INTRODUCTION
Coronavirus disease 2019 (COVID-19) is widespread worldwide and has become a global threat. After the identification of the first COVID-19 patient in January 2020 in Wuhan, the number of confirmed patients has been increasing rapidly. According to the World Health Organization situation report on July 24, 2020, there have been 15,296,926 confirmed cases and 628,903 COVID-19 deaths globally.
1 Korea experienced the COVID-19 outbreak earlier than many other countries. On March 2, 2020, the number of confirmed cases in Korea was 4,212, which was the second highest number after China.
2 However, the curve flattened as the Korean government implemented policies to reduce the transmission of the disease, and as of July 23, the number of confirmed cases was approximately 14,000.
3 To control the spread of COVID-19, social distancing measures were implemented, and the crisis alert level was raised incrementally as the number of confirmed COVID-19 cases increased.
24
Several reports have shown that the number of emergency department (ED) visits has decreased worldwide after the start of the COVID-19 pandemic.
56 The total number of ED visits in the United States (US) decreased by 42% during the early pandemic period compared to the previous year.
5 A single center study in the US also reported a 49.3% decrease in the number of ED patients, with relatively larger decreases in pediatric and older patients.
7 Similar trends were also observed in previous infectious disease outbreaks, such as the Middle East Respiratory Syndrome (MERS) and severe acute respiratory syndrome outbreaks.
89
Understanding the changes in ED visit patterns during the COVID-19 pandemic is important to facilitating an effective response. Although there have been some studies that have addressed the impact of the COVID-19 on ED visits,
5710 few have focused on the pediatric population, which had been found to be the most strongly affected population.
11
In this multicenter study, we aimed to analyze the changes in ED visit patterns in children before and during the COVID-19 outbreak. First, we hypothesized that the number of children visiting the ED would be lower during the outbreak than in the previous year. Second, we hypothesized that the degree of stringency of the national government social distancing measures would be associated with the decrease in ED utilization by children. Our third hypothesis was that the characteristics and outcomes of the children visiting the ED would be different before and during the COVID-19 pandemic.
METHODS
Study design and setting
We performed a retrospective observational study in 5 tertiary hospitals in Korea (Seoul National University Hospital, Seoul National University Bundang Hospital, Gachon University Gil Medical Center, Samsung Medical Center, Ajou University Hospital), which have an annual ED volume ranging from 65,000 to 95,000. We used each study hospital's National Emergency Department Information System (NEDIS) data to acquire the demographics and outcomes of the study participants. The NEDIS is a nationwide emergency medical care database in Korea, and systematic quality control is conducted to ensure the quality of the data.
12 We obtained data on government social distancing policy measures from the Oxford COVID-19 Government Response Tracker (OxCGRT). The OxCGRT collects information on government policies in response to the COVID-19 pandemic, such as school closures and closure restrictions. The Government Response Stringency Index (GRSI) is a composite measure based on 9 social distancing indicators and ranges from 0 to 100. The OxCGRT database has been described in previously published articles.
1314 The number of daily confirmed COVID-19 cases was acquired from the Korean Centers for Disease Control and Prevention reports.
3
The data pertaining to pediatric ED visits between June 1, 2018, and May 31, 2020, were used to analyze the overall trends in visits before and during the COVID-19 pandemic. To evaluate the effect of the degree of stringency of the social distancing measures on the number of ED visits, a Poisson regression model was constructed with month, year, and the average monthly GRSI as fixed effects.
We compared ED visits during the COVID-19 period and in same period in the previous year. February 1, 2020, to May 31, 2020, was defined as the COVID-19 period, and February 1, 2019, to May 31, 2019, was defined as the reference period. The reason for this definition was that in Korea, the first COVID-19 patient was identified in late January 2020, and the number of confirmed patients started to increase dramatically in February 2020. Patient demographics and ED results were compared between the two periods. The top five most frequent chief complaints and common ED diagnoses of patients were also compared.
The number of pediatric ED visits to a hospital can be affected by the existence of a specialist in pediatric emergency care. Changes in nearby pediatric EDs can bring changes in the patient population and affect our study. However, there were no newly opening or closing of secondary or tertiary hospital pediatric centers nearby the study hospitals during the study period. All of the study hospital EDs had pediatric emergency care specialists for 24 hours a day. The number of specialists had only minor changes of one or two during the study period.
Selection of participants
All patients under the age of 18 years who visited one of the study hospital EDs between June 1, 2018, and May 31, 2020, were included. Patients with missing demographic information, ED triage level, or ED outcomes were excluded. Patients who visited the ED for nonmedical reasons, such as the issuing of medical records or certificates, were also excluded. Multiple ED visits during the study period from the same patient were considered separate visits.
Measurements
Patient age, sex, mode of arrival (ambulance use vs. nonuse), time of ED visit (daytime vs. nighttime), time of symptom onset, ED triage level, chief complaint, ED length of stay (LOS), ED diagnosis, and status at discharge from the ED were retrieved from each hospital's NEDIS database. Information on whether the patient visit was due to an injury was collected. We subdivided the patients into 4 groups by age in accordance with previous literature: younger than 2 years (infancy and toddlerhood), 2 to 5 years (early childhood), 6 to 11 years (middle childhood), and 12 to 17 years (adolescence).
15 Daytime was defined as 6 AM to 6 PM, and nighttime was defined as 6 PM to 6 AM. Since 2016, ED triage has been performed using the Korean Triage and Acuity Scale (KTAS) in Korea. The KTAS was developed based on the Canadian Triage and Acuity Scale and has 5 levels: level 1, resuscitation; level 2, emergency; level 3, urgent; level 4, less urgent; and level 5, nonurgent. The ED diagnosis was recorded based on the Korean Standard Classification of Diseases and Causes of Death 7 (KCD-7) codes, which has been modified from the International Statistical Classification of Diseases and Related Health Problems 10 to suit the circumstances in Korea.
16 Only the primary diagnosis codes were used for the analysis. A patient's status at discharge was classified as one of the following: discharge, discharge against medical advice, admission, transfer, or death. We were not able to acquire the variable time of onset of symptoms of Samsung Medical Center due to the hospital's regulations. Therefore, when analyzing the time from symptom onset to ED arrival, we excluded the data from Samsung Medical Center.
Statistical analysis
The number of monthly ED visits during the study period, the average monthly Korean GRSI and the monthly number of confirmed COVID-19 cases nationwide were analyzed together to show the overall trends. The Poisson model included month and year (June 2018 to May 2019 vs. June 2019 to May 2020) to account for monthly and yearly changes in pediatric ED visits. The coefficient for the GRSI variable represents the change in the number of ED visits based on the degree of stringency of the social distancing measures. To assess the goodness of fit of the Poisson model, a scaled Pearson chi-square test was used to correct for overdispersion. The characteristics and outcomes of the patients who visited the ED during the COVID-19 period were compared with those during the reference period. We calculated the percent decrease and its 95% confidence interval (CI) for each category by dividing the proportion of ED visits during the COVID-19 period by the proportion of visits during the reference period. Categorical variables are expressed using frequencies and proportions. Continuous variables are shown using medians and interquartile ranges. The chi-square test and Wilcoxon rank sum test were used to compare the two groups, as appropriate. A P value less than 0.05 was considered significant. All analyses were performed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The institutional review board at each of the study hospitals approved this project and waived the need to obtain informed consent (Seoul National University Hospital: 2006-148-1134, Seoul National University Bundang Hospital: B-2009636-402, Gachon University Gil Medical Center: GDIRB2020-355, Samsung Medical Center: 2020-06-149, Ajou University Hospital: AJIRB-MED-MDB-20-376).
RESULTS
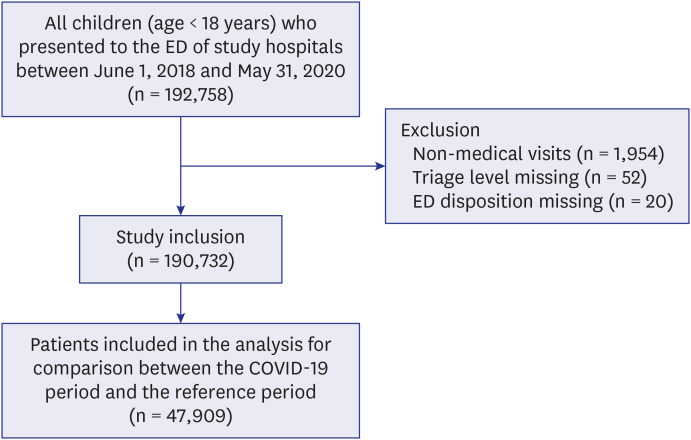
Fig. 1 depicts the flowchart of this study. A total of 192,758 children younger than 18 years presented to the ED during the study period. After exclusion, a total of 190,732 patients were included in the study. For the comparison between the COVID-19 period and the reference period, 47,909 patients were analyzed.
Fig. 1
Patient flow chart.
ED = emergency department, COVID-19 = coronavirus disease 2019.
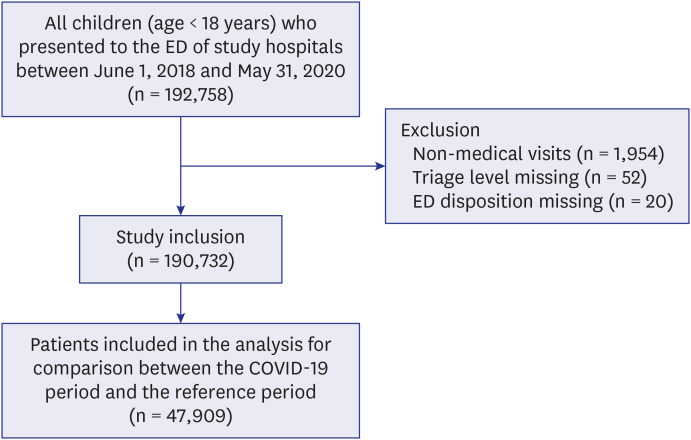
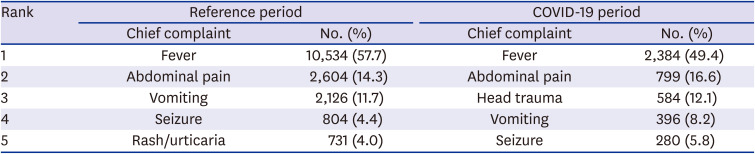
Fig. 2 shows the overall trends in the number of ED visits, confirmed COVID-19 cases in Korea, and average monthly GRSI during the study period. Between January 2020 and February 2020, the number of ED visits dropped from 8,756 to 3,791, decreasing by 56.7%. The number of ED visits reached the lowest point in March 2020 and recovered slowly thereafter. The number of confirmed COVID-19 cases in Korea reached a peak in March 2020 (6,636) and then declined sharply. The GRSI increased as the number of monthly confirmed COVID-19 cases in Korea increased but reached the peak slightly later in April 2020.
Fig. 2
Trends in emergency department visits. The number of ED visits, number of monthly confirmed COVID-19 cases and average monthly GRSI values in Korea are shown.
ED = emergency department, COVID-19 = coronavirus disease 2019, GRSI = Government Response Stringency Index.

The Poisson regression model using year, month, and GRSI as fixed effects was well fitted (
P value 0.440). Even after controlling for year and month, the GRSI was significantly associated with the number of monthly ED visits (
P value < 0.001). For every 10-point increase in the GRSI, there was a 15.1% (95% CI, 12.9%–17.4%) decrease in the number of monthly ED visits (
Supplementary Data 1). After controlling for month and GRSI, year (June 2018 to May 2019 vs. June 2019 to May 2020) was not significantly associated with the number of monthly ED visits (
P value 0.875).
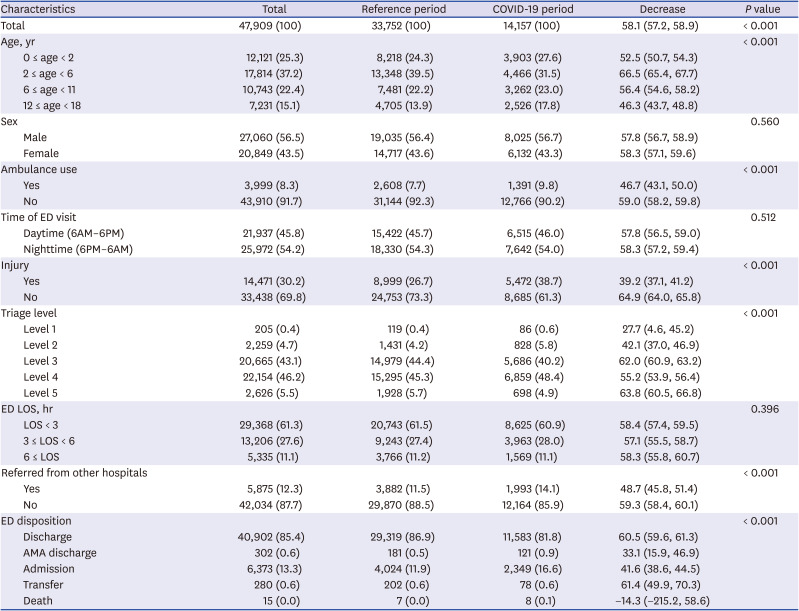
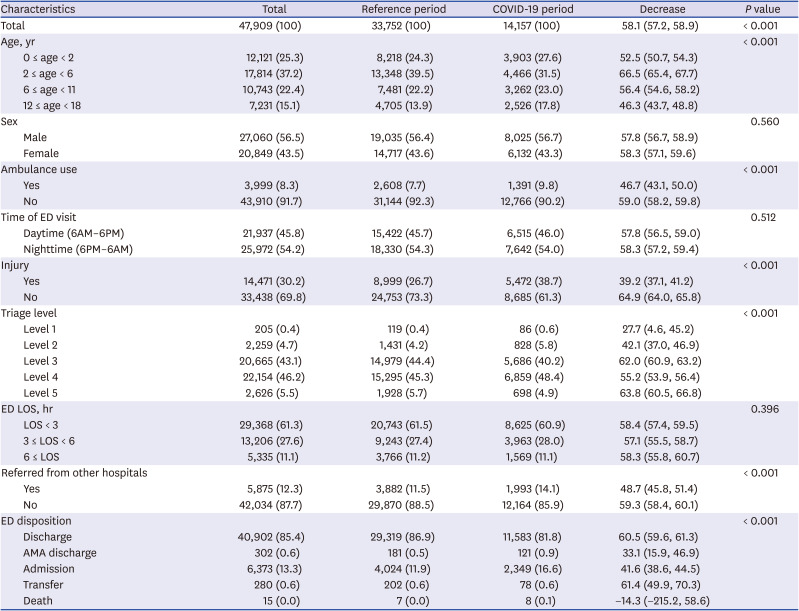
The characteristics of the patients who visited the ED during the reference period and the COVID-19 period are shown in
Table 1. A total of 33,752 and 14,157 patients visited the ED during the reference period and the COVID-19 period, respectively, with a 58.1% (95% CI, 57.2%–58.9%) decline. The number of patients decreased the most in the early childhood age group (66.5%), while the number decreased the least in adolescents (46.3%). There were disproportionately greater decreases in low-acuity (triage level 3–5) patients (55.2%–63.8%), those who did not use an ambulance (59.0%), and those who came to the ED for noninjury complaints (64.9%). In the adolescent group, injuries were the primary reason for 70% of ED visits during the reference period and 75% of ED visits during the COVID-19 period. The proportion of patients who were referred from other hospitals increased from 11.5% to 14.1%. Disproportionately greater decreases were observed in the numbers of discharged (60.5%) and transferred (61.4%) patients. The proportion of admitted patients increased from 11.9% to 16.6%, while the proportion of discharged patients decreased from 86.9% to 81.8%.
Table 1
Characteristics of the patients who visited the ED during the reference and the COVID-19 period
|
Characteristics |
Total |
Reference period |
COVID-19 period |
Decrease |
P value |
|
Total |
47,909 (100) |
33,752 (100) |
14,157 (100) |
58.1 (57.2, 58.9) |
< 0.001 |
|
Age, yr |
|
|
|
|
< 0.001 |
|
0 ≤ age < 2 |
12,121 (25.3) |
8,218 (24.3) |
3,903 (27.6) |
52.5 (50.7, 54.3) |
|
2 ≤ age < 6 |
17,814 (37.2) |
13,348 (39.5) |
4,466 (31.5) |
66.5 (65.4, 67.7) |
|
6 ≤ age < 11 |
10,743 (22.4) |
7,481 (22.2) |
3,262 (23.0) |
56.4 (54.6, 58.2) |
|
12 ≤ age < 18 |
7,231 (15.1) |
4,705 (13.9) |
2,526 (17.8) |
46.3 (43.7, 48.8) |
|
Sex |
|
|
|
|
0.560 |
|
Male |
27,060 (56.5) |
19,035 (56.4) |
8,025 (56.7) |
57.8 (56.7, 58.9) |
|
Female |
20,849 (43.5) |
14,717 (43.6) |
6,132 (43.3) |
58.3 (57.1, 59.6) |
|
Ambulance use |
|
|
|
|
< 0.001 |
|
Yes |
3,999 (8.3) |
2,608 (7.7) |
1,391 (9.8) |
46.7 (43.1, 50.0) |
|
No |
43,910 (91.7) |
31,144 (92.3) |
12,766 (90.2) |
59.0 (58.2, 59.8) |
|
Time of ED visit |
|
|
|
|
0.512 |
|
Daytime (6AM–6PM) |
21,937 (45.8) |
15,422 (45.7) |
6,515 (46.0) |
57.8 (56.5, 59.0) |
|
Nighttime (6PM–6AM) |
25,972 (54.2) |
18,330 (54.3) |
7,642 (54.0) |
58.3 (57.2, 59.4) |
|
Injury |
|
|
|
|
< 0.001 |
|
Yes |
14,471 (30.2) |
8,999 (26.7) |
5,472 (38.7) |
39.2 (37.1, 41.2) |
|
No |
33,438 (69.8) |
24,753 (73.3) |
8,685 (61.3) |
64.9 (64.0, 65.8) |
|
Triage level |
|
|
|
|
< 0.001 |
|
Level 1 |
205 (0.4) |
119 (0.4) |
86 (0.6) |
27.7 (4.6, 45.2) |
|
Level 2 |
2,259 (4.7) |
1,431 (4.2) |
828 (5.8) |
42.1 (37.0, 46.9) |
|
Level 3 |
20,665 (43.1) |
14,979 (44.4) |
5,686 (40.2) |
62.0 (60.9, 63.2) |
|
Level 4 |
22,154 (46.2) |
15,295 (45.3) |
6,859 (48.4) |
55.2 (53.9, 56.4) |
|
Level 5 |
2,626 (5.5) |
1,928 (5.7) |
698 (4.9) |
63.8 (60.5, 66.8) |
|
ED LOS, hr |
|
|
|
|
0.396 |
|
LOS < 3 |
29,368 (61.3) |
20,743 (61.5) |
8,625 (60.9) |
58.4 (57.4, 59.5) |
|
3 ≤ LOS < 6 |
13,206 (27.6) |
9,243 (27.4) |
3,963 (28.0) |
57.1 (55.5, 58.7) |
|
6 ≤ LOS |
5,335 (11.1) |
3,766 (11.2) |
1,569 (11.1) |
58.3 (55.8, 60.7) |
|
Referred from other hospitals |
|
|
|
|
< 0.001 |
|
Yes |
5,875 (12.3) |
3,882 (11.5) |
1,993 (14.1) |
48.7 (45.8, 51.4) |
|
No |
42,034 (87.7) |
29,870 (88.5) |
12,164 (85.9) |
59.3 (58.4, 60.1) |
|
ED disposition |
|
|
|
|
< 0.001 |
|
Discharge |
40,902 (85.4) |
29,319 (86.9) |
11,583 (81.8) |
60.5 (59.6, 61.3) |
|
AMA discharge |
302 (0.6) |
181 (0.5) |
121 (0.9) |
33.1 (15.9, 46.9) |
|
Admission |
6,373 (13.3) |
4,024 (11.9) |
2,349 (16.6) |
41.6 (38.6, 44.5) |
|
Transfer |
280 (0.6) |
202 (0.6) |
78 (0.6) |
61.4 (49.9, 70.3) |
|
Death |
15 (0.0) |
7 (0.0) |
8 (0.1) |
−14.3 (−215.2, 58.6) |
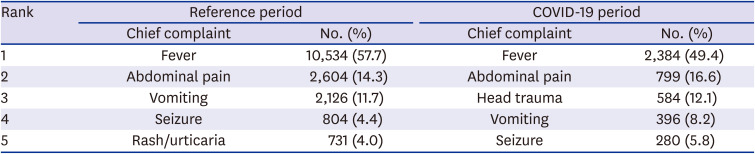
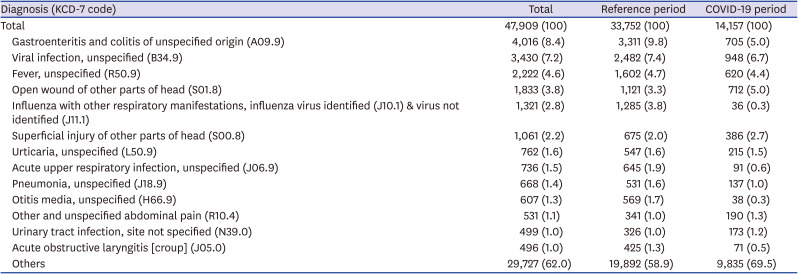
The top five most common chief ED complaints in the reference period were fever (57.7%), abdominal pain (14.3%), vomiting (11.7%), seizure (4.4%), and rash/urticaria (4.0%), in decreasing order. The top five most common chief ED complaints in the COVID-19 period were fever (49.4%), abdominal pain (16.6%), head trauma (12.1%), vomiting (8.2%), and seizure (5.8%), in decreasing order (
Table 2).
Table 2
Top five most common ED chief complaints in the reference and the COVID-19 period
|
Rank |
Reference period |
COVID-19 period |
|
Chief complaint |
No. (%) |
Chief complaint |
No. (%) |
|
1 |
Fever |
10,534 (57.7) |
Fever |
2,384 (49.4) |
|
2 |
Abdominal pain |
2,604 (14.3) |
Abdominal pain |
799 (16.6) |
|
3 |
Vomiting |
2,126 (11.7) |
Head trauma |
584 (12.1) |
|
4 |
Seizure |
804 (4.4) |
Vomiting |
396 (8.2) |
|
5 |
Rash/urticaria |
731 (4.0) |
Seizure |
280 (5.8) |
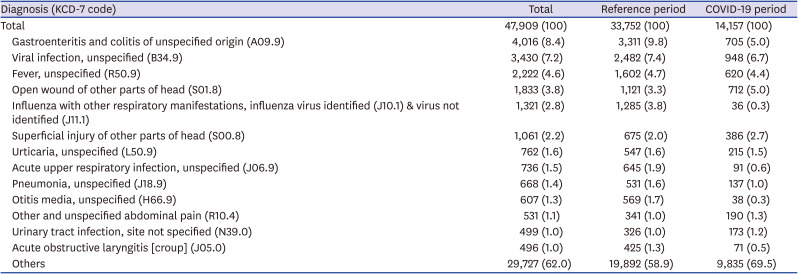
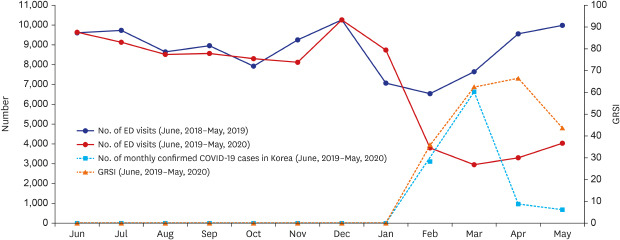
Table 3 shows the number of children diagnosed with each disease or injury. The proportion of children diagnosed with infectious diseases such as gastroenteritis and colitis, viral infection, influenza, upper respiratory infection, pneumonia, acute otitis media, and croup decreased significantly. The number of patients who were diagnosed with influenza during the COVID-19 period decreased by 97% compared to the number during the reference period. On the other hand, the proportion of patients with the diagnosis related to head injury increased. The proportion of diagnoses of urticaria, abdominal pain, and urinary tract infection remained similar in both periods.
Table 3
Common ED diagnoses during the reference and the COVID-19 period
|
Diagnosis (KCD-7 code) |
Total |
Reference period |
COVID-19 period |
|
Total |
47,909 (100) |
33,752 (100) |
14,157 (100) |
|
Gastroenteritis and colitis of unspecified origin (A09.9) |
4,016 (8.4) |
3,311 (9.8) |
705 (5.0) |
|
Viral infection, unspecified (B34.9) |
3,430 (7.2) |
2,482 (7.4) |
948 (6.7) |
|
Fever, unspecified (R50.9) |
2,222 (4.6) |
1,602 (4.7) |
620 (4.4) |
|
Open wound of other parts of head (S01.8) |
1,833 (3.8) |
1,121 (3.3) |
712 (5.0) |
|
Influenza with other respiratory manifestations, influenza virus identified (J10.1) & virus not identified (J11.1) |
1,321 (2.8) |
1,285 (3.8) |
36 (0.3) |
|
Superficial injury of other parts of head (S00.8) |
1,061 (2.2) |
675 (2.0) |
386 (2.7) |
|
Urticaria, unspecified (L50.9) |
762 (1.6) |
547 (1.6) |
215 (1.5) |
|
Acute upper respiratory infection, unspecified (J06.9) |
736 (1.5) |
645 (1.9) |
91 (0.6) |
|
Pneumonia, unspecified (J18.9) |
668 (1.4) |
531 (1.6) |
137 (1.0) |
|
Otitis media, unspecified (H66.9) |
607 (1.3) |
569 (1.7) |
38 (0.3) |
|
Other and unspecified abdominal pain (R10.4) |
531 (1.1) |
341 (1.0) |
190 (1.3) |
|
Urinary tract infection, site not specified (N39.0) |
499 (1.0) |
326 (1.0) |
173 (1.2) |
|
Acute obstructive laryngitis [croup] (J05.0) |
496 (1.0) |
425 (1.3) |
71 (0.5) |
|
Others |
29,727 (62.0) |
19,892 (58.9) |
9,835 (69.5) |
After removing the Samsung Medical Center data, we used the data of the remaining 4 hospitals to analyze the time from symptom onset to ED visit. There were 12,268 ED visits during the COVID-19 period and 29,673 visits during the reference period in this population. During the COVID-19 period, the median time from symptom onset to ED visit was 4 (1–25) hours. The time from symptom onset to ED visit was significantly longer in the reference period (8 [1–35] hours, P value < 0.001).
DISCUSSION
In this multicenter retrospective study, we observed a significant decrease in pediatric ED visits after the start of the COVID-19 pandemic. The number of pediatric ED visits during the COVID-19 period declined by 58.1% compared to the previous year. The number of ED visits dropped to the lowest level in March 2020, when the number of newly confirmed COVID-19 cases in Korea reached the maximum. There were disproportionate declines in the numbers of ED visits for specific groups: children in early childhood, low-acuity children, those who did not use an ambulance, and those who came to the ED for noninjury complaints. In terms of ED outcomes, the frequency of the diagnosis of infectious diseases, especially influenza, significantly declined. The proportion of admitted patients increased, while the proportion of discharged patients decreased compared to the reference period. The Poisson regression model was well fitted, and we observed a 15.1% decrease in monthly ED visits for every 10-point increase in the GRSI.
The decrease in ED utilization may be explained by several factors. First, fear of being exposed to COVID-19 in healthcare facilities may have had an impact on the behavior of Koreans. EDs in Korea experienced a similar decrease in ED volume during the MERS outbreak in 2015, as it was suggested that healthcare facilities were the primary locations of virus transmission.
9 In a study performed in Italy, 12 cases of delayed access to hospital care were analyzed.
10 Surprisingly, the parents reported avoiding using the hospital because of the fear of COVID-19 in all cases. In a survey conducted in Korea, 92.3% of the respondents answered that they avoided healthcare facilities as a means of social distancing.
4 Second, social distancing policies may have directly affected the incidence of injuries and diseases. In the same survey mentioned above, 96.7%, 87.4%, and 83.4% of the participants responded that they avoided outdoor activities, public transportation, and crowded places, respectively.
4 Avoiding travel and outdoor activities may have resulted in a decrease in the number of injuries. Other social distancing measures could have resulted in a decrease in close contact between people, leading to a decreased transmission of infectious diseases. The decrease in the incidence of the infectious diseases in the ED is one of the pieces of evidence that supports this possibility. In our study, the diagnosis of influenza in the ED decreased by 97% compared to the previous year. Gastrointestinal and respiratory infectious diseases seem to have decreased the most. Similar results were reported from the US, showing a 95% decrease among children younger than 11 years old.
5 Third, the closure of schools, kindergartens, and daycare centers may have had a significant impact, especially on the pediatric population. As COVID-19 spread nationwide, the Korean government delayed the start of the new school year.
2 As an alternative to going to school in person, online classes started in April. Then, after the first surge of the COVID-19 pandemic subsided, high school seniors started to go to school on May 20, 2020, and the rest of the students followed gradually thereafter. Therefore, during the COVID-19 period defined in this study as extending from February to May 2020, school closures may have significantly affected the ED utilization patterns of children.
The characteristics of the children visiting the EDs changed during the COVID-19 pandemic. In the reference period, 26.7% were injury patients, whereas in the COVID-19 period, this increased to 38.7%. Head trauma was the third most common chief complaint in the COVID-19 period. It seems that the number of head trauma visits showed a smaller decrease because many children sustain head injury indoors.
17 In social distancing periods where outdoor activities are limited, indoor injuries can become relatively more common. A similar increase in the proportion of trauma patients was also observed during the MERS outbreak, and it was suspected that these pediatric trauma patients could not be easily treated in primary medical institutions in Korea.
9 In the adolescent group, injury accounted for 75% of ED visits during the COVID-19 period in our study. This may be the reason for the relatively smaller decrease in the number of ED visits in this age group. In a study conducted in Italy, the proportion of trauma patients decreased during the COVID-19 period.
10 That study mentioned that there was an almost complete cessation of traffic and sports activities. Additionally, COVID-19 patients accounted for a high portion of ED visits. These differences may explain the conflicting results.
The disproportionate decrease in the number of low-acuity patients may indicate the traditional overuse of ED resources by this patient group. However, we must be cautious when interpreting this result. There is evidence that delayed access to the hospital due to fear of COVID-19 has led to increased morbidity and mortality.
18 The increased proportion of patients using ambulances was probably due to the increased proportion of high-acuity patients. The reason for the increase in admission rate is also associated with acuity. The increase in referred patients may be because all of our study hospitals are tertiary hospitals which provide treatment for patients who are severely ill or have chronic comorbidities. Such patients are frequently referred from primary and secondary hospitals even during the pandemic. Unlike expected, patients' time from symptom onset to ED visit has reduced during the COVID-19 pandemic. Patients avoid hospitals during the pandemic, causing a drop in the overall visits to EDs, but those who need medical care seems to rush to the hospital with concerns.
The decrease in ED visits of children may impact the society in several ways. The decrease in low-acuity patients allows ED physicians to concentrate their efforts on treating severe, urgent patients. Although it may be transient, ED crowding may also be alleviated. The decrease in infectious diseases due to social distancing can have some positive effects on the public health of children. However, the training of ED residents may become a problem due to the decreased volume of patients. Lo et al.
19 reported that the average number of pediatric patients managed by residents decreased from 1.56 to 0.51 during the pandemic. To maintain the quality of ED resident training, new education programs should be considered. Also, EDs, especially those in tertiary hospitals, should be prepared to accept transferred patients from other hospitals during a pandemic. Some hospitals can become occupied by COVID-19 patients and have no choice but to transfer their ED patients to available hospitals.
To our knowledge, this is the first study to model the number of monthly ED visits in relation to the degree of stringency of social distancing measures during the early period of the COVID-19 pandemic. The degree of stringency of social distancing policies, measured using the GRSI, was significantly associated with the number of monthly ED visits, even after adjusting for month and year. Governments implement stricter social distancing policies when the pandemic is more severe. Therefore, the GRSI can be thought of as an index that represents both the stringency of the social distancing measures and the severity of the pandemic.
There are several important limitations of this study. First, this study was conducted at 5 tertiary hospital EDs in Korea, and our results may not be generalizable to other EDs. Nonetheless, the study hospitals' EDs are the core EDs in the capital region and provide care to a large portion of the pediatric patients in the region. Second, this was a retrospective observational study, and we may not have captured all the data needed to explain the changes in ED visits. There may have been unrecognized factors other than COVID-19 that affected the results of our study. However, it is almost impossible to conduct a prospective study to explore the changes during a pandemic. Given the circumstances, we performed a retrospective study using as much information as we could collect. Third, this study did not capture data after May 31, 2020. The patterns of ED utilization during the later COVID-19 pandemic period may be different from those in the early period. Fatigue from long-lasting social distancing measures and the decrease in the fear of COVID-19 as time passes may influence ED utilization patterns. Future studies with longer study periods are needed to observe the changes in ED visits after the COVID-19 pandemic has subsided.
In this study, we analyzed the changes in pediatric ED utilization patterns during the COVID-19 outbreak. A striking decrease in pediatric ED visits was observed, and the scale of this decrease was associated with the stringency of government social distancing policies. Changes in the number and characteristics of children visiting the ED should be taken into account when developing plans for the effective operation of EDs during the COVID-19 pandemic. Future studies that consider data from longer periods during the COVID-19 outbreak are needed to further explore the changes in ED utilization during the pandemic.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download