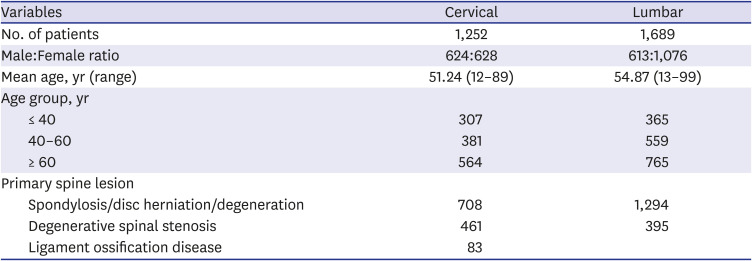
We reviewed 1,252 and 1,689 consecutive cases of routine cervical and lumbar spine MRI respectively, where whole spine T2 sagittal screening had been performed in patients with degenerative spinal diseases (
Table 1).
Table 1
Demographics
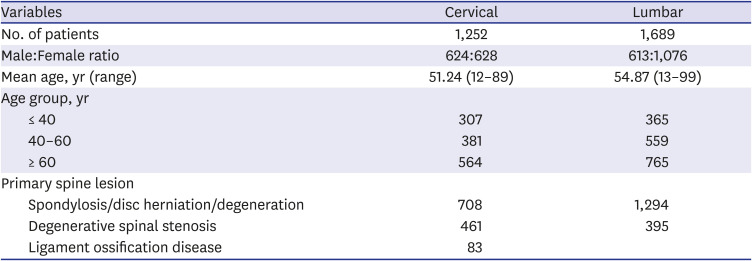
|
Variables |
Cervical |
Lumbar |
|
No. of patients |
1,252 |
1,689 |
|
Male:Female ratio |
624:628 |
613:1,076 |
|
Mean age, yr (range) |
51.24 (12–89) |
54.87 (13–99) |
|
Age group, yr |
|
|
|
≤ 40 |
307 |
365 |
|
40–60 |
381 |
559 |
|
≥ 60 |
564 |
765 |
|
Primary spine lesion |
|
|
|
Spondylosis/disc herniation/degeneration |
708 |
1,294 |
|
Degenerative spinal stenosis |
461 |
395 |
|
Ligament ossification disease |
83 |
|
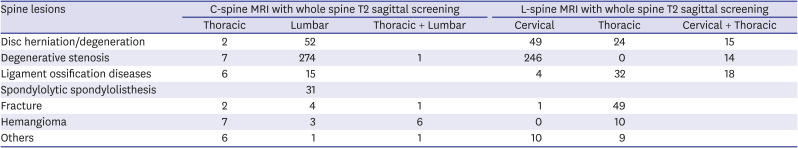
In cervical spine MRI with whole spine T2 sagittal screening cases, 419 patients had coexisting spine lesions with 214 males, 205 females and a mean age of 58.7 years. The lumbar spine was the most common site of coexisting spine lesions followed by coexisting thoracic spine lesions while 9 patients had coexisting lesions in both thoracic and lumbar spines. Common coexisting spine lesions in the lumbar spine were degenerative spinal stenosis, disc herniation/degeneration, and spondylolytic spondylolisthesis. Common coexisting spine lesions in the thoracic spine were degenerative stenosis, ligament ossification disease, and hemangioma (
Table 2). There was no difference in the prevalence of coexisting spine lesions between male and female patients (
P = 0.536).
Table 2
Types of coexisting spine lesions
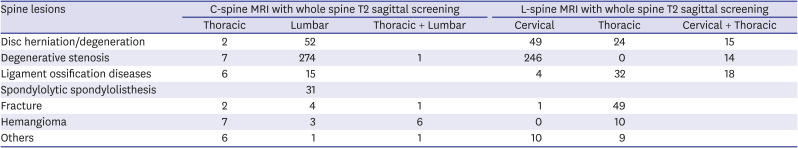
|
Spine lesions |
C-spine MRI with whole spine T2 sagittal screening |
L-spine MRI with whole spine T2 sagittal screening |
|
Thoracic |
Lumbar |
Thoracic + Lumbar |
Cervical |
Thoracic |
Cervical + Thoracic |
|
Disc herniation/degeneration |
2 |
52 |
|
49 |
24 |
15 |
|
Degenerative stenosis |
7 |
274 |
1 |
246 |
0 |
14 |
|
Ligament ossification diseases |
6 |
15 |
|
4 |
32 |
18 |
|
Spondylolytic spondylolisthesis |
|
31 |
|
|
|
|
|
Fracture |
2 |
4 |
1 |
1 |
49 |
|
|
Hemangioma |
7 |
3 |
6 |
0 |
10 |
|
|
Others |
6 |
1 |
1 |
10 |
9 |
|
In lumbar spine MRI with whole spine sagittal screening cases, 481 patients had coexisting spine lesions with 178 males, 303 females and a mean age of 60.0 years. The cervical spine was the most common site of coexisting spine lesions followed by coexisting thoracic spine lesions while 47 patients had coexisting lesions in both cervical and thoracic spines. Common coexisting spine lesions in the cervical spine were degenerative spinal stenosis (including cervical myelopathy), disc herniation/degeneration, and ligament ossification disease. Common coexisting spine lesions in the thoracic spine were ligament ossification disease, occult (acute or subacute) fractures, disc herniation/degeneration, and hemangioma (
Table 2). There was no difference in the prevalence of coexisting spine lesions between male and female patients (
P = 0.833).
In patients with primary lesions in the cervical spine, older patients showed a significantly higher prevalence of coexisting spine lesions than younger patients (
P < 0.001); 8.8% in patients ≤ 40 years of age, 34.4% in patients 40 to 60 years of age, and 52% in patients ≥ 60 years of age. The primary diagnosis was significantly correlated with prevalence of coexisting spine lesions (
P < 0.001). In patients diagnosed with cervical ligament ossification disease, 48.2% had coexisting lesions in the thoracic or lumbar spine (
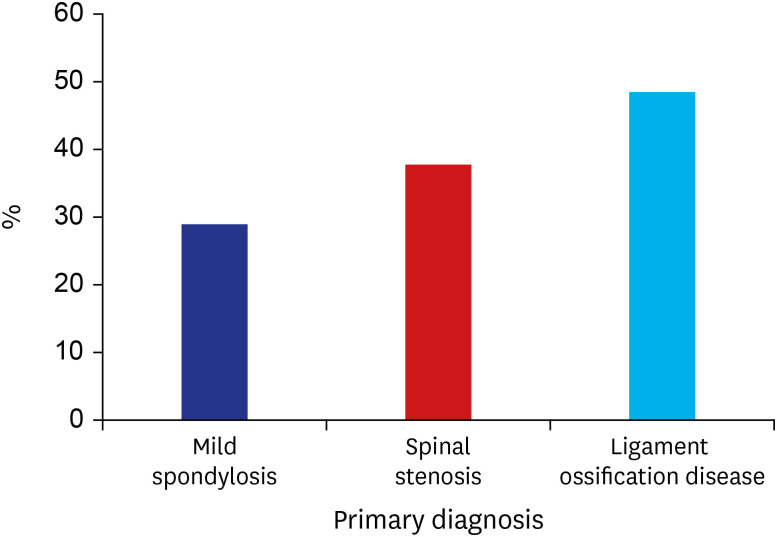
Fig. 1).
Fig. 1
Coexisting thoracolumbar lesions and primary diagnosis of the cervical spine.
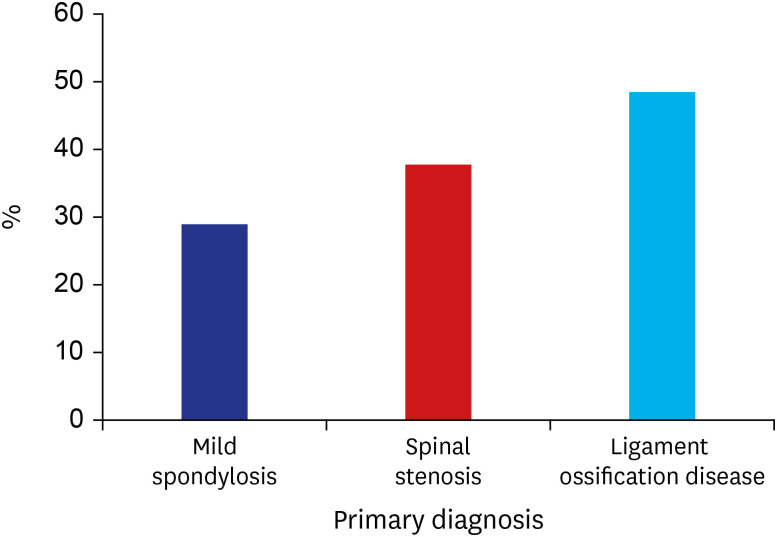
In patients with primary lesions in the lumbar spine, older patients showed a significantly higher prevalence of coexisting spine lesions than younger patients P < 0.001); 15.6% in patients ≤ 40 years of age, 25.8% in patients 40 to 60 years of age, and 36.1% in patients ≥ 60 years of age. The primary diagnosis was not significantly correlated with prevalence of coexisting spine lesions (P = 0.650).
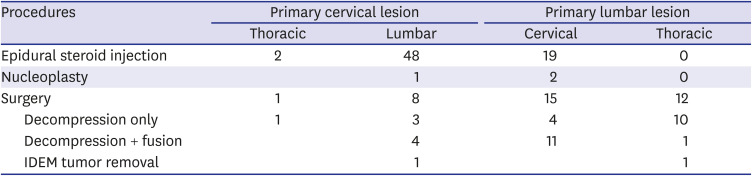
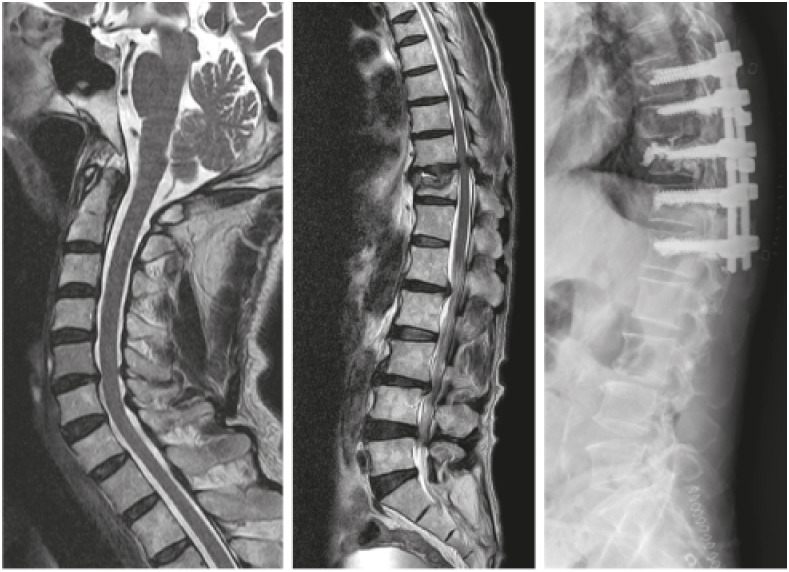
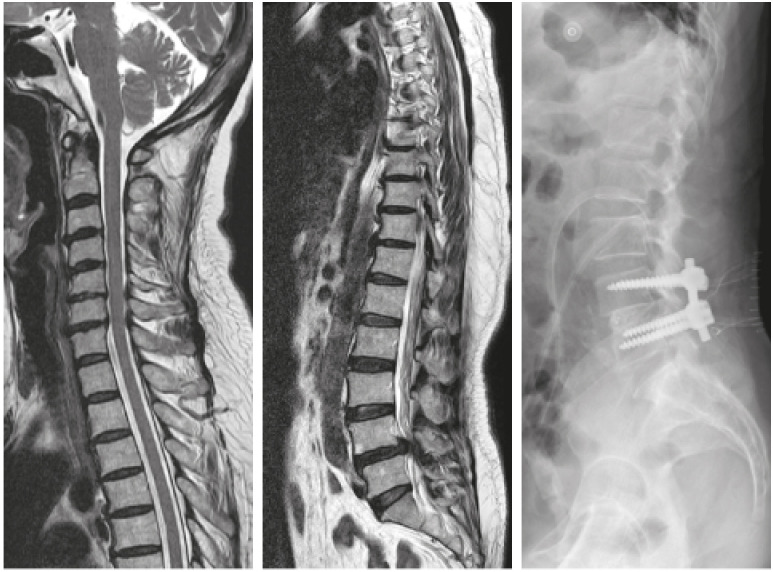
Sixty of 419 cervical spine patients with coexisting spine lesions needed additional intervention. For thoracic lesions, we performed epidural steroid injection in 2 cases and 1 case of surgery. For lumbar lesions, we performed 48 epidural steroid injections, 1 nucleoplasty, and 8 surgeries (
Table 3). The figures below show a patient with an unremarkable thoracolumbar MRI screening, and patients who received surgical treatment for coexisting lesions found in the thoracic or lumbar spine (
Figs. 2,
3,
4).
Table 3
Additional procedures due to coexisting lesions
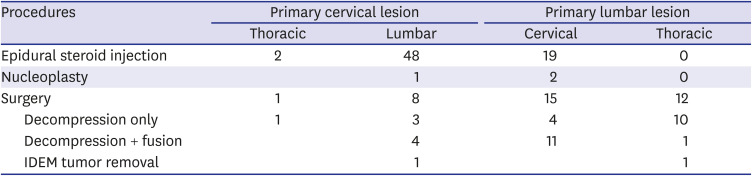
|
Procedures |
Primary cervical lesion |
Primary lumbar lesion |
|
Thoracic |
Lumbar |
Cervical |
Thoracic |
|
Epidural steroid injection |
2 |
48 |
19 |
0 |
|
Nucleoplasty |
|
1 |
2 |
0 |
|
Surgery |
1 |
8 |
15 |
12 |
|
Decompression only |
1 |
3 |
4 |
10 |
|
Decompression + fusion |
|
4 |
11 |
1 |
|
IDEM tumor removal |
|
1 |
|
1 |
Fig. 2
Thoracolumbar sagittal screening with unremarkable findings.

Fig. 3
A 71-year-old male presented with an unstable gait and posterior neck pain. Cervical spine MRI revealed moderate stenosis without definite cervical myelopathy, while thoracolumbar magnetic resonance imaging screening showed thoracic myelopathy at T10-11 with Kummell's disease at T11. Decompression and instrumented fusion was performed.
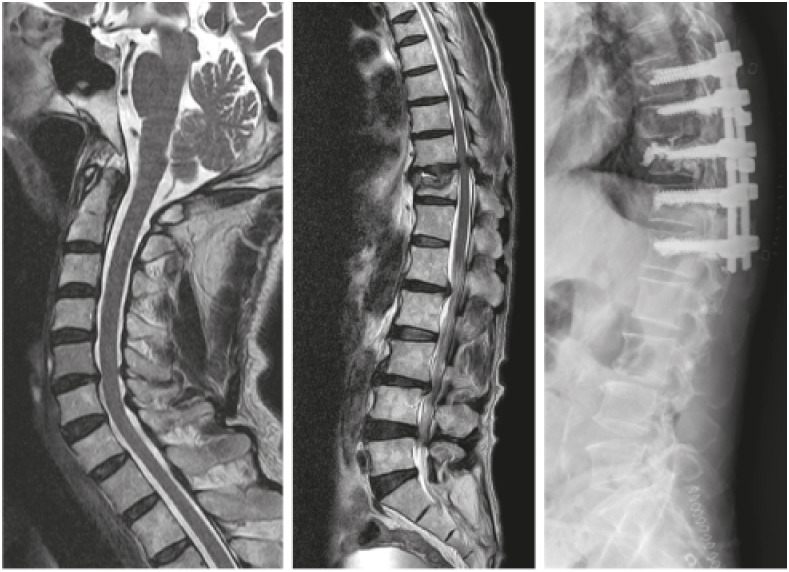
Fig. 4
A 51-year-old female presented with posterior neck pain and low back pain with radiating pain to both lower extremities. Cervical spine MRI showed moderate stenosis but thoracolumbar MRI screening showed severe lumbar spinal stenosis. Posterior lumbar interbody fusion was performed.
MRI = magnetic resonance imaging.
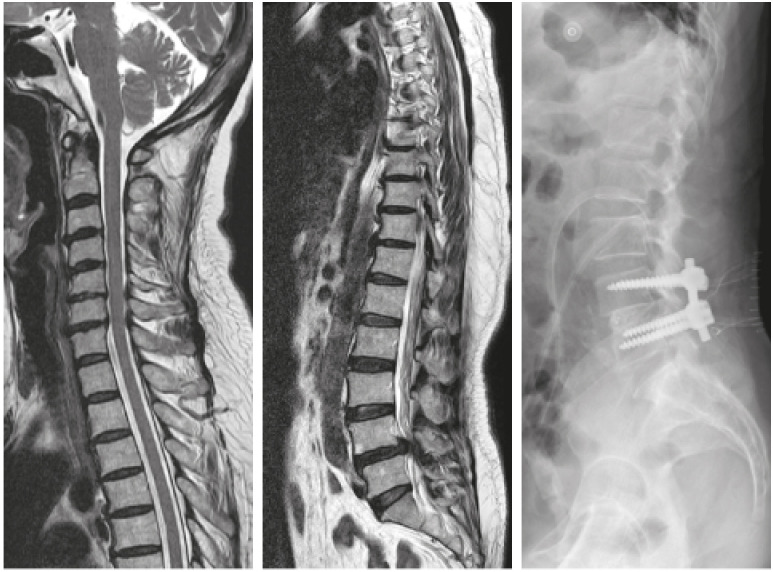
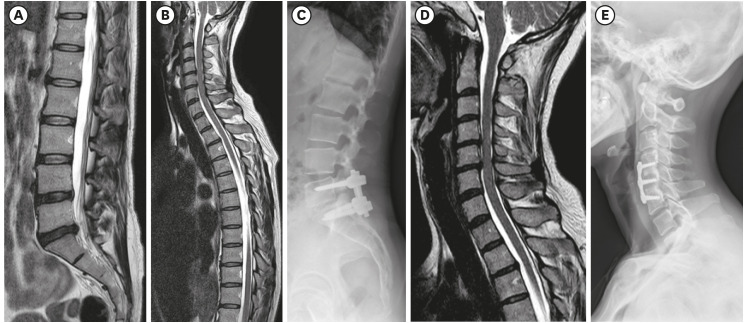
Forty-eight of 481 lumbar spine patients with coexisting spine lesions warranted additional intervention such as epidural steroid injection, vertebroplasty/kyphoplasty, and decompression with or without fusion (
Table 3). Cervical myelopathy (11 of 15 cases) was the most common cause for cervical spine surgery and occult fracture (10 of 12 cases) was the most common cause for thoracic spine surgery. The following figures depict a patient without any concomitant cervical or thoracic lesion, and patients who underwent surgery or cervical and thoracic lesions, respectively (
Figs. 5,
6,
7).
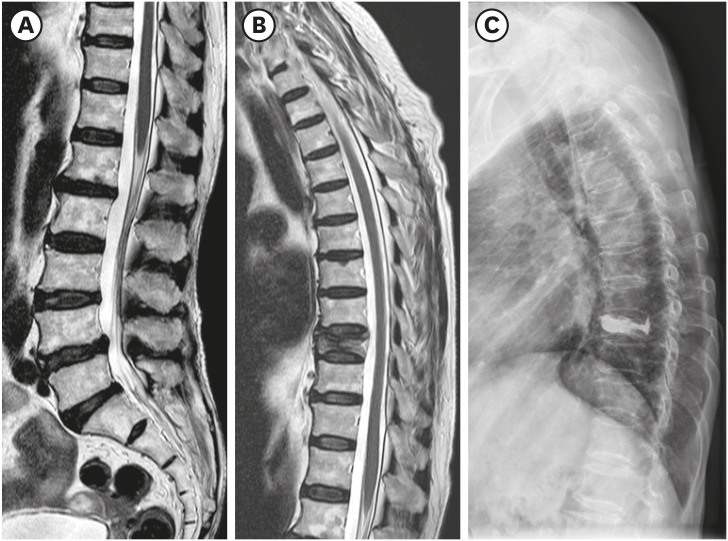
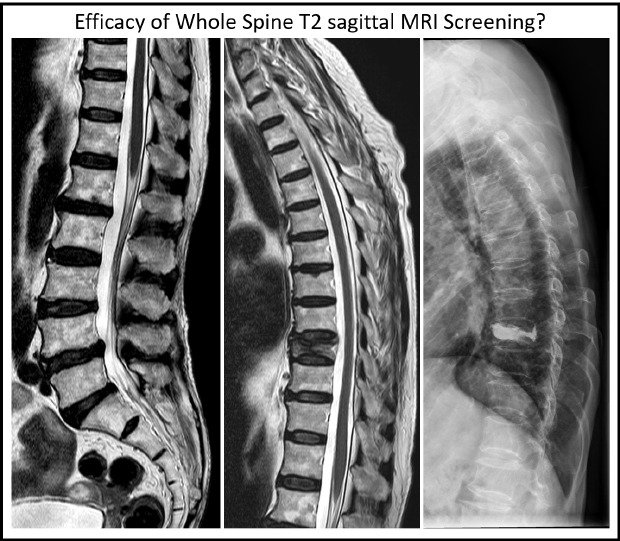
Fig. 5
Cervicothoracic sagittal magnetic resonance imaging screening with unremarkable findings.

Fig. 6
This 41-year-old female has a complicated treatment history. She initially presented with low back and radiating pain to both lower extremities. (A) L5-S1 disc protrusion was observed in the lumbar spine, (B) while screening of her cervicothoracic spine showed moderate cord compression in her cervical spine albeit asymptomatic. (C) Despite conservative treatment of the lumbar spine for over 2 years, the patient's low back pain became intractable and she opted for a L5-S1 posterior lumbar interbody fusion. (D) 2 years after lumbar surgery, she developed radiating pain to both upper extremities with radiographic evidence of early stage compressive myelopathy. (E) A 2 level anterior cervical discectomy and fusion was performed.
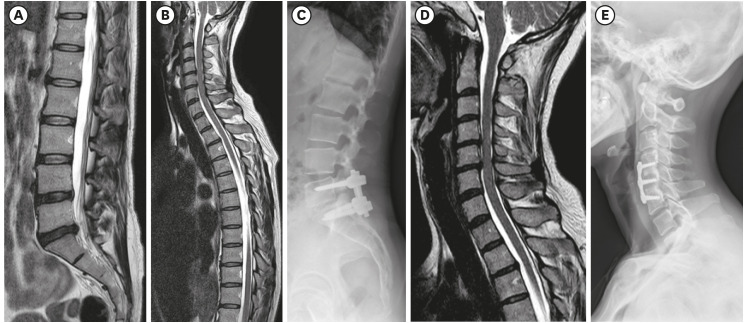
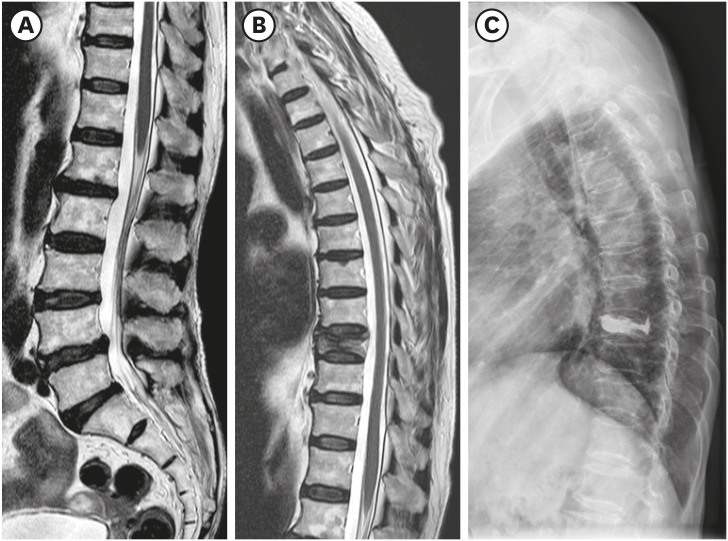
Fig. 7
A 45-year-old female presented with low back pain. (A) L-spine MRI showed only mild disc bulging, (B) while whole spine sagittal MRI screening showed an occult fracture in the thoracic spine. (C) The patient's symptoms improved after undergoing vertebroplasty.
MRI = magnetic resonance imaging.
DISCUSSION
Whole spine MRI has been adopted as a useful and necessary diagnostic tool in certain spinal diseases likely to affect the whole spine.
6789 While there have been reports of asymptomatic and symptomatic “tandem spinal stenosis” in up to 60% of patient with spinal stenosis,
10 there are few studies concerning the use of whole spine sagittal MRI screening in spinal degenerative diseases.
The routine use of whole spine sagittal MRI screening in spinal degenerative diseases and may be controversial due to additional time and cost required. However, recent advances in MRI have allowed such screening with minimal additional time and cost. At our institution, whole spine sagittal MRI screening requires approximately an additional 5 minutes and 50,000 Korean won (approximately 44 US dollars). Other studies have reported that whole spine sagittal screening required an additional 1.5–5 minutes scanning time without mention of additional cost.
1112 While the efficacy of routine whole spine sagittal MRI screening is debatable and warrants further study, additional time and cost currently required seems to make its routine use a feasible option.
In our study, coexisting spine lesions were identified in 419 of 1,252 patients (33.5%) and 481 of 1,689 patients (28.5%), through cervical and lumbar spine MRI with whole spine T2 sagittal screening, respectively. Sixty of 419 patients (14.3%) and 48 of 481 patients (10.0%) required additional intervention. While most coexisting lesions were asymptomatic, this does not construe these findings as unmeaningful. There is the possibility of delayed aggravation, as reported by Bednarik et al.
13 where myelopathy developed in 19.7% of patients with asymptomatic spondylotic cervical cord compression in MRI, at 2 or more years of follow up. Numerous studies have reported on concurrent stenosis of the cervical and lumbar spine.
141516 Although in some cases, additional diagnostic studies may contribute to rising healthcare costs due to unnecessary surgery based on incidental findings, we believe that whole spine sagittal MRI screening is a useful tool for clinicians. It allows clinicians to better match patients' symptoms with MRI findings and take coexisting spine lesions into consideration in planning operative procedures.
Whole spine sagittal MRI screening may be especially meaningful for older patients as our study showed a statistically significant increase in coexisting spine lesions with age. Due to the nature of degenerative spine diseases, such results may be expected, but early detection of such lesions allow the physician to educate patients regarding their current status and suggest changes in lifestyle to mitigate the possibility of further aggravation.
17 Han et al.,
12 who conducted a similar study albeit with a smaller number of patients (306 cases), also concluded that old age (≥ 40 years of age) showed a significantly higher prevalence of coexisting spine lesions. Knowledge of coexisting spine lesions also makes it possible for prompt follow-up upon aggravation.
Our study showed that primary diagnosis in the cervical spine was significantly associated with the prevalence of coexisting spine lesions. Nearly half (48.2%) of patients diagnosed with cervical ligament ossification disease had coexisting lesions in the thoracolumbar spine. Although studies regarding this subject are scarce, Yamada et al.
18 reported that that patients with cervical ossified posterior longitudinal ligament disease were more likely to have tandem spinal stenosis. Han et al.
12 stated that in patients with ligament ossification diseases, either in the cervical or lumbar spine, coexisting spine lesions were found in 52.4% of patients. In patients with cervical ligament ossification disease, surgeons should consider the possibility of coexisting lesions in the thoracolumbar spine.
We believe that this study is significant in that it is one of the few studies focusing on utilizing whole spine T2 sagittal screening in degenerative spinal diseases. Our patient pool of 1,252 and 1,689 consecutive cases of cervical and lumbar spine degenerative disease cases, respectively, is the largest to date in the published literature.
This study is limited in its retrospective nature, and further prospective study with sufficient follow up is warranted for conclusive results.
In conclusion, coexisting spine lesions were identified in 33.5% and 28.5% of cervical and lumbar degenerative spinal disease patients, respectively, with routine whole spine T2 sagittal screening. Sixty of 419 and 48 of 481 patients required additional intervention. Considering the minimal extra time and social costs in performing whole spine screening, its application to routine spine MRI can be considered in evaluating cervical spinal degenerative diseases.




 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download