INTRODUCTION
Ocular trauma is a leading cause of preventable monocular blindness and visual impairment.
12 Globally, 19 million people suffer from trauma-related monocular blindness or low vision. In the United States, an estimated 2.0 to 2.4 million cases of ocular trauma, with many progressing to permanent vision loss, are recorded annually.
134 Ocular injuries associated with major trauma are vision threatening. Minor ocular injuries have been associated with considerable morbidity and time lost from work.
5 In Korea, out of 1,900,000 cases 70,000 (3.7%) major trauma cases occur each year according to data collected in 2018 by the Korean National Emergency Department Information System,
6 and the incidence increases every year. The current epidemiology of ocular injuries in patients with major trauma has been under-evaluated, despite its relevance to public health; there is no population-based or regional center-based study. However, such investigations are useful for injury prevention and are crucial.
The Pusan National University Hospital (PNUH) level 1 regional trauma center has four basement floors, 13 ground floors, 50 intensive care unit beds, and 84 general beds. It serves the urban and rural population up to 7,000,000 people. It is the first stand-alone trauma center in Korea and the biggest level 1 regional trauma center in Korea and Asia. We present the epidemiology, causes, and outcomes of ocular traumas over a 3-year period in patients with major trauma. We aimed to evaluate the efficacy of the conventional Ocular Trauma Score (OTS) system
7 and gain information on the incidence, subtypes, severity and risk factors of ocular trauma. This data will aid public health and allow the development of strategies to reduce the socioeconomic burden of ocular trauma on the healthcare system and community.
Go to :

RESULTS
Epidemiology
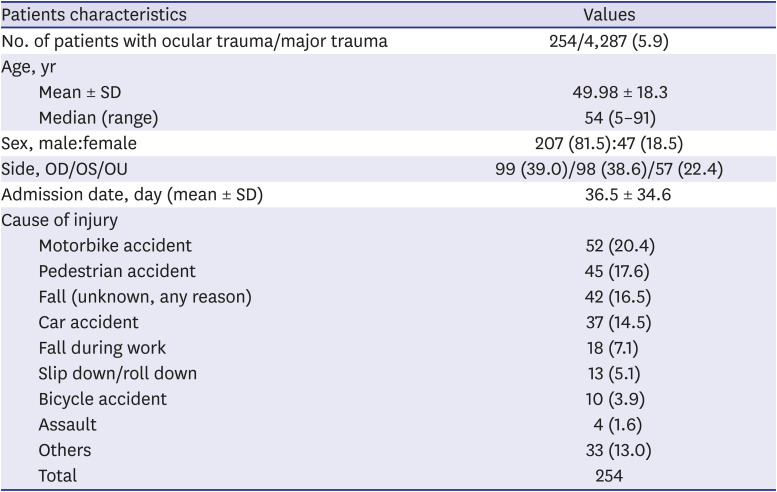
The patient's demographics and characteristics are summarized in
Table 1. In total, 307 ocular trauma (7.2%) patients were identified out of 4,287 major trauma patients. There were 100 (6.9%) out of 1,446 ocular trauma patients in 2016, 106 (7.5%) out of 1,416 in 2017, and 101 (7.1%) out of 1,425 in 2018. The complete electronic medical charts of 254 patients were successfully evaluated. The rest had insufficient medical records, including ophthalmological documentation due to poor cooperation, underwent emergent surgery, or did not arrive for their scheduled ophthalmology appointment or were transferred before final evaluation. Therefore, the studies of incidence involved 307 ocular trauma patients, while detailed analysis was conducted using data on the selected 254 patients. Among the patients who were excluded, 5 patients were excluded because of death.
Table 1
Patients demographics and characteristics
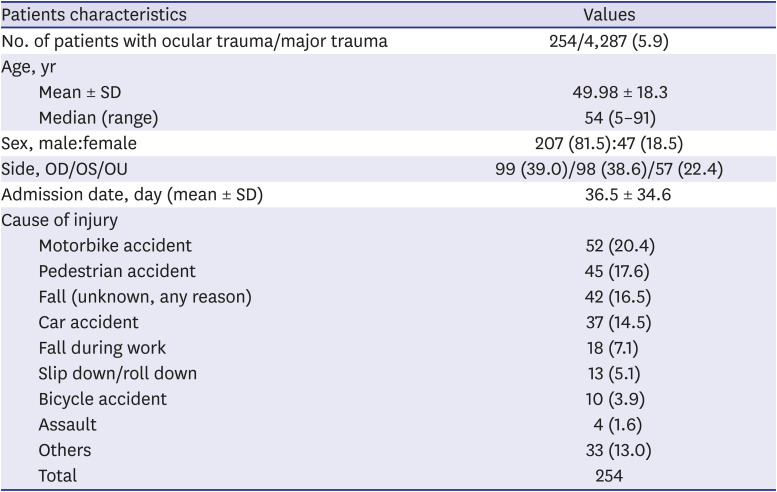
|
Patients characteristics |
Values |
|
No. of patients with ocular trauma/major trauma |
254/4,287 (5.9) |
|
Age, yr |
|
|
Mean ± SD |
49.98 ± 18.3 |
|
Median (range) |
54 (5–91) |
|
Sex, male:female |
207 (81.5):47 (18.5) |
|
Side, OD/OS/OU |
99 (39.0)/98 (38.6)/57 (22.4) |
|
Admission date, day (mean ± SD) |
36.5 ± 34.6 |
|
Cause of injury |
|
|
Motorbike accident |
52 (20.4) |
|
Pedestrian accident |
45 (17.6) |
|
Fall (unknown, any reason) |
42 (16.5) |
|
Car accident |
37 (14.5) |
|
Fall during work |
18 (7.1) |
|
Slip down/roll down |
13 (5.1) |
|
Bicycle accident |
10 (3.9) |
|
Assault |
4 (1.6) |
|
Others |
33 (13.0) |
|
Total |
254 |

The incidence rates of major trauma were 21.33/100,000, 20.94/100,000, and 20.91/100,000 in 2016, 2017 and 2018, respectively. The incidence rate of major trauma gradually decreased over time from 2016 to 2018. The incidence of ocular trauma patients with major trauma who were transferred or referred to the trauma center were 1.47/100,000, 1.57/100,000, and 1.48/100,000 in 2016, 2017 and 2018, respectively. The rate of ocular trauma was rather irregular for 3 years, despite the decrease in the total number of major trauma patients.
There were 207 (81.5%) male patients and 47 (18.5%) female patients in the study. The mean (standard deviation) age of ocular trauma patients were 49.98 ± 18.3 years, and the age range was 5 to 91 years. The median age was 54 years. There were 99 cases of right ocular trauma, 98 cases were left-sided, and 57 cases were bilateral.
We observed a mean time (hours) of 2.5 hours from arrival at the trauma center to the request for ophthalmologic consultation, and 6.7 hours from arrival at trauma center to examination by an ophthalmologist. There were 122 out of 254 patients evaluated and diagnosed by ophthalmology specialists. The mean time of hospitalization period at the trauma center was 36.5 ± 34.6 days.
Characteristics of trauma and ocular injuries
The frequencies for the most common causes of ocular trauma subsequent to major trauma were 52 (20.4%) cases of motorbike accidents, 45 (17.6%) of pedestrian accidents, and 42 (16.5%) of falls (any reason except fall during work). Thirty-seven patients (14.5%) were associated with in-car traffic accidents, 18 (7.1%) with falls during work, 13 (5.1%) slipped or rolled down, 10 (3.9%) suffered a bicycle accident, 4 (1.6%) were involved in assaults, and the remaining 33 (13.0%) were classified under ‘others’. Overall, road traffic accidents including motorbike accidents, pedestrian accidents, in-car traffic accidents, and bicycle accidents accounted for 144 (56.7%) cases and were the most common causes of ocular trauma associated with major trauma. Falls (including during work) accounted for 60 (23.6%) cases.
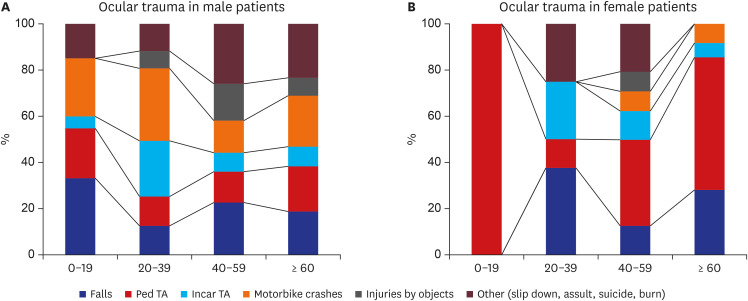
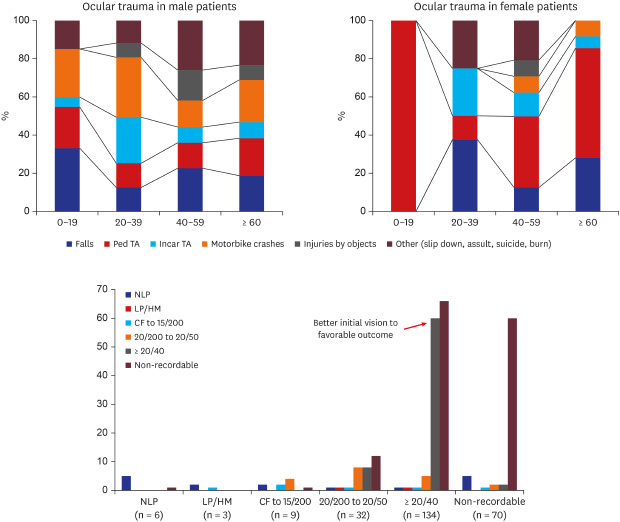
We present the causes of ocular trauma in patients with major trauma stratified by age and sex in
Fig. 1. Road traffic accidents were the main causes of ocular injuries in both sexes. Motorbike accidents were predominant in male patients, especially aged in their 10s and 20s. Pedestrian traffic accidents were the main causes in female patients. Falls were the second most common causes in both sexes.
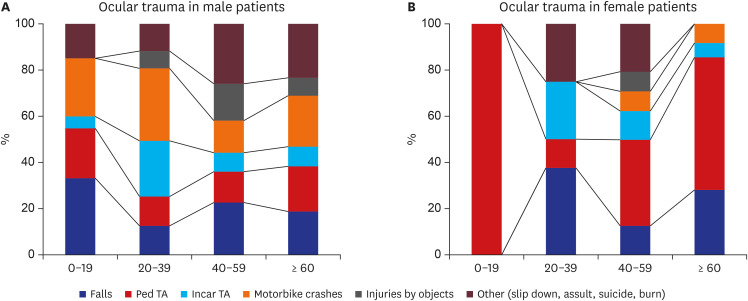 | Fig. 1
Causes of ocular trauma in patients with major trauma, stratified by age and sex. (A) Distribution of ocular trauma in male patients. More than half of the cases are related to the TAs including motorbike crashes. Especially in 10s–20s, the number of motorbike crashes were significantly higher than other age groups. (B) Distribution of ocular trauma in female patients. Falls and Ped TAs are mostly related major causes of ocular trauma.
TA = traffic accident, Ped = pedestrian.

|
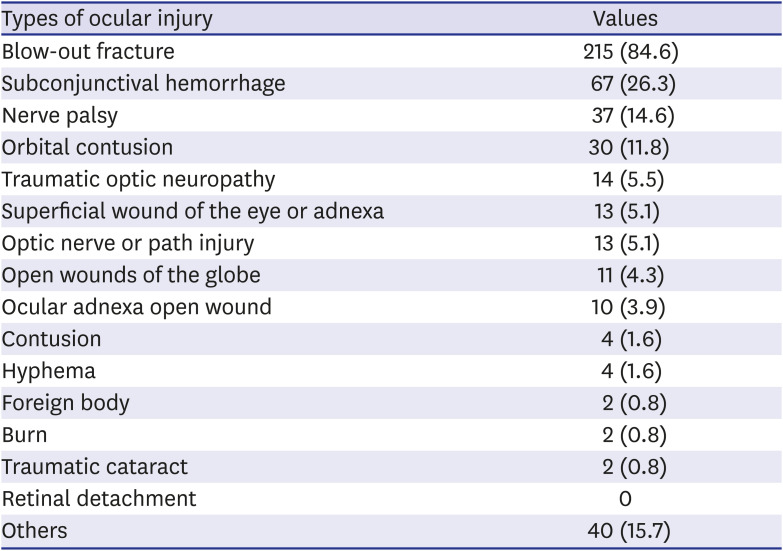
The types of ocular injuries and major trauma are illustrated in
Tables 2 and
3. Many patients had more than one diagnosis. The most frequent ocular injuries in patients with major trauma were blow-out fractures (n = 215, 84.6%). Out of these blow-out fracture cases, 52% were due to multiple traumas and were managed by trauma specialists at the trauma center and 50.2% were complex orbital and facial fractures. Only 26.5% were isolated blow-out fractures. Traumatic optic neuropathy was diagnosed in 14 patients (5.5%). There were 11 cases of open wounds of the globe (n = 11, 4.3%). Fifty-five percent (n = 6) of these were caused by road traffic accidents, and on VA testing, 90.9% (n = 10) and 9.1% (n = 1) had no LP (NLP) and LP, respectively. There was no case of retinal detachment. Regarding major trauma, 187 patients (73.6%) had at least one fracture at any site and 104 patients (40.9%) had brain hemorrhages. Sixty-one patients (24%) had skull fractures and 57 patients (22.4%) were hospitalized for orbital fractures classified as major systemic traumas.
Table 2
Types of ocular trauma in patients with major trauma
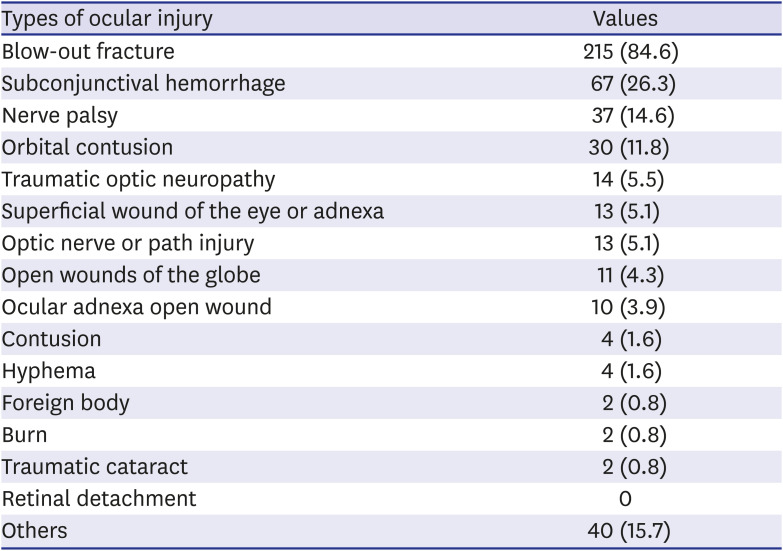
|
Types of ocular injury |
Values |
|
Blow-out fracture |
215 (84.6) |
|
Subconjunctival hemorrhage |
67 (26.3) |
|
Nerve palsy |
37 (14.6) |
|
Orbital contusion |
30 (11.8) |
|
Traumatic optic neuropathy |
14 (5.5) |
|
Superficial wound of the eye or adnexa |
13 (5.1) |
|
Optic nerve or path injury |
13 (5.1) |
|
Open wounds of the globe |
11 (4.3) |
|
Ocular adnexa open wound |
10 (3.9) |
|
Contusion |
4 (1.6) |
|
Hyphema |
4 (1.6) |
|
Foreign body |
2 (0.8) |
|
Burn |
2 (0.8) |
|
Traumatic cataract |
2 (0.8) |
|
Retinal detachment |
0 |
|
Others |
40 (15.7) |

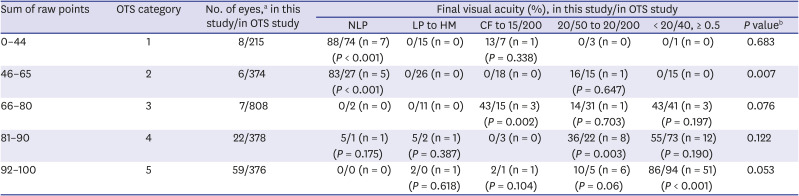
Table 3
Comparison of final visual acuities assessed with the OTS categorization with Kuhn et al.'s study7
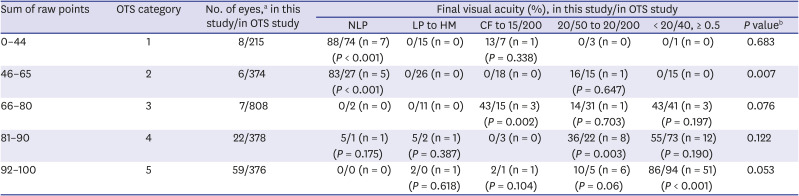
|
Sum of raw points |
OTS category |
No. of eyes,a in this study/in OTS study |
Final visual acuity (%), in this study/in OTS study |
|
NLP |
LP to HM |
CF to 15/200 |
20/50 to 20/200 |
< 20/40, ≥ 0.5 |
P valueb
|
|
0–44 |
1 |
8/215 |
88/74 (n = 7) |
0/15 (n = 0) |
13/7 (n = 1) |
0/3 (n = 0) |
0/1 (n = 0) |
0.683 |
|
(P < 0.001) |
(P = 0.338) |
|
46–65 |
2 |
6/374 |
83/27 (n = 5) |
0/26 (n = 0) |
0/18 (n = 0) |
16/15 (n = 1) |
0/15 (n = 0) |
0.007 |
|
(P < 0.001) |
(P = 0.647) |
|
66–80 |
3 |
7/808 |
0/2 (n = 0) |
0/11 (n = 0) |
43/15 (n = 3) |
14/31 (n = 1) |
43/41 (n = 3) |
0.076 |
|
(P = 0.002) |
(P = 0.703) |
(P = 0.197) |
|
81–90 |
4 |
22/378 |
5/1 (n = 1) |
5/2 (n = 1) |
0/3 (n = 0) |
36/22 (n = 8) |
55/73 (n = 12) |
0.122 |
|
(P = 0.175) |
(P = 0.387) |
(P = 0.003) |
(P = 0.190) |
|
92–100 |
5 |
59/376 |
0/0 (n = 0) |
2/0 (n = 1) |
2/1 (n = 1) |
10/5 (n = 6) |
86/94 (n = 51) |
0.053 |
|
(P = 0.618) |
(P = 0.104) |
(P = 0.06) |
(P < 0.001) |

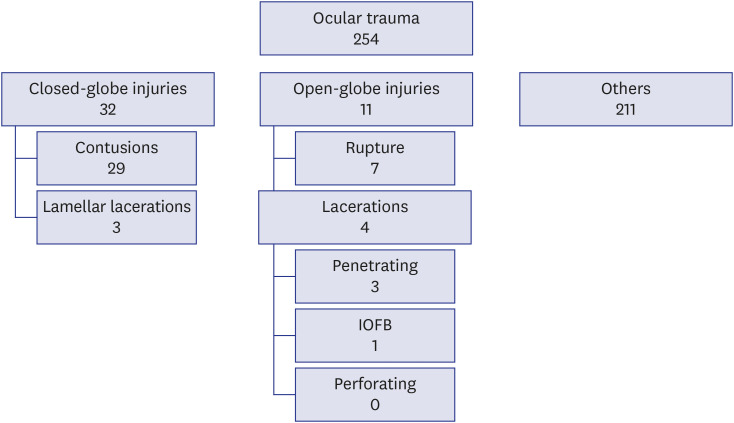
Application of BETTS, deprivation index and OTS
Fig. 2 shows 254 cases of ocular injuries that were classified using the standardized international classification of ocular trauma, termed the BETTS. Thirty-two cases were closed-globe injuries, 11 cases were open-globe injury, and 211 cases were included in ‘others.’ Among the patients with closed-globe injuries, 29 patients had contusions and 3 patients had lamellar lacerations. Regarding open-globe injuries, 7 patients had globe ruptures and 4 patients had lacerations.
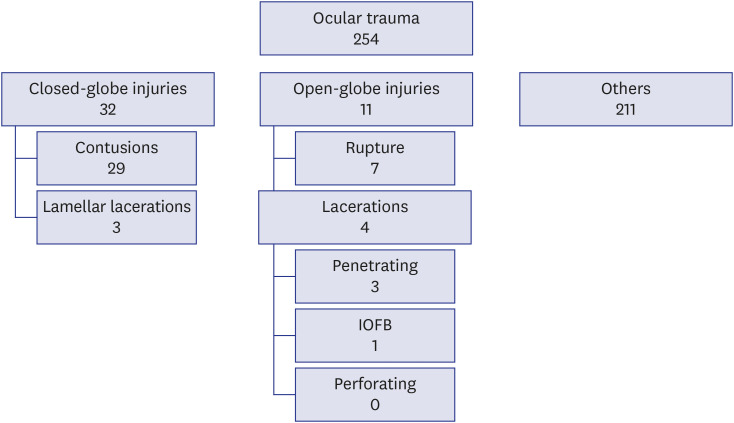 | Fig. 2
Ocular trauma associated with major trauma grouped according to the BETTS. Most of the ocular trauma patients with major trauma were not categorized into closed-globe injuries or open-globe injuries but most of them were categorized into ‘others.’
BETTS = Birmingham Eye Trauma Terminology System, IOFB = intraocular foreign body.

|
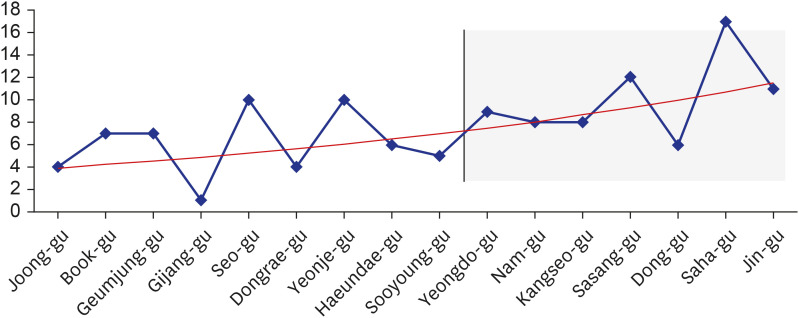
Of 125 patients; 54 patients were included in 9 non-high deprivation index areas and 71 patients were included in 7 high deprivation index areas. The distribution of ocular trauma with major trauma by residence showed a higher incidence of 56.8% in high deprivation index areas than non-high deprivation index areas in Busan (
Fig. 3). There was no correlation with the final VA (
P > 0.05,
t-test).
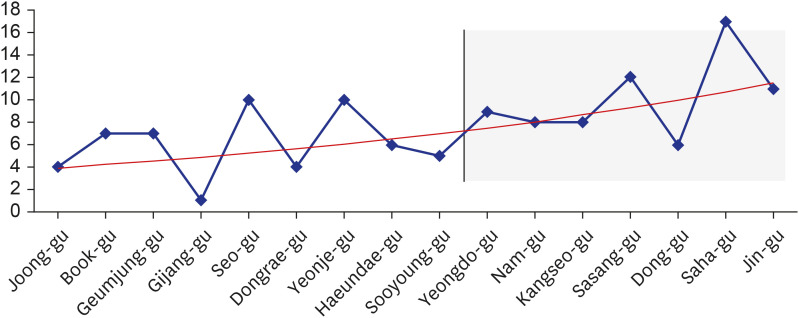 | Fig. 3Distribution by residence of ocular trauma patients with major trauma, and its association with deprivation index. Dark gray colored box indicates the upper 5% percentile deprivation index area. Despite the lack of statistical significance, it showed a tendency of increasing the number of trauma cases within area which shows the upper 5% percentile deprivation index. Black line indicates number of ocular traumas. Red line indicates exponential function of the number of ocular traumas.
|
Table 3 shows the result of comparison of the final VA assessed using the OTS categorization, reported by Kuhn et al.
7 In 254 patients, a total of 102 patients were evaluated and the rest of them could not be categorized due to lack of medical records for calculating OTS categorization. In the OTS groups 1 and 2 with low ocular trauma points, the final visual acuities were mostly restricted to NLP. Groups 4 and 5, with high ocular trauma points, had visual acuities higher than 0.4.
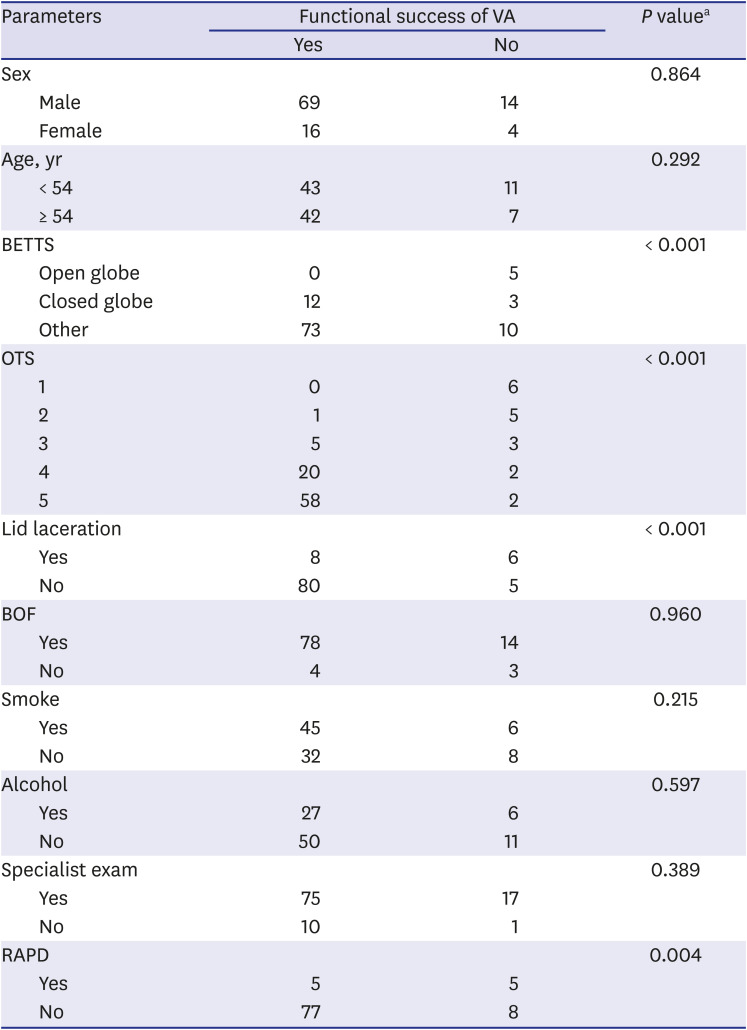
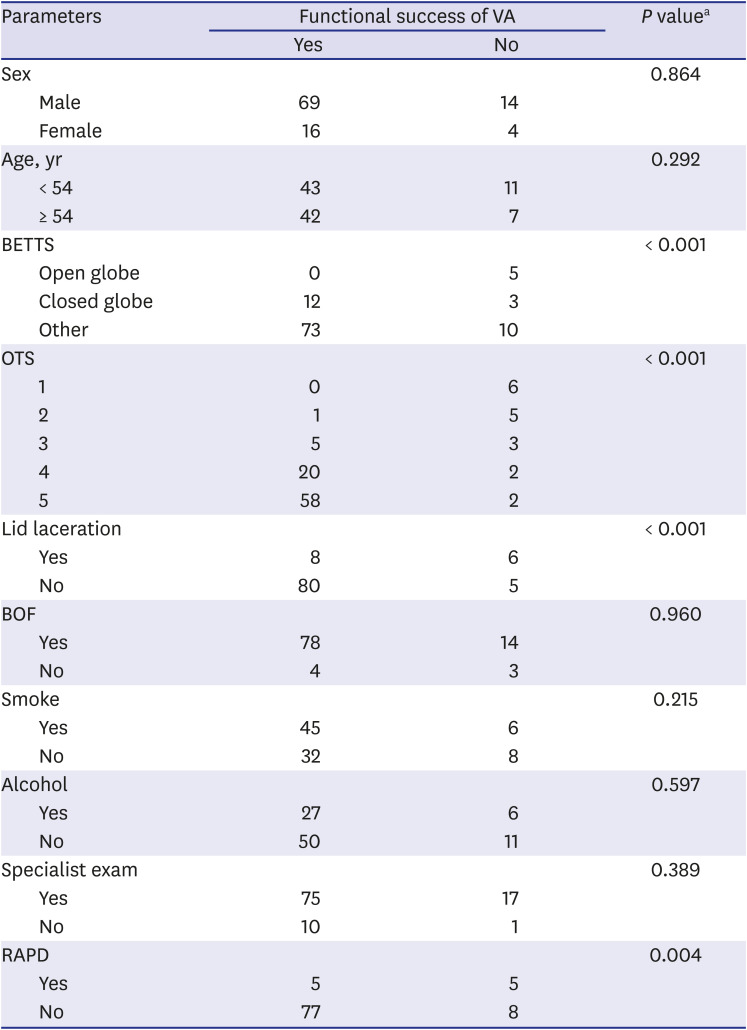
Predictive factors for final visual acuities
VA was assessed in 103 patients; 92 patients and 85 patients were vision survival and functional success, respectively. Eleven patients and 18 patients were included in no-vision survival group and no-functional success group, respectively. More details are described in
Table 4.
Table 4
Predictive factors for functional success of VA using χ2 and Fisher's exact test
|
Parameters |
Functional success of VA |
P valuea
|
|
Yes |
No |
|
Sex |
|
|
0.864 |
|
Male |
69 |
14 |
|
Female |
16 |
4 |
|
Age, yr |
|
|
0.292 |
|
< 54 |
43 |
11 |
|
≥ 54 |
42 |
7 |
|
BETTS |
|
|
< 0.001 |
|
Open globe |
0 |
5 |
|
Closed globe |
12 |
3 |
|
Other |
73 |
10 |
|
OTS |
|
|
< 0.001 |
|
1 |
0 |
6 |
|
2 |
1 |
5 |
|
3 |
5 |
3 |
|
4 |
20 |
2 |
|
5 |
58 |
2 |
|
Lid laceration |
|
|
< 0.001 |
|
Yes |
8 |
6 |
|
No |
80 |
5 |
|
BOF |
|
|
0.960 |
|
Yes |
78 |
14 |
|
No |
4 |
3 |
|
Smoke |
|
|
0.215 |
|
Yes |
45 |
6 |
|
No |
32 |
8 |
|
Alcohol |
|
|
0.597 |
|
Yes |
27 |
6 |
|
No |
50 |
11 |
|
Specialist exam |
|
|
0.389 |
|
Yes |
75 |
17 |
|
No |
10 |
1 |
|
RAPD |
|
|
0.004 |
|
Yes |
5 |
5 |
|
No |
77 |
8 |

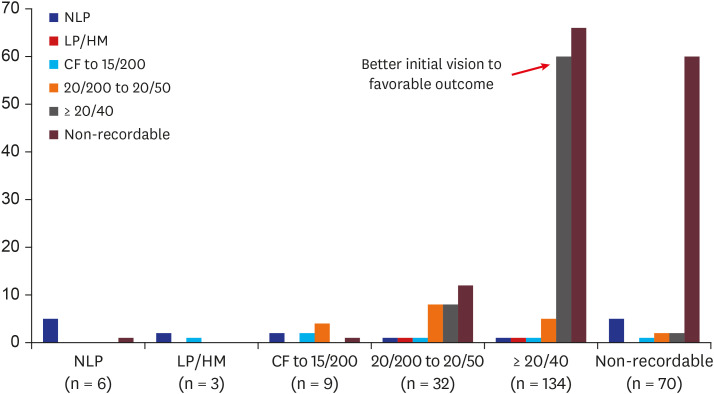
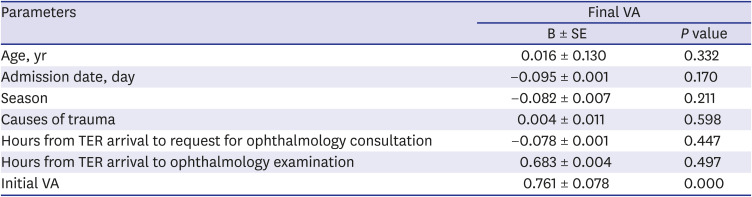
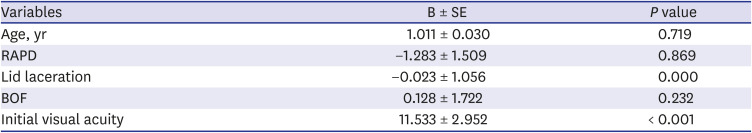
Univariate analysis for the predictive factors of visual outcomes revealed that BETTS, OTS, lid laceration, and relative afferent pupillary defect (RAPD) affected functional visual success. Old age was associated with vision survival. Linear and logistic regression analysis showed that initial VA and the presence of lid laceration were the important factors for functional visual success of final VA. The presence of lid laceration and low initial VA in trauma patients, there is a good chance to show no functional success of final VA. In terms of both vision survival and functional success, initial VA was the common important predictive factor for functional success was initial VA (
Tables 4,
5,
6). The better the initial VA, the better the final VA. The results are shown in
Fig. 4.
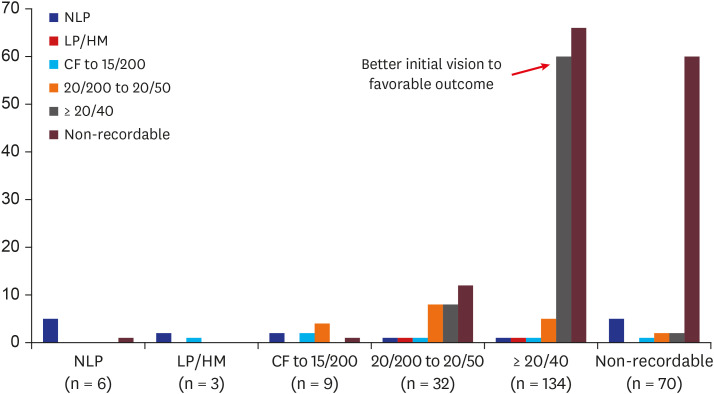 | Fig. 4
Distribution of final visual acuities according to the initial visual acuities. In univariate analysis, better initial visual acuity was found to be an important predictive factor of favorable visual outcome.
NLP = no light perception, LP = light perception, HM = hand motion, CF = count fingers.

|
Table 5
Linear regression analysis of potential predictive factors for final VA
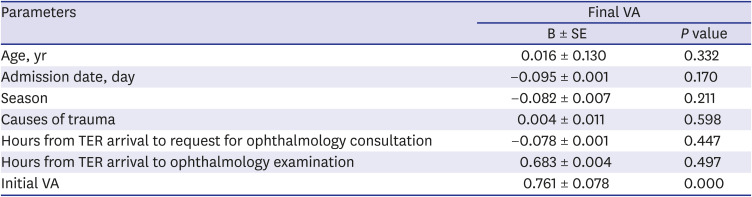
|
Parameters |
Final VA |
|
B ± SE |
P value |
|
Age, yr |
0.016 ± 0.130 |
0.332 |
|
Admission date, day |
−0.095 ± 0.001 |
0.170 |
|
Season |
−0.082 ± 0.007 |
0.211 |
|
Causes of trauma |
0.004 ± 0.011 |
0.598 |
|
Hours from TER arrival to request for ophthalmology consultation |
−0.078 ± 0.001 |
0.447 |
|
Hours from TER arrival to ophthalmology examination |
0.683 ± 0.004 |
0.497 |
|
Initial VA |
0.761 ± 0.078 |
0.000 |

Table 6
Logistic regression analysis of potential predictive factors for final visual acuity (functional success)
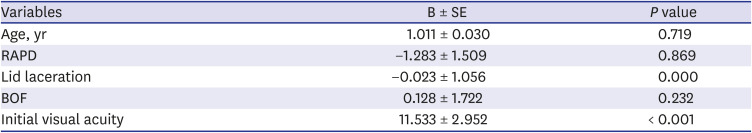
|
Variables |
B ± SE |
P value |
|
Age, yr |
1.011 ± 0.030 |
0.719 |
|
RAPD |
−1.283 ± 1.509 |
0.869 |
|
Lid laceration |
−0.023 ± 1.056 |
0.000 |
|
BOF |
0.128 ± 1.722 |
0.232 |
|
Initial visual acuity |
11.533 ± 2.952 |
< 0.001 |

Go to :

DISCUSSION
Trauma is the major cause of death in adults younger than 44 years in Korea and is considered a major public health problem. Level 1 trauma centers are institutions positioned to provide care for patients with severe trauma and can help reduce the mortality rate of preventable traumas to less than 20% by 2020.
10 Among trauma patients, ocular trauma is a major cause of morbidity and its socioeconomic impact on the younger population of working age can be significant. The incidence, subtypes, severity, risk factors, and other characteristics of ocular trauma in major trauma should be thoroughly researched to inform public health strategies and the adoption of effective interventional approaches to patients. This will reduce the socioeconomic burden on the healthcare system and the country.
11
This is the first study to examine the incidence of ocular injuries associated with major trauma at the largest level 1 trauma center in Korea and Asia. The total population of Korea is approximately 50,000,000, and the population of the Seoul, which is the capital city in Korea, is approximately 9,000,000 (18%). The population of the area covered by the level 1 trauma center of PNUH is estimated as 7,000,000 (15%). The incidence of ocular injuries associated with major trauma were 1.47/100,000, 1.57/100,000 and 1.48/100,000, while those of major trauma were 21.33/100,000, 20.94/100,000 and 20.91/100,000 in 2016, 2017 and 2018, respectively. According to previous studies on ocular trauma associated with major trauma, the incidence rate of ocular trauma associated with major trauma was within 1.49/100,000–1.57/100,000 per year. Although this is consistent with our findings, the previous studies revealed that the overall ocular trauma rate associated with major trauma has gradually decreased.
121314 In a US study, the 23.5% ocular trauma rate in 1982–88 had considerably decreased by 2.3% in 2006, mainly because of the seat belt legislation.
12 In our study, the ocular trauma rate associated with major trauma was either similar to that in the previous year or gradually increased.
There are several possible reasons for this finding. The first is the lack of awareness on ocular trauma associated with major trauma. Most of the regional trauma centers in Korea have been in operation since 2014; trauma center in PNUH was established in 2015 and is in its infancy. The main purpose of regional trauma centers is to decrease the mortality rate of preventable traumas to under 20% and help reduce the associated socioeconomic burden. Therefore, the focus of the care in trauma centers was to keep patients alive and not to maintain vision.
10 However, improvements in awareness of ocular trauma and its socioeconomic burden has resulted in increased attention and diagnoses of ocular trauma.
15 The second is by the characteristics of causes of trauma different from previous studies.
121314 The rate of falls in the aging population and pedestrian traffic accidents in an aging female population are high as well as the high rate of motorbike crashes in 10–30s male group. This is supported by our findings (
Fig. 1).
In this study, the number of male patients were 207 (81.6%), and many of them were between 50 and 60 years. According to the latest data from the National Statistical office, this is possibly related to the industrial characteristics and population distribution in Busan and the Gyeongnam Province. According to an analysis by Statistical office in 2016–2018, the proportion of people between 50 and 60 years were higher in Busan and the Gyeongnam Province than in Seoul. According to previous studies, the increase in trauma was caused by the increased rate of falls in the aging population, and approximately 82% of the increase was attributed to falls.
12131415 Another study showed that approximately 5.6% of major trauma was associated with ocular trauma and most of them were associated with road traffic accident.
12
Despite decreased trauma incidence after the seatbelt legislation, road traffic accidents are still major causes of ocular trauma in patients with major trauma (56.7% in our study).
1617 This is similar to the findings in a previous study conducted in the US, where motor vehicle crashes accounted for 52.1% of injuries.
18 This rate has decreased because of deployment of the frontal airbag, which increases the overall risk of eye injury and at the same time, reduces the number of severe eye injuries.
12 We should focus on the exorbitant number of motorbike accidents especially in male patients aged between 20 and 30 years. Guly et al.
12 reported that the significant decrease in ocular injuries associated with major trauma in the United States, from 13.5% in 1982–88 to 2.3% in 2006, was associated with the enforcement of the seat belt legislation. Similarly, in our study, the proportion of the ‘in-car traffic accidents’ was low but the proportion of motorbike accidents, which is less affected by the legislation, was significantly high. This is a problem related to the citizenship and the society, as well as the government, which must be attended to.
In a study conducted in Montreal in 2016, Ross et al.
19 reported that 73 patients underwent consultation for orbital fractures in a level 1 trauma center for over a year. This is similar to our findings; the number of patients with orbital fracture in our level 1 trauma center is around 70 patients per year. In contrast, Korea reported approximately 16.2%–19.2%, as a small proportion of ocular trauma patients were diagnosed with orbital fractures in comparison to our study that revealed approximately 84.6% of ocular trauma associated with major trauma cases to be orbital fractures. The higher proportion of orbital fractures in our study compared to the other study on eye trauma in Korea is mainly attributable to the difference in the analysis groups. The previous studies in Korea analyzed all the patients referred from the emergency room, while our study analyzed patients with major trauma who were referred to the ophthalmology department from the trauma center. In our study, only 26.5% of cases were isolated orbital fractures, and more than half of the patients with orbital fractures had multiple or complex facial fractures, as well as multiple trauma such as brain hemorrhages and skull fractures. Similar to previous studies, orbital fractures could be associated with serious complications, such as globe rupture or traumatic optic neuropathy, but orbital fracture itself was not significantly associated with the final VA and functional visual success.
1920 Based on our practice, and unlike in past studies,
2122 patients with only orbital fractures, even if associated with major trauma, who do not have visual symptoms do not require emergent evaluation. We may propose some benefit in delaying treatment of orbital fractures after full trauma evaluation.
Recently, some authors have reported that a lower education level is an independent determinant of ocular trauma.
23 This may be attributed to the fact that lower education is associated with a lack of awareness of the necessary safety and precautionary measures, and risk-taking. This increases the risk of various types of trauma including ocular trauma.
2324 In the same context, Choi et al.
8 reported on the deprivation index and mortality rate in Busan, and revealed that more deprived towns were likely to have higher mortality, particularly from physical injury. The results analyzing the relationship between the ocular trauma and this index did not show any significant correlation including final VA (
P > 0.05,
t-test). However, the results show a higher occurrence rate of ocular trauma (56.8%) in high deprivation index area which indicates upper 5% percentile deprivation. Regarding this result, more efforts are needed for analysis, with assistance from the government and the community.
We found that BETTS and OTS were good predictors of final VA. However, Ahmad et al.
25 in 2016, reported that 70% of all ocular traumas could not be categorized by BETTS, as the classification does not include superficial eye, adnexal lid, lacrimal, or orbital injuries. Similarly, 83.1% of ocular trauma with major trauma in this study could not be categorized by BETTS. There are some limitations of BETTS classification itself to classify all ocular trauma types, and some shortage of documented objective terminology and evaluation of ocular trauma patients were the inevitable problem that cannot be ignored. Ahmad et al.
25 attempted to use the modified BETTS classification, but as the main focus area of BETTS is the eyeball, and there is a major limitation in applying it to all ocular traumas associated with major traumas. OTS is also a standardized categorical system for prediction of visual prognosis, which was first introduced by Kuhn et al.
7 in 2002. Several studies assessing ocular trauma using OTS have been well described in literature.
262728 OTS is a good predictive scoring system to evaluate ocular trauma and studies using this system have shown comparable results with those of the OTS study by Kuhn et al.
7 In our study, the results that final VA evaluated using OTS categories were good predictors but still 37.1% of patients could not be categorized by OTS. The initial reason is that the sclera and cornea are the main factors assessed in BETTS. OTS factors, on the other hand, are initial vision, presence of globe rupture, endophthalmitis, perforating injury, retinal detachment, and RAPD. These factors are all focused on the eyeball and its related problems. Therefore, it could be ineffective for patients who only have periocular trauma, facial or orbital fractures, and lacerations, foreign bodies, contusions on eyelid, lacrimal duct, or periorbital regions. The second reason is that there is a lack of medical records with appropriate terms for application to OTS. Overall, BETTS and OTS are both excellent assessment tools to predict the final VA, but more comprehensive eye trauma assessment tools covering the eyeball, orbital, and periorbital trauma are necessary, while considering cases of extensive and systemic trauma referred to the level 1 trauma center. Additional analysis is ongoing for the development of an assessment tool for ocular trauma associated with major trauma, which comprehensively covers the factors of trauma, including the presence of an ocular trauma specialist.
Univariate analysis revealed that age, BETTS, OTS, Lid laceration and RAPD were significantly related to the final VA. Logistic and linear regression analysis revealed that initial VA was the most significant predictive factor of final VA in trauma patients. This has been established in previous studies,
272930 and measurement of VA is mandatory. Lid laceration was also significantly related to the final VA. This may be a key sign for trauma specialists who are not ophthalmologists to observe. The first medical personnel who evaluates a trauma patient is usually not an ophthalmologist. Staff should be aware of lid laceration as an important sign for poor final VA and request ophthalmological treatment promptly.
From this study, more objective terminology must be applied to ocular trauma patients and effort is needed to evaluate OTS and BETTS system to arrive at an appropriate treatment strategy and reduce clinical and socioeconomic burden caused by trauma. The important thing is that a more effective evaluation system should also be established for ocular trauma globally. This study reports on the epidemiology of ocular trauma in patients with major trauma. Our findings would facilitate better evaluation strategies for ocular trauma patients with major trauma in Korea. We also believe that the perceptions about trauma centers and eye trauma in the Busan area will change. These findings may also provide the substrate for investments and development of the medical system for the care of trauma patients. In a future study, we will endeavor to develop an eye trauma evaluation index that can be used at a level 1 trauma center for patients with major trauma.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download