This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The risk of tick-borne diseases is decreased by increasing awareness and knowledge through prevention education. The aim of the present study was to evaluate the effect of long-lasting permethrin impregnated (LLPI) socks for tick bites.
Methods
A randomized open label study was conducted to determine the effectiveness of LLPI socks for prevention of tick bites among 367 adults living in a rural area. Participants completed questionnaires at the start of follow-up (July 2014) and at the end of follow-up (December 2014), and tick bites were reported.
Results
A total of 332 subjects completed the follow-up survey. The tick bite rate of the two groups was not significantly different (3.6% vs. 3.1%). But the tick bite rate of lower extremities of subjects wearing LLPI socks was significantly lower compared to that of subjects wearing general socks.
Conclusion
The tick bite rate was not different between the two groups, but the tick bite rate of lower extremities of LLPI was significantly lower than general groups. Further study is needed to investigate the effect of LLPI clothes with larger populations.
Keywords: Insect Repellents, Permethrin, Randomized Controlled Trial, Ticks
INTRODUCTION
The most common vector-borne diseases in Korea are those carried by ticks or mites. The incidence of mite or tick-borne diseases such as scrub typhus, severe fever with thrombocytopenia syndrome and Lyme disease has been increasing.
1 These mite or tick-borne diseases can cause serious illness or death if not treated early and is a significant public health threat.
23
Arthropods-borne diseases are an occupational risk for outdoor workers, particularly among farmers or subjects living in rural areas.
45 Recommended prevention methods against biting ticks or mites for outdoor workers include wearing light-colored clothes, wearing protective clothe (long sleeves, high boots, and a hat), use of tick repellants, showering after work, washing and drying work clothes at high temperature, and examining the body for ticks after work.
67
The most commonly used form of tick repellant for clothing treatment is a self-applied permethrin spray. Under controlled conditions, spray of permethrin to clothing can provide highly effective protection against ticks.
89 However, the protective effect of this method does not persist over long periods of wear or multiple washings.
1011 Previous studies reported that adherence to traditional recommendations for preventing tick bites including self-applied repellents was less than optimal even among people knowledgeable about the risks of tick-borne disease.
12 Thus, more effective and user friendly tick bite prevention methods are needed.
The use of long-lasting permethrin impregnated (LLPI) clothing for high-risk outdoor workers could be a simple, safe, and cost-effective method to reduce tick bites and tick-borne disease. This study was conducted to determine the effectiveness of LLPI socks for the prevention of tick bites among adults living in rural areas in Korea.
METHODS
Study design
An open-label, randomized intervention study was conducted to determine whether wearing LLPI socks was associated with fewer tick bites among adults living in rural areas. Adults living in a rural area of Boseong, Jeollanam-do, Korea were selected as the study population for the study. The majority of these sites are farming areas.
Each subject was assigned to either the treatment or control group through block randomization using block sizes of four, which were generated randomly by computer, with 1:1 allocation for the treatment or control interventions. In addition, according to their treatment group, subjects were either given four pairs of treated or untreated socks at the start of the study. LLPI socks produced by Insect Shield, a company based in Greensboro, NC, USA were provided to the treatment group. General socks which were of similar length, thickness and color with treated socks were provided to the control group. All subjects were instructed to launder their socks as they normally would and to continue with their normal tick bite prevention measures, regardless of their treatment status.
Preventive education regarding scrub typhus was provided to both groups at enrollment using a 9-minute video and paper leaflets. The educational materials were developed by the Korea Center for Disease Control and Prevention in 2009 and consisted of the definition, causative agent, risky behavior, clinical features, early detection and treatment and preventive practices of scrub typhus.
Subject recruitment and data collection
Subjects living in the rural area more than 1 year were invited to participate in the study. Initially, informational meetings with the head of the village were conducted to describe the permethrin treatment, study design, and participation requirements at the township office on 10th July 2014. Then eligible subjects were invited to enroll at village hall. Finally, 367 subjects completed informed consent and were enrolled in the study.
After completion of informed consent, participants completed a baseline questionnaire. In addition to general demographic and occupational information, subjects were asked to report tick bite history in the past year and lifetime history of tick-borne disease. The follow-up periods started the week of July 14–17, 2014, or the week the subject started wearing their provided socks and continued over 3 months until December 18–19, 2014. At the end of the follow-up period, subjects completed a follow-up questionnaire. Questions included tick bites, and site of tick bite during the follow-up period and knowledge of preventive behavior for scrub typhus. In addition, the number of days socks were worn during the past weeks and the number of washes of socks were investigated.
Statistical analysis
Baseline characteristics of the treatment and control groups were compared using the χ2 tests. The proportion of tick bites and site of tick bite between treatment and control groups were compared using χ2 tests. Differences in preventive behavior and knowledge were assessed by t-tests. All analyses were performed using SAS (version 9.2; SAS Institute Inc., Cary, NC, USA). P value < 0.05 was considered statistically significant.
Ethics statement
The Institutional Review Board of Chosun University Hospital approved the study protocol (CHOSUN 2014-06-019-001). All subjects were adults and provided written informed consent.
RESULTS
Baseline characteristics of treatment and control groups
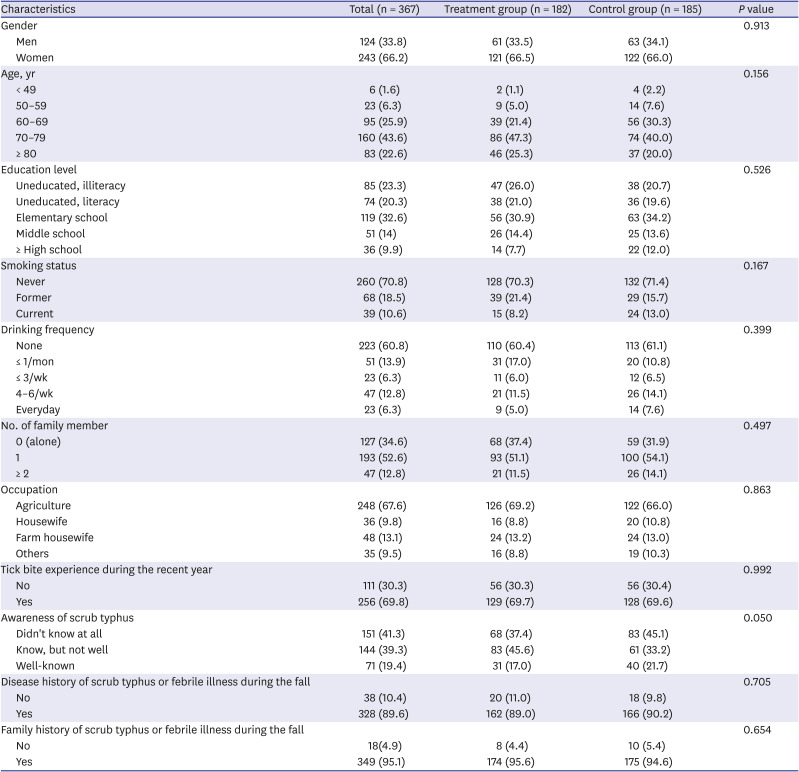
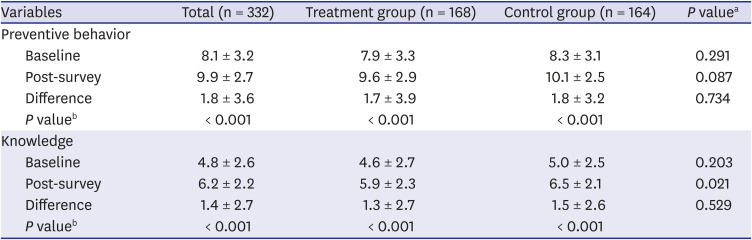
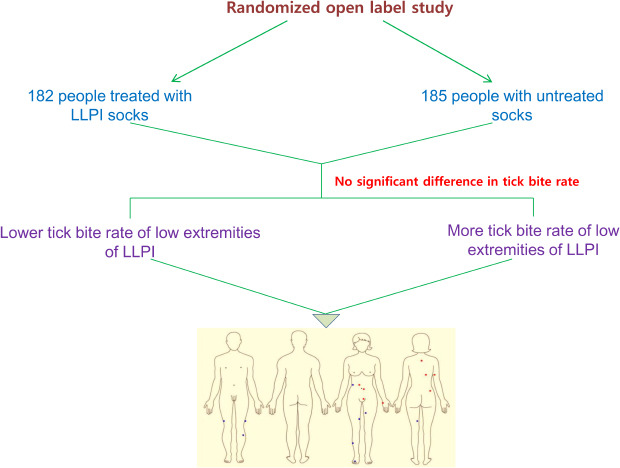
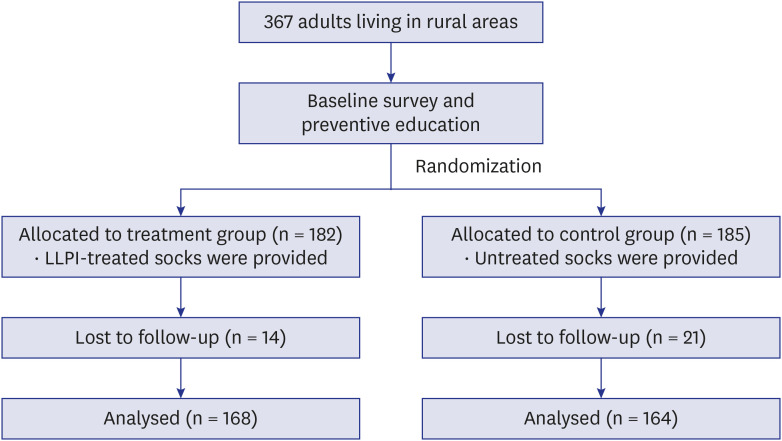
A total of 182 subjects in treatment group and 185 subjects in control group were enrolled (
Fig. 1). The proportions of women were 66.5% and 66.0% in treatment and control groups, respectively. About 70% of subjects had tick bite history during the past year. Additionally, the tick bite experience during the recent year, disease history of scrub typhus or febrile illness during the fall and other baseline characteristics were not different between treatment and control groups (
Table 1).
Fig. 1
Flow of study participants.
LLPI = long-lasting permethrin impregnated.
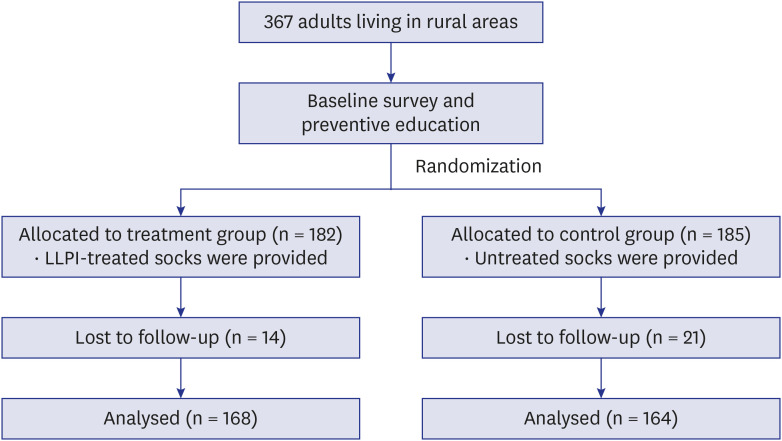
Table 1
Baseline characteristics of treatment and control groups
|
Characteristics |
Total (n = 367) |
Treatment group (n = 182) |
Control group (n = 185) |
P value |
|
Gender |
|
|
|
0.913 |
|
Men |
124 (33.8) |
61 (33.5) |
63 (34.1) |
|
Women |
243 (66.2) |
121 (66.5) |
122 (66.0) |
|
Age, yr |
|
|
|
0.156 |
|
< 49 |
6 (1.6) |
2 (1.1) |
4 (2.2) |
|
50–59 |
23 (6.3) |
9 (5.0) |
14 (7.6) |
|
60–69 |
95 (25.9) |
39 (21.4) |
56 (30.3) |
|
70–79 |
160 (43.6) |
86 (47.3) |
74 (40.0) |
|
≥ 80 |
83 (22.6) |
46 (25.3) |
37 (20.0) |
|
Education level |
|
|
|
0.526 |
|
Uneducated, illiteracy |
85 (23.3) |
47 (26.0) |
38 (20.7) |
|
Uneducated, literacy |
74 (20.3) |
38 (21.0) |
36 (19.6) |
|
Elementary school |
119 (32.6) |
56 (30.9) |
63 (34.2) |
|
Middle school |
51 (14) |
26 (14.4) |
25 (13.6) |
|
≥ High school |
36 (9.9) |
14 (7.7) |
22 (12.0) |
|
Smoking status |
|
|
|
0.167 |
|
Never |
260 (70.8) |
128 (70.3) |
132 (71.4) |
|
Former |
68 (18.5) |
39 (21.4) |
29 (15.7) |
|
Current |
39 (10.6) |
15 (8.2) |
24 (13.0) |
|
Drinking frequency |
|
|
|
0.399 |
|
None |
223 (60.8) |
110 (60.4) |
113 (61.1) |
|
≤ 1/mon |
51 (13.9) |
31 (17.0) |
20 (10.8) |
|
≤ 3/wk |
23 (6.3) |
11 (6.0) |
12 (6.5) |
|
4–6/wk |
47 (12.8) |
21 (11.5) |
26 (14.1) |
|
Everyday |
23 (6.3) |
9 (5.0) |
14 (7.6) |
|
No. of family member |
|
|
|
0.497 |
|
0 (alone) |
127 (34.6) |
68 (37.4) |
59 (31.9) |
|
1 |
193 (52.6) |
93 (51.1) |
100 (54.1) |
|
≥ 2 |
47 (12.8) |
21 (11.5) |
26 (14.1) |
|
Occupation |
|
|
|
0.863 |
|
Agriculture |
248 (67.6) |
126 (69.2) |
122 (66.0) |
|
Housewife |
36 (9.8) |
16 (8.8) |
20 (10.8) |
|
Farm housewife |
48 (13.1) |
24 (13.2) |
24 (13.0) |
|
Others |
35 (9.5) |
16 (8.8) |
19 (10.3) |
|
Tick bite experience during the recent year |
|
|
|
0.992 |
|
No |
111 (30.3) |
56 (30.3) |
56 (30.4) |
|
Yes |
256 (69.8) |
129 (69.7) |
128 (69.6) |
|
Awareness of scrub typhus |
|
|
|
0.050 |
|
Didn't know at all |
151 (41.3) |
68 (37.4) |
83 (45.1) |
|
Know, but not well |
144 (39.3) |
83 (45.6) |
61 (33.2) |
|
Well-known |
71 (19.4) |
31 (17.0) |
40 (21.7) |
|
Disease history of scrub typhus or febrile illness during the fall |
|
|
|
0.705 |
|
No |
38 (10.4) |
20 (11.0) |
18 (9.8) |
|
Yes |
328 (89.6) |
162 (89.0) |
166 (90.2) |
|
Family history of scrub typhus or febrile illness during the fall |
|
|
|
0.654 |
|
No |
18(4.9) |
8 (4.4) |
10 (5.4) |
|
Yes |
349 (95.1) |
174 (95.6) |
175 (94.6) |
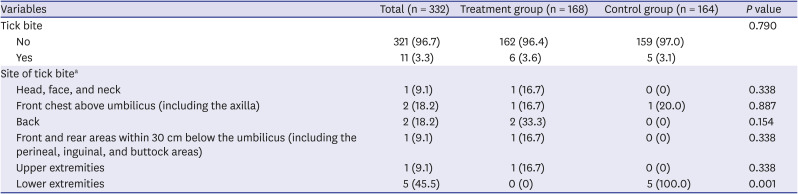
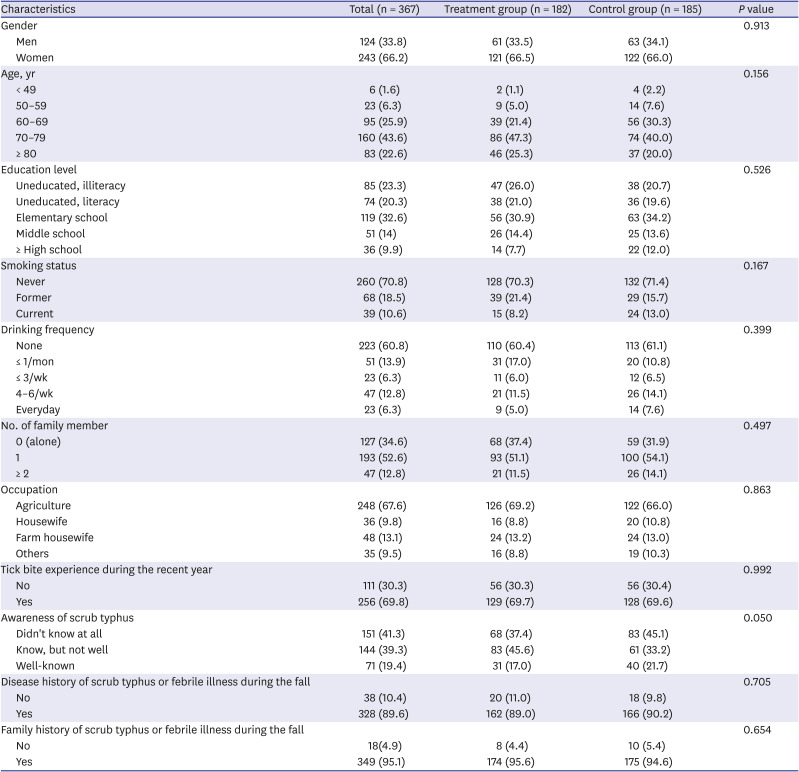
Tick bite at post-survey
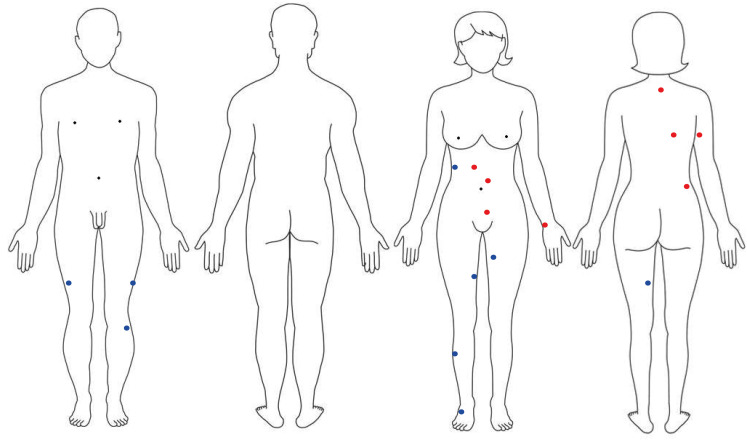
A total of 332 subjects completed a follow-up questionnaire. There were no significant differences in the number of days socks were worn during the past week (4.99 ± 2.05 vs. 5.08 ± 2.04,
P = 0.684) and the number of washes of socks per week (7.19 ± 9.22 vs. 6.97 ± 8.08,
P = 0.818). Among them, 3.3% of subjects reported the tick bite experience. The tick bite rates of the two groups were not significantly different (3.6% vs. 3.1%). But the tick bite rate of lower extremities of subjects wearing permethrin impregnated socks was significantly lower compared to subjects wearing general socks (
Table 2 and
Fig. 2).
Table 2
Tick bite experience at post-survey
|
Variables |
Total (n = 332) |
Treatment group (n = 168) |
Control group (n = 164) |
P value |
|
Tick bite |
|
|
|
0.790 |
|
No |
321 (96.7) |
162 (96.4) |
159 (97.0) |
|
Yes |
11 (3.3) |
6 (3.6) |
5 (3.1) |
|
Site of tick bitea
|
|
|
|
|
|
Head, face, and neck |
1 (9.1) |
1 (16.7) |
0 (0) |
0.338 |
|
Front chest above umbilicus (including the axilla) |
2 (18.2) |
1 (16.7) |
1 (20.0) |
0.887 |
|
Back |
2 (18.2) |
2 (33.3) |
0 (0) |
0.154 |
|
Front and rear areas within 30 cm below the umbilicus (including the perineal, inguinal, and buttock areas) |
1 (9.1) |
1 (16.7) |
0 (0) |
0.338 |
|
Upper extremities |
1 (9.1) |
1 (16.7) |
0 (0) |
0.338 |
|
Lower extremities |
5 (45.5) |
0 (0) |
5 (100.0) |
0.001 |
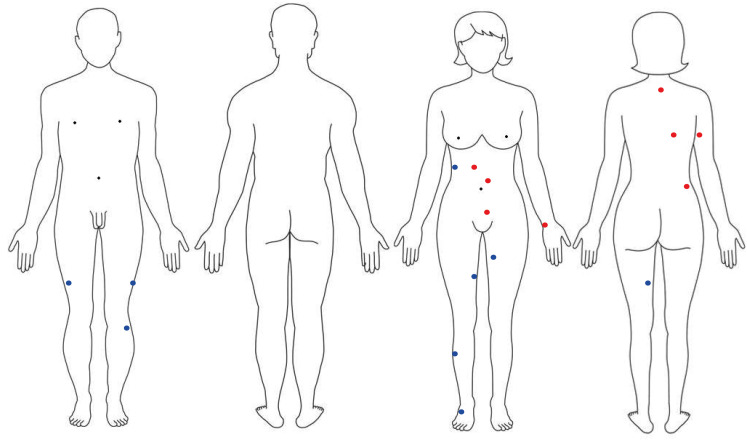
Fig. 2
Sites of tick bites at post-survey. Red colored dot: treatment group. Blue colored dot: control group.
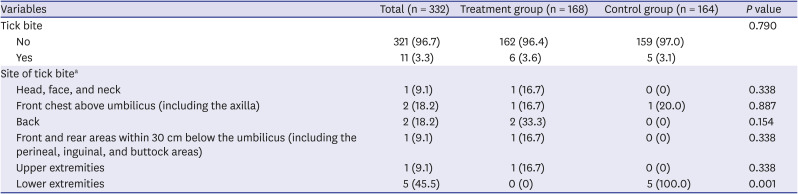
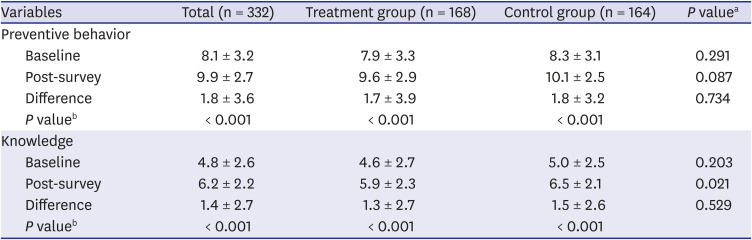
Preventive behavior and knowledge regarding scrub typhus
While the scores for preventive behavior and knowledge regarding scrub typhus were not different between the groups at baseline (
P < 0.05), they were significantly increased in both groups after the survey (
P < 0.001) (
Table 3).
Table 3
Preventive behavior and knowledge regarding scrub typhus
|
Variables |
Total (n = 332) |
Treatment group (n = 168) |
Control group (n = 164) |
P valuea
|
|
Preventive behavior |
|
|
|
|
|
Baseline |
8.1 ± 3.2 |
7.9 ± 3.3 |
8.3 ± 3.1 |
0.291 |
|
Post-survey |
9.9 ± 2.7 |
9.6 ± 2.9 |
10.1 ± 2.5 |
0.087 |
|
Difference |
1.8 ± 3.6 |
1.7 ± 3.9 |
1.8 ± 3.2 |
0.734 |
|
P valueb
|
< 0.001 |
< 0.001 |
< 0.001 |
|
|
Knowledge |
|
|
|
|
|
Baseline |
4.8 ± 2.6 |
4.6 ± 2.7 |
5.0 ± 2.5 |
0.203 |
|
Post-survey |
6.2 ± 2.2 |
5.9 ± 2.3 |
6.5 ± 2.1 |
0.021 |
|
Difference |
1.4 ± 2.7 |
1.3 ± 2.7 |
1.5 ± 2.6 |
0.529 |
|
P valueb
|
< 0.001 |
< 0.001 |
< 0.001 |
|
DISCUSSION
Prevention of tick bites is critical for control of tick-borne disease among outdoor workers and subjects in rural areas. This study investigated the effect of LLPI socks on tick bite. After 4–5 months of wearing socks, the tick bite rate between the two groups was not different. But the tick bite of lower extremities was significantly lower in LLPI socks group. Interestingly, tick bites in lower extremities only occurred in subjects who wore general socks. Preventive behavior and knowledge scores for scrub typhus were improved in both groups, and tick bite rates decreased significantly after the interventions of preventive behavior education and wearing LLPI or standard socks.
Permethrin is widely used as a repellent and insecticide for agricultural, residential, and personal use on clothing. Permethrin when used at appropriate concentrations has an excellent safety record.
13 A factory-based method for long-lasting permethrin impregnation of clothing has been developed by Insect Shield, Inc., that allows clothing to retain insecticidal activity for over 70 washes.
14 A nonrandomized open label pilot study with 16 outdoor workers under actual field conditions showed that LLPI clothing provided 93% reduction in tick bites compared to standard tick bite prevention measures in North Carolina, USA.
14 A double-blind RCT with 159 outdoor workers reported that the effectiveness of LLPI uniforms for the prevention of work-related tick bites was 0.82 and 0.34 for the first and second years of follow-up.
15 These studies concluded LLPI clothing may be highly effective against tick bites. The use of LLPI clothing, especially trousers and socks, has been recommended for general tick-bite prevention.
16
The overall tick bite rate of the treatment and control groups after 4–5 months wearing socks was not different in this study. But the site of tick bite between the two groups was quite different. The tick bite in treatment group occurred above the trunk and did not occur in lower extremities. On the other hand, tick bites in lower extremities occurred among all five subjects in the control group who reported tick bite history during the study period. Ticks typically quest close to the ground in leaf litter. Because of this, the initial site of tick encounter for humans is likely to be on lower extremities, especially footwear.
1517 In previous study, the success of permethrin-treated clothing in reducing tick bites varied depending on the type of clothing. Permethrin-treated socks have been shown to be particularly effective in preventing tick bites.
17
Another point of interest is that the tick bites in subjects wearing LLPI socks only occurred on the trunk and above. We speculate that the LLPI socks acted as a barrier, preventing the tick from crawling further up the body.
Due to the open-label nature of this study, it is possible that subjects who selected to be in the treatment group may be different than subjects who were in the control group. Since this study was not blinded, subjects may have altered their behavior regarding tick bite prevention measures based on their sock status. But we conducted intention-to-treat analysis to minimize the effect of bias. Tick bites were assessed using a self-reported manner. Therefore, it might have been affected by the recognition of the respondents.
To the best of our knowledge, this study is the first RCT to evaluate the effectiveness of LLPI socks in Korea. This study provides preliminary evidence that LLPI socks may be effective against tick bites in lower extremities. Future studies in a larger population with randomized treatment assignment are needed to determine whether LLPI clothing can prevent tick bites and tick-borne diseases.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download