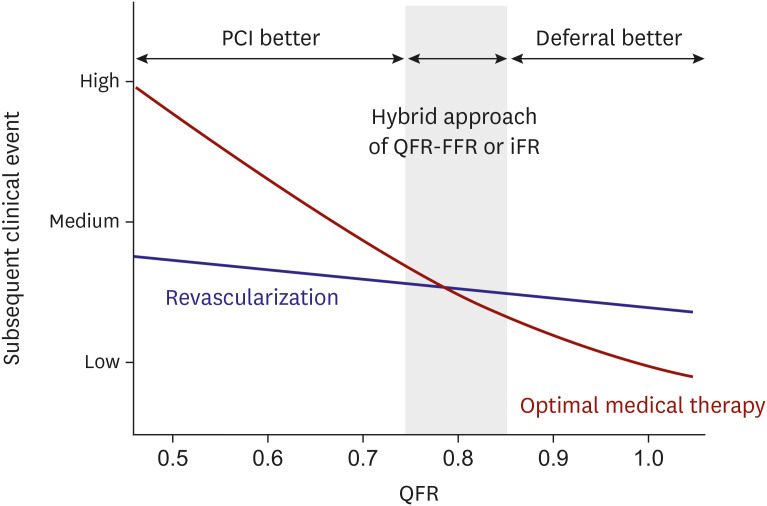
 | Figure 1QFR-FFR or iFR hybrid approach. In the gray zone of the QFR (0.75–0.85), adoption of an invasive physiologic measurement could improve the diagnostic accuracy.FFR = fractional flow reserve; iFR = instantaneous wave-free ratio; PCI = percutaneous coronary intervention; QFR = quantitative flow ratio.
|
Although the determination of myocardial ischemia is the first step in the evaluation of coronary artery disease, there is still a discrepancy between anatomical stenosis and the functional severity.1) The fractional flow reserve (FFR) is a useful index for invasively evaluating lesion-specific myocardial ischemia. Compared with angiography- or intravascular ultrasound-guided percutaneous coronary intervention (PCI), physiology-guided PCI significantly reduces the rate of cardiac events as well as decreases the number of stents and amount of contrast agent.2)3)4) However, the adoption of FFR in routine practice has lagged despite its clinical benefit.5) Potential reasons are the lengthy procedure to perform the FFR measurements, equipment and drug costs, and high incidence of patient-related discomfort. Because the instantaneous wave-free ratio (iFR) derived from resting gradients alone is quicker and does not require the administration of hyperemic agents, it is an alternative to FFR and largescale clinical studies have demonstrated the use of iFR as an alternative to FFR.6) Nevertheless, the need for interrogating the stenosis with a pressure wire and cost of the equipment have limited its widespread adoption. Recently less invasive techniques, such as FFR derived from computed tomography and quantitative flow ratio (QFR), have been developed to overcome the weaknesses of invasive physiologic measurements.
QFR is a 3-dimensional quantitative coronary angiography for calculating the FFR from angiographic images and does not require the introduction of an invasive pressure wire in the coronary artery or induction of hyperemia. At least 2 adequate contrast-filled angiographic projections >25° apart (with minimum overlap) were acquired and a 3-dimensional model reconstruction was performed. By utilizing the thrombolysis in myocardial infarction (TIMI) frame counting method, the contrast flow velocity was estimated, and software automatically calculated the contrast QFR value. In the FAVOR pilot study of 73 patients with 84 vessels, the QFR showed good agreement with the pressure wire-determined standard FFR measurements and had an accuracy of 86% for the diagnosis of ischemia defined according to an FFR ≤0.80.7) The FAVOR II study, which was an adequately powered multicenter study of 308 patients with 332 vessels, the patient- and vessel-level diagnostic accuracy of the QFR was 92.4% and 92.7%, respectively.8) However, the diagnostic accuracy of the QFR versus FFR can differ according to the reference index used to define myocardial ischemia. As the diagnostic performance of the invasive physiological indices was compared using positron emission tomography (PET) as the reference standard,9) QFR also should be validated with PET, which is considered the most accurate noninvasive myocardial perfusion imaging to define myocardial ischemia.
Dai et al.10) compared the QFR, FFR, and iFR for the response to the different degrees of the anatomical and hemodynamic stenosis severity and diagnostic performance against PET-derived parameters. This was the first study to investigate the association of the QFR with the PET-derived hemodynamic indices in comparison to the invasive physiologic measurements of the FFR and iFR. From 109 patients with 185 vessels, the authors employed the PET-derived relative flow reserve (RFR), coronary flow reserve (CFR), and coronary flow capacity (CFC) as independent references. The QFR demonstrated a similar response to different anatomic and hemodynamic stenosis severities for the FFR or iFR. There was no difference among the diagnostic accuracies of the 3 indices for the CFR. However, its diagnostic performance was inferior to the FFR and iFR when the PET-derived RFR and CFC were used as a reference. The discordance between the QFR and FFR or iFR was associated with a dependency of the QFR on the anatomical stenosis severity and assumption of the hemodynamic status. Because the QFR computations incorporate the TIMI frame count in its calculation algorithm, the presence of microvascular dysfunction may affect the QFR. Accordingly, an invasively measured physiologic assessment has a better performance in defining ischemia-causing stenosis. An advantage of the QFR is the indirect physiologic measurement derived from an anatomic parameter. However, a QFR analysis also requires a learning curve for the image acquisition and subsequent computation. Further, some anatomic issues (e.g., bifurcation lesions, ostial lesions, severe vessel tortuosity, and diffuse long lesions) still remain. In this study, the QFR could not be measured in all cases with an exclusion rate of 33.9%. While awaiting steady evidence that a QFR-based strategy shows an acceptable clinical outcome as compared to the FFR or iFR, a hybrid approach with QFR-FFR or iFR could be the first step toward a reliable assessment (Figure 1). For lesions with a QFR value in the gray zone, additional measurements of the FFR or iFR could improve the discrimination ability. An adoption of a machine learning-based analysis could give a high accuracy and consistent performance, and the use of the QFR could become wider even in the future.
Notes
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The contents of the report are the author's own views and do not necessarily reflect the views of the Korean Circulation Journal.
Go to : 
References
1. Cho YK, Nam CW, Han JK, et al. Usefulness of combined intravascular ultrasound parameters to predict functional significance of coronary artery stenosis and determinants of mismatch. EuroIntervention. 2015; 11:163–170. PMID: 26093837.


2. Nam CW, Yoon HJ, Cho YK, et al. Outcomes of percutaneous coronary intervention in intermediate coronary artery disease: fractional flow reserve-guided versus intravascular ultrasound-guided. JACC Cardiovasc Interv. 2010; 3:812–817. PMID: 20723852.

3. Cho YK, Nam CW. Percutaneous coronary intervention in patients with multi-vessel coronary artery disease: a focus on physiology. Korean J Intern Med. 2018; 33:851–859. PMID: 29551050.



4. Lee JM, Choi KH, Doh JH, et al. Long-term patient prognostication by coronary flow reserve and index of microcirculatory resistance: international registry of comprehensive physiologic assessment. Korean Circ J. 2020; 50:890–903. PMID: 32725991.



5. Kim JH, Choi W, Kim KC, et al. The current status of intervention for intermediate coronary stenosis in the Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circ J. 2019; 49:1022–1032. PMID: 31190480.



6. Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N Engl J Med. 2017; 376:1813–1823. PMID: 28317438.
7. Tu S, Westra J, Yang J, et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the International Multicenter FAVOR Pilot Study. JACC Cardiovasc Interv. 2016; 9:2024–2035. PMID: 27712739.

8. Xu B, Tu S, Qiao S, et al. Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol. 2017; 70:3077–3087. PMID: 29101020.

9. Hwang D, Jeon KH, Lee JM, et al. Diagnostic performance of resting and hyperemic invasive physiological indices to define myocardial ischemia: validation with 13N-ammonia positron emission tomography. JACC Cardiovasc Interv. 2017; 10:751–760. PMID: 28365268.

10. Dai N, Hwang D, Lee JM, et al. Association of quantitative flow ratio with lesion severity and its ability to discriminate myocardial ischemia. Korean Circ J. 2021; 51:126–139. PMID: 33525067.


Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download