RESULTS
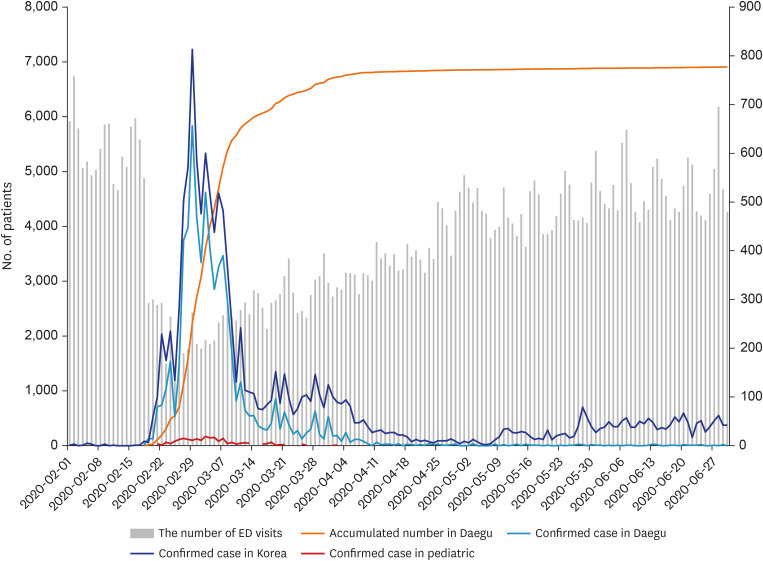
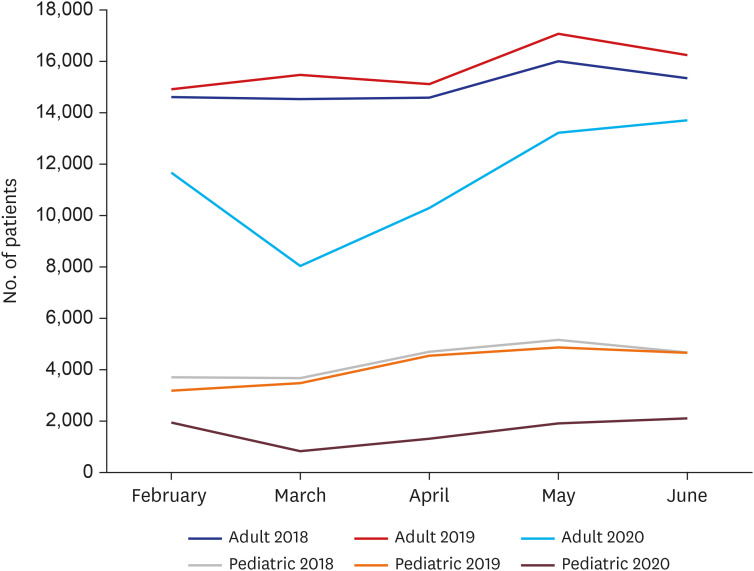
A total of 65,017 patients visited the six EDs during the COVID-19 outbreak in 2020; this number was markedly less than that from the years 2018 (96,983) and 2019 (99,529) (
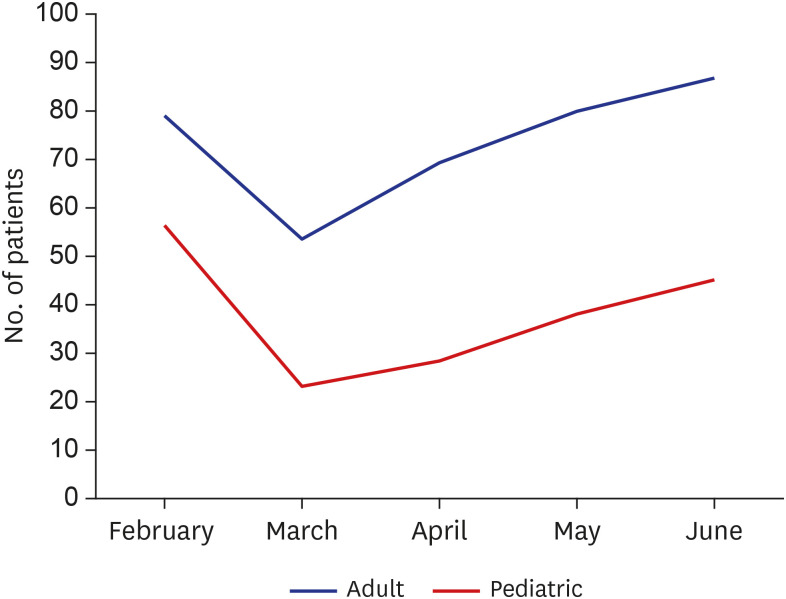
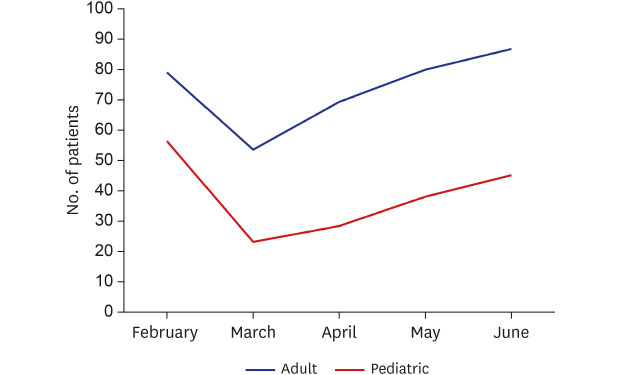
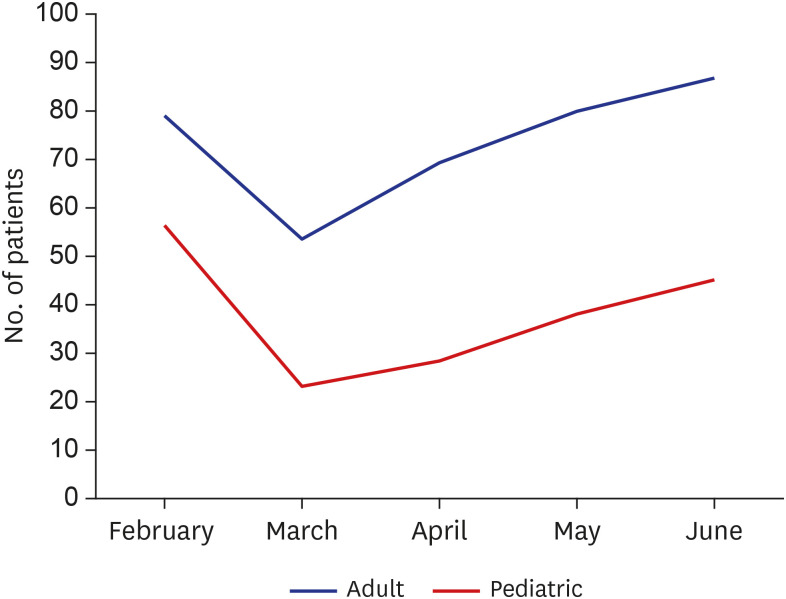
Fig. 1). While adult patients' visits decreased by 26.0% compared with that in 2018 and 2019, pediatric patients' visits decreased remarkably by 62.0%. In March 2020, when the outbreak was at its peak, the mean numbers of adult and child patients were lower than that of the two preceding years by 46.4% and 76.9%, respectively. The number of patients gradually increased over the months until June 2020. While the number of adult patients was 86.8% of that in the two preceding years, the number of pediatric patients was barely 45.2% (
Fig. 2). Furthermore, pediatric patients accounted for 21.7% of the total ED presentations in 2018 and 2019, whereas they only accounted for 12.5% in 2020.
Fig. 1
Number of adult and pediatric emergency department visits per month from 2018 to 2020.
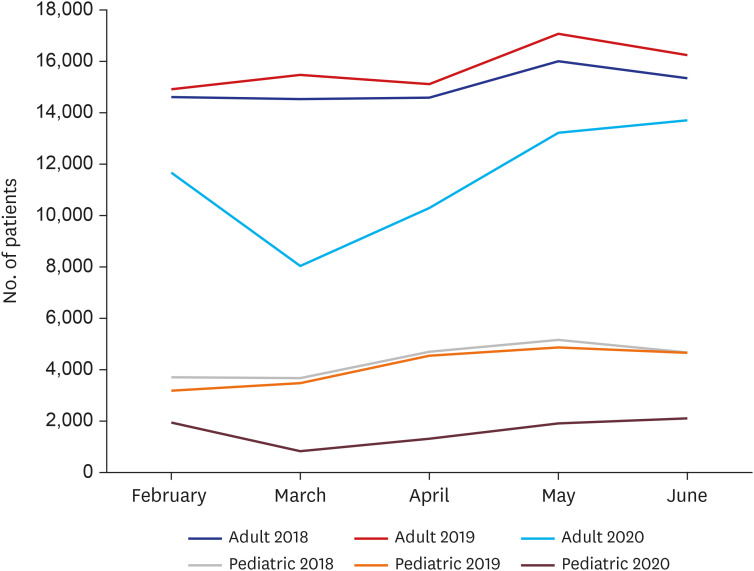

Fig. 2
Percentages of adult and pediatric emergency department visits compared with those in the previous two years.

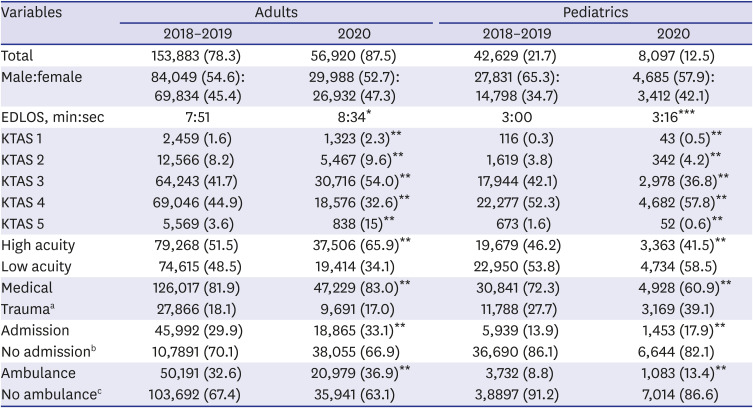
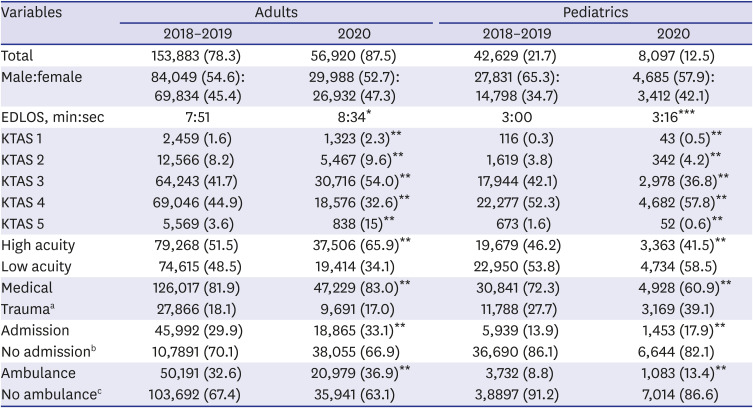
Compared with that of the two preceding years, the LOS in the EDs increased by 43 minutes for adults and 16 minutes for children in 2020. Regarding KTAS, compared with that in 2018 and 2019, the proportion of adults presenting with high acuity increased by 14.4%, whereas that of children decreased by 4.7% in 2020. Furthermore, the number of adults who visited the EDs because of a disease increased by 1.1%, whereas that of children decreased 11.4% in 2020 compared with those in 2018 and 2019. The percentage of adults and children who were hospitalized after an ED visit in 2020 increased by 3.2% and 4.0%, respectively, compared with those in the preceding years. The mean ED LOS of hospitalized pediatric patients increased from 341.8 minutes in 2018/2019 to 394.7 minutes in 2020. Regarding transportation means to EDs, the use of an ambulance in 2020 increased by 4.3% and 4.6% among adults and children, respectively, compared with those in 2018 and 2019 (
Table 1).
Table 1
The number of emergency department patients in 2018–2019 compared to those in 2020
|
Variables |
Adults |
Pediatrics |
|
2018–2019 |
2020 |
2018–2019 |
2020 |
|
Total |
153,883 (78.3) |
56,920 (87.5) |
42,629 (21.7) |
8,097 (12.5) |
|
Male:female |
84,049 (54.6):69,834 (45.4) |
29,988 (52.7):26,932 (47.3) |
27,831 (65.3):14,798 (34.7) |
4,685 (57.9):3,412 (42.1) |
|
EDLOS, min:sec |
7:51 |
8:34*
|
3:00 |
3:16***
|
|
KTAS 1 |
2,459 (1.6) |
1,323 (2.3)**
|
116 (0.3) |
43 (0.5)**
|
|
KTAS 2 |
12,566 (8.2) |
5,467 (9.6)**
|
1,619 (3.8) |
342 (4.2)**
|
|
KTAS 3 |
64,243 (41.7) |
30,716 (54.0)**
|
17,944 (42.1) |
2,978 (36.8)**
|
|
KTAS 4 |
69,046 (44.9) |
18,576 (32.6)**
|
22,277 (52.3) |
4,682 (57.8)**
|
|
KTAS 5 |
5,569 (3.6) |
838 (15)**
|
673 (1.6) |
52 (0.6)**
|
|
High acuity |
79,268 (51.5) |
37,506 (65.9)**
|
19,679 (46.2) |
3,363 (41.5)**
|
|
Low acuity |
74,615 (48.5) |
19,414 (34.1) |
22,950 (53.8) |
4,734 (58.5) |
|
Medical |
126,017 (81.9) |
47,229 (83.0)**
|
30,841 (72.3) |
4,928 (60.9)**
|
|
Traumaa
|
27,866 (18.1) |
9,691 (17.0) |
11,788 (27.7) |
3,169 (39.1) |
|
Admission |
45,992 (29.9) |
18,865 (33.1)**
|
5,939 (13.9) |
1,453 (17.9)**
|
|
No admissionb
|
10,7891 (70.1) |
38,055 (66.9) |
36,690 (86.1) |
6,644 (82.1) |
|
Ambulance |
50,191 (32.6) |
20,979 (36.9)**
|
3,732 (8.8) |
1,083 (13.4)**
|
|
No ambulancec
|
103,692 (67.4) |
35,941 (63.1) |
3,8897 (91.2) |
7,014 (86.6) |

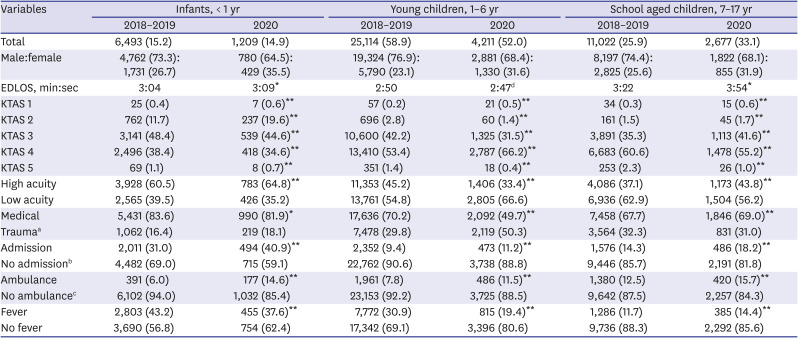
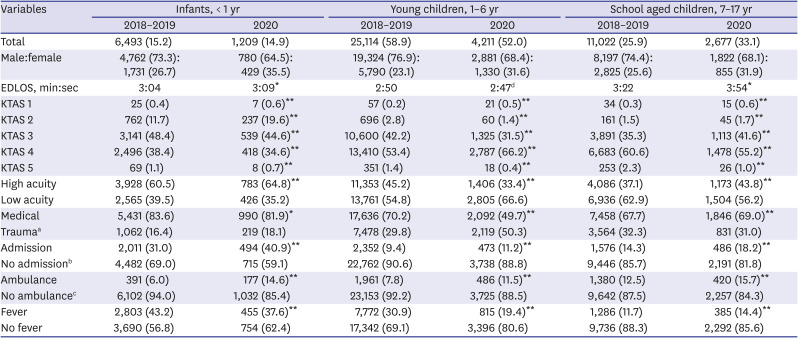
Children were categorized as infants, young children, and school-aged children to analyze and compare the parameters with those for the two preceding years. In 2020, the percentage of infants and young children presenting to EDs decreased by 0.3% and 6.9%, respectively, and increased by 7.2% among school-aged children compared with those in 2018 and 2019. Moreover, the LOS in the EDs in 2020 increased by 5 minutes and 32 minutes for infants and school-aged children, respectively, and decreased by 3 minutes for young children compared with those in 2018 and 2019. Regarding KTAS, in 2020, the number of patients with high acuity increased by 4.3% and 6.7% among infants and school-aged children, respectively, and decreased by 11.8% among young children compared with those in 2018 and 2019. Regarding the reason for ED visit, in 2020, the number of patients who visited because of a disease decreased by 1.7% and 20.5% among infants and young children, respectively, and increased by 1.3% among school-aged children compared with those in the preceding years. The percentage of patients hospitalized after ED presentation in 2020 increased by 9.9%, 1.8%, and 3.9% among infants, young children, and school-aged children, respectively, compared with those in 2018 and 2019. Regarding transportation means to EDs, ambulance use in 2020 increased by 8.6%, 3.7%, and 3.2% in among infants, young children, and school-aged children, respectively, compared with those in 2018 and 2019. Finally, the number of patients presenting with fever in 2020, the most common chief complaint among children, changed by -5.6%, -11.5%, and +2.7% among infants, young children, and school-aged children, respectively, compared with those in the preceding years (
Table 2).
Table 2
The number of pediatrics emergency department patients in 2018–2019 compared to those in 2020
|
Variables |
Infants, < 1 yr |
Young children, 1–6 yr |
School aged children, 7–17 yr |
|
2018–2019 |
2020 |
2018–2019 |
2020 |
2018–2019 |
2020 |
|
Total |
6,493 (15.2) |
1,209 (14.9) |
25,114 (58.9) |
4,211 (52.0) |
11,022 (25.9) |
2,677 (33.1) |
|
Male:female |
4,762 (73.3):1,731 (26.7) |
780 (64.5):429 (35.5) |
19,324 (76.9):5,790 (23.1) |
2,881 (68.4):1,330 (31.6) |
8,197 (74.4):2,825 (25.6) |
1,822 (68.1):855 (31.9) |
|
EDLOS, min:sec |
3:04 |
3:09*
|
2:50 |
2:47d
|
3:22 |
3:54*
|
|
KTAS 1 |
25 (0.4) |
7 (0.6)**
|
57 (0.2) |
21 (0.5)**
|
34 (0.3) |
15 (0.6)**
|
|
KTAS 2 |
762 (11.7) |
237 (19.6)**
|
696 (2.8) |
60 (1.4)**
|
161 (1.5) |
45 (1.7)**
|
|
KTAS 3 |
3,141 (48.4) |
539 (44.6)**
|
10,600 (42.2) |
1,325 (31.5)**
|
3,891 (35.3) |
1,113 (41.6)**
|
|
KTAS 4 |
2,496 (38.4) |
418 (34.6)**
|
13,410 (53.4) |
2,787 (66.2)**
|
6,683 (60.6) |
1,478 (55.2)**
|
|
KTAS 5 |
69 (1.1) |
8 (0.7)**
|
351 (1.4) |
18 (0.4)**
|
253 (2.3) |
26 (1.0)**
|
|
High acuity |
3,928 (60.5) |
783 (64.8)**
|
11,353 (45.2) |
1,406 (33.4)**
|
4,086 (37.1) |
1,173 (43.8)**
|
|
Low acuity |
2,565 (39.5) |
426 (35.2) |
13,761 (54.8) |
2,805 (66.6) |
6,936 (62.9) |
1,504 (56.2) |
|
Medical |
5,431 (83.6) |
990 (81.9)*
|
17,636 (70.2) |
2,092 (49.7)**
|
7,458 (67.7) |
1,846 (69.0)**
|
|
Traumaa
|
1,062 (16.4) |
219 (18.1) |
7,478 (29.8) |
2,119 (50.3) |
3,564 (32.3) |
831 (31.0) |
|
Admission |
2,011 (31.0) |
494 (40.9)**
|
2,352 (9.4) |
473 (11.2)**
|
1,576 (14.3) |
486 (18.2)**
|
|
No admissionb
|
4,482 (69.0) |
715 (59.1) |
22,762 (90.6) |
3,738 (88.8) |
9,446 (85.7) |
2,191 (81.8) |
|
Ambulance |
391 (6.0) |
177 (14.6)**
|
1,961 (7.8) |
486 (11.5)**
|
1,380 (12.5) |
420 (15.7)**
|
|
No ambulancec
|
6,102 (94.0) |
1,032 (85.4) |
23,153 (92.2) |
3,725 (88.5) |
9,642 (87.5) |
2,257 (84.3) |
|
Fever |
2,803 (43.2) |
455 (37.6)**
|
7,772 (30.9) |
815 (19.4)**
|
1,286 (11.7) |
385 (14.4)**
|
|
No fever |
3,690 (56.8) |
754 (62.4) |
17,342 (69.1) |
3,396 (80.6) |
9,736 (88.3) |
2,292 (85.6) |

During the study, a total of 6,906 confirmed COVID-19 patients were identified in Daegu, Korea, of which 254 (3.7%) were pediatric patients. In the pediatric patient group, male patients comprised 50.4% (128/254) of the total, and the majority (82.3%, 209/254) were school-aged children.
DISCUSSION
To the best of our knowledge, this is the first study to compare changes between the utilization of EDs during the pandemic and that during the same period in the two preceding years in Daegu, a region that underwent an explosive outbreak of COVID-19. In our study, although the number of ED visits reduced for both children and adults, a greater reduction was observed among the former. During 2020, the number of patients visiting the ED increased; however, the rate of increase was lower among children than that among adults. The proportion of patients with severe conditions increased in adults, infants, and school-aged children, and consequently resulted in increased ambulance use and higher hospitalization rates. Although the number of febrile infants and young children decreased, more school-aged children visited the ED with febrile illnesses. During the study, 3.7% (254/6,906) of all patients were pediatric COVID-19 patients; no deaths were reported among them.
Since the first confirmed case in Korea on January 20, 2020, COVID-19 spread relatively slowly in the country until the first case in Daegu on February 18th, 2020, after which an explosive outbreak occurred with massive transmission of infection, primarily in the Daegu region. As of March 14, 2020, the number of confirmed cases in Daegu City, including the nearby Gyeongbuk region, accounted for 88.3% of the entire COVID-19 patient population in Korea. Having become a major epidemic area in Korea, Daegu was designated as a special disaster region.
From the onset of the pandemic, the Korean government and media emphasized the importance of social distancing and personal hygiene, including facial mask usage and handwashing, to prevent the spread of infection; based on the most recent experience with the MERS outbreak. To prevent the spread of the infection within hospitals, those with fever or respiratory symptoms have been requested to call the Korea Centers for Disease Control and Prevention (KCDC) or the local public health center for further instructions. Hospitals have also banned visits from family and friends and postponed scheduled surgeries, if feasible. Contactless outpatient care over the phone was temporarily permitted. The Koreans also avoided hospital visits in fear of possible infection transmission. Therefore, the number of visits to all healthcare facilities, from local clinics to tertiary referral hospitals, decreased substantially.
The observed change in ED utilization can be explained in several different ways. For example, ED utilization may vary according to disease features, such as infectivity and mortality rate. They may also vary according to the source of infection as observed in the SARS epidemic in 2003, H1N1 influenza pandemic in 2009, and MERS outbreak in 2015.The number of ED visits decreased during the SARS epidemic due to the fear of nosocomial transmission, but increased during the H1N1 pandemic due to the fear of the disease itself and its low case fatality rate. During the MERS epidemic, the number of ED visits declined due to the high nosocomial transmission rate and high mortality despite the low number of patients affected.
567
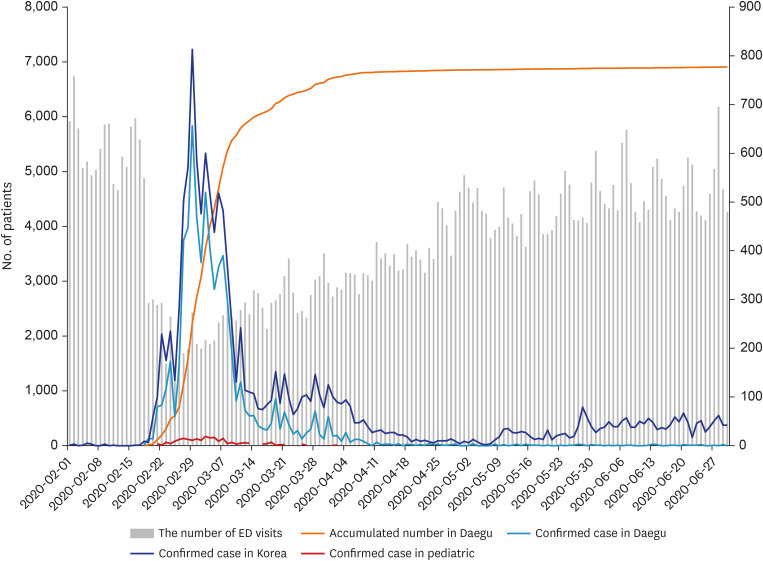
Contrastingly, changes in the number of ED visits in the present study were closely but inversely related to the increase in the confirmed cases (
Fig. 3). The number of ED visits declined rapidly with the first confirmed case in Korea in February 2020, and by March 2020, when the spread of the infection had peaked in the country, the percentages of ED visits were 53.6% and 23.2% compared with that in the preceding years (2018, 2019) among adults and children, respectively. Recent studies revealed a consistent pattern globally, with 30%–88% reduction in pediatric ED presentations, during the pandemic.
10111213 Such dramatic decline in pediatric presentations could have been influenced by an interaction of biological, psychological, and social factors, as summarized below.
Fig. 3
Total number of confirmed cases in Korea and Daegu and numbers of ED visits.
ED = emergency department.

First, reinforcement of personal hygiene practices, prohibition of physical school attendance, and revision of the academic schedule by the Ministry of Education (including school closure, reopening with virtual instruction, and implementation of attendance on alternate days) noticeably impacted children. Owing to personal hygiene prevention practices and isolation of infected or exposed individuals, the incidence of acute infection and hospital visits decreased. Thus, pediatric patients, who are most often more susceptible to acute infections, were most influenced. This is because, despite the slightly earlier onset of the influenza outbreak in Korea compared with the COVID-19 outbreak, the spread of influenza was virtually halted,
14 unlike in previous years. In this study, pediatric patients comprised a smaller proportion of all ED patients in 2020 than in 2018/2019. Moreover, fewer infants and young children and more school-aged children presented to the ED with fever as the chief complaint in 2020 than in the previous years. Despite the extension of the winter break and postponement of school reopening, the anxiety about COVID-19 might have caused the increase in the number of ED presentations by school-aged children. This is possibly because school-aged children were the most affected (82.3%) among all the children with confirmed COVID-19 in this study. Thus, those who would have normally been administered antipyretics and who would have stayed at home possibly presented to the ED at the slightest evidence of symptoms of COVID-19 following screening. After attendance on alternate days, schools also required students who developed symptoms to undergo screening, thereby leading to an increase in ED presentations.
Second, ED presentations could also have declined due to the fear of nosocomial transmission, possibly due to previous spread of MERS in EDs in Korea in June 2015. In that incident, one infected patient had transmitted the infection to 78 other people at the hospital, including healthcare providers. Overall, 186 MERS cases were confirmed in Korea (mortality rate, 20%).
615 Moreover, the media report of closure of some hospital EDs due to ED visits by patients with COVID-19 could have further increased the avoidance of ED visits.
16 The fear of nosocomial transmission also led primary clinics to practice restrictive care, which further diminished patients' access to health care facilities. Due to the prolonged COVID-19 pandemic, resources were depleted in most hospitals; hence, they were unable to attend to patients with fever or respiratory symptoms. This might have increased the ambulance use for adults and children by 4.3% and 4.6%, respectively, compared with that in 2018 and 2019. Reduced access to healthcare facilities in fear of nosocomial transmission may also cause reduced routine hospital visits, thereby reducing the number of routine examinations.
1217 A previous study suggested greater consequences for pediatric patients due to the fear of COVID-19 that results in delayed access to care, and called for “high-quality coordinated care.”
1018
Third, EDs are unable to accept a large number of patients. Furthermore, hospitals limited the number of admissions and transfer of patients who were not in need of emergency care. While the number of patients declined, the LOS in the ED increased for both adults and children in this study. Despite the simplification of all procedures to minimize ED LOS, the use of restricted isolation rooms and COVID-19 screening results were time consuming. In addition, the space between hospital beds was increased and the number of available beds was decreased to prevent potential spread of infection among the patients. Of the six hospitals, four reported an increase in LOS whereas two reported a decrease. In the latter, patients who needed hospitalization were quarantined in a single room even before the COVID-19 screening result was confirmed. In all six hospitals, there was no reported nosocomial infection by pediatric patients admitted from the ED.
Fourth, Korea's implementation of the National Health Insurance Service (NHIS) does not impose limitations to healthcare facilities that patients may visit. Therefore, non-emergency patients have contributed to the crowding of EDs in tertiary hospitals. The reduction of non-urgent patients seeking medical care due to simple infections was similar to that observed during the MERS epidemic.
6 A recent study also reported that the reduction in non-emergency pediatric patients during the COVID-19 pandemic is closely related to ED crowding.
19 Despite the introduction of various measures to relieve the situation, several studies revealed that EDs remain crowded.
202122 ED overcrowding increases mortality,
232425 delays timely treatment,
26 facilitates the spread of infection within the hospital,
27 and diminishes physicians' job satisfaction.
28 In particular, children often present with problems that can be addressed in units other than the ED. Continuous policy support and development are needed such that non-urgent, low-acuity patients can seek medical care in primary clinics to foster an ED environment that allows healthcare providers to focus on patients with urgent conditions.
In the present study, the proportion of pediatric patients with low acuity KTAS level increased. This may be related to the increase in the proportion of young children group with low acuity levels, which accounts for the largest proportion of pediatric patients. In this group, the proportion of patients with low acuity level increased while the overall number of patients decreased. Specifically, the proportion of trauma patients with low acuity level decreased by 3.9% while that of medical patients increased by 5.3%. Therefore, the increase in low acuity levels in young children may be associated with the increase among medical patients. Additionally, the proportion of trauma patients in this group markedly increased by 20.5%. Higher trauma rates were reported in young children than those in other age groups. Children in this age group had a higher rate of falls and safety accidents possibly because of an inability to control posture or judge a situation. In addition, external activities decreased due to COVID-19; thereby increasing the amount of time spent at home where child safety accidents occur most frequently. Moreover, as observed during the MERS epidemic, ED presentations of trauma patient aged 1–6 years increased because they could not be appropriately treated in primary medical institutions.
29
This study has a few limitations. First, six EDs in the Daegu region are not representative of all EDs in Korea, and the reported changes in ED utilization are not representative of the entire healthcare utilization changes due to COVID-19. Furthermore, limitations exist with the retrospective analysis of medical records, and examining changes during a short study period in the early days of the pandemic may not represent the overall changes in ED utilization. In addition, due to the limitations of KTAS, which only scores patients based on the major symptoms and vital signs at the time of the presentation, underlying diseases or features of diseases that are not manifested during the incubation period may not be accurately reflected. Analyzing the nationwide ED usage patterns and changes in primary clinic visits using the NEDIS and NHIS data during the entire COVID-19 pandemic period would provide a more accurate understanding of the pediatric patients' healthcare utilization patterns in relation to COVID-19.
The COVID-19 pandemic has highlighted the need for EDs to more promptly maintain flexible and effective operations, worldwide. It is important to predict any changes in patterns of patient ED visits and establish guidelines, to actively respond to the pandemic situation.
30 At the current rate, EDs will not be crowded with non-urgent pediatric patients who have simple infections, as it did before the COVID-19 pandemic. When or if the COVID-19 pandemic ends and the students resume school after a long break, we hope that the children seek prompt medical care for the timely identification of diseases during their treatment windows.
In conclusion, COVID-19 has brought about many changes to ED utilization. A greater reduction of ED utilization occurred in pediatric patients than in adult patients, and the rate of increase in the number of patients presenting to the ED over time was lower among children. The proportion of patients with severe conditions increased in adults, infants, and school-aged children, and consequently resulted in increased ambulance use and higher hospitalization rates. Although fewer febrile infants and young children presented to the ED, more school-aged children visited the ED with febrile illnesses. In the event of an infectious disease outbreak, measures to predict ED utilization by the healthcare system and ensure changes in ED utilization to provide the most efficient health care are essential.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download