INTRODUCTION
In 1999, the Internal Organ, etc. Transplant Act (which is equivalent to the Organ Transplantation Act [OTA])
1 was enacted in Korea, legalizing organ transplantation from brain-dead donors. After passage of this act, the Korean government increased its efforts to locate brain-dead donors for organ procurement. As a result, the number of brain-dead donors steadily increased between 2002 and 2016 from 36 to 573 (from per million population [pmp], 0.74 to 11.28).
2 However, this number decreased to 515 (pmp, 10.01) in 2017 and 449 (pmp, 8.70) in 2018.
3 Considering the huge disparity between organ donation and organ demand, this decline is a serious problem. Therefore, it is necessary to examine the reasons for and seek to reverse the downward trend.
Currently, the organ donation and transplantation system in Korea is structured as follows. Korean Network for Organ Sharing (KONOS) evaluates the eligibility of living donors and allocates procured organs to the recipients, while Korea Organ Donation Agency (KODA) and Hospital-based Organ Procurement Organizations (HOPOs)—hospitals designated as special institutions for management of suspected brain-dead patients—carry out organ procurement.
4 There are 47 KODA-contracted hospitals and 36 HOPOs in the country.
3 In HOPOs, the process of brain-dead organ donation is carried out after brain-dead patients have been identified, whereas KODA engages in the organ donation process after it has been notified of brain-dead individuals by contracted hospitals. The revised version of OTA was enacted in 2010, giving a legal basis for organ procurement organizations and introducing a system that mandates reporting of suspected brain-dead patients.
56 As the number of reported potential brain-dead patients increased, the number of brain-dead donors jumped from 268 (pmp, 5.31) in 2010 to 368 (pmp, 7.25) in 2011.
3 When a suspected brain-dead patient is reported to KODA, an organ procurement coordinator is dispatched immediately to coordinate the process of organ donation and transplantation. The coordinator assists evaluation of brain death, management of brain-dead donors, harvest of organs and tissues, as well as management of the cadaver and the bereaved family.
4 Consent of the patient's family is essential in carrying out this process. Korea utilizes a modified version of a broad opt-in system through which families make decisions regarding organ donation.
7 When the brain-dead patient has not provided explicit objection, organ donation can occur with consent from family members. However, even if the patient has explicitly stated the intention to donate their organs, donation cannot take place if family members object.
78 At the same time, determination of brain death cannot occur when a family objects to donation, because brain death evaluation is provided only for the purpose of organ donation.
1
In Korea, legal death usually means cessation of the heart. However, a brain-dead patient can be recognized as legally dead, but only when diagnosed with brain death for the purpose of organ donation.
1 To be diagnosed with brain death, the patient's family must consent to the evaluation process for purposes of possible organ donation. If the patient qualifies as brain dead and the family consents to donation, then the patient is recognized as legally dead at the moment the committee diagnoses brain death. Accordingly, potential brain-dead patients who do not proceed to the evaluation process are not recognized as legally dead.
Before enactment of the “Act on Decisions on Life-Sustaining Treatment for Patients in Hospice and Palliative Care or at the End of Life,”
9 hereafter the Life-Sustaining Treatment Act, it was unclear whether life-sustaining treatment could be withheld or withdrawn from any patient regardless of brain function. Therefore, an issue had long existed in Korea whether life-sustaining treatment should continue for potentially brain-dead patients. In particular, it was unclear whether it was legal to withdraw life-sustaining treatment and accelerate death for potential brain-dead patients.
10 Moreover, as legal determination of brain death could only be performed for the purpose of organ donation,
1 the only permissible way to forgo life-sustaining treatment of suspected brain-dead patients was through the process of brain-dead organ donation.
This situation changed in 2017 with implementation of the Life-Sustaining Treatment Act. This Act provides a legal procedure whereby patients at the end of life are allowed to forgo life-sustaining treatment, either through legal documents stating patient intentions, through a patient's inferred intention supported by the family, or through unanimous agreement among the family members. Brain-dead patients who are expected to die within days or weeks fall under the Act's category of patients in the end-of-life process and therefore are allowed to legally forgo life-sustaining treatment. The Act, the part on end-of-life and life-sustaining treatment, took effect in certain hospitals in October 2017
11 and became effective throughout Korea in February 2018.
9 Thereafter, families of potentially brain-dead patients were provided a legal process that allowed them to forgo life-sustaining treatment without being declared brain dead and an organ donor.
Efforts have been made to identify reasons for the decline in organ donation since 2017. A recent study identified aspects of the management process for brain-dead potential organ donors that impeded donation.
12 Meanwhile, another study by Cho
13 identified several possible reasons behind the decrease: a decline in occurrence of certain medical conditions that lead to brain death; a reduced consent rate in patient families due to media reports on inappropriate care of organ donor remains; reduced reporting of potential brain death from large hospitals; the aging population, an increase in mean age of organ donors, and hospital reluctance to manage elderly donors; a labor shortage for donor processing; delays managing brain-dead patients due to cuts in official work hours; and enactment of the Life-Sustaining Treatment Act. The reasons listed by Cho
13 can be broadly classified into three categories: brain-death incidence factor, family consent factor, and donor management process factor. In this paper, we will analyze statistics to determine which of these factors actually led to the decrease in organ donation rate in 2017 and 2018.
Go to :

METHODS
This study analyzed published data of KODA annual reports from 2013 to 2018 on 11,636 potentially brain-dead organ donors. Definitions of terms utilized are as follows: 1) brain-dead potential organ donors (PBDs) are patients who meet the criteria of Glasgow Coma Scale score less than four due to irreversible brain injury and absence of brain stem reflex or possibility of progression to brain death. From a practical viewpoint, the actual incidence of brain-dead donors cannot be obtained, as number of PBDs is assumed as a representation of the brain-death incidence factor; 2) Eligible donors (ED) are those who passed the first brain death examination after obtaining family consent for organ donation; and 3) transplanted donors (TD) are those who completed organ donation after brain death determination and organ procurement surgery. The changes in numbers by time and causes of failure in PBD and ED were analyzed according to three factors that may affect brain-dead organ donation: 1) brain-death incidence factor; 2) family consent factor; and 3) donor management process factor.
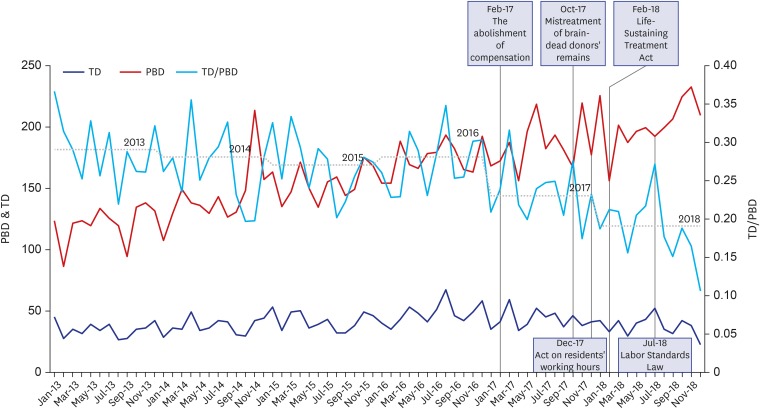
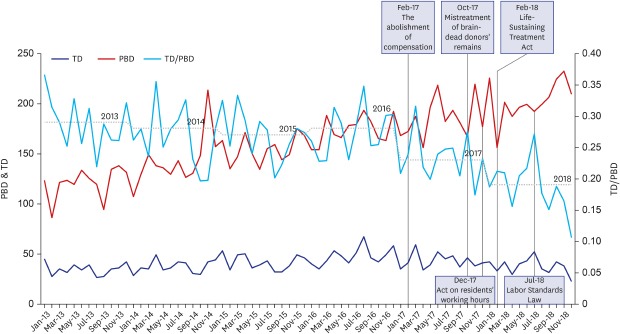
Brain-death incidence factor and family consent factor were examined by annual changes of PBD, ED, ED/PBD, and TD/PBD ratios to compare consent rates throughout the period. Then, monthly change in TD/PBD ratio was displayed along with five events related to consent from the family and donor management process factors. Finally, annual change in causes of failure to proceed with the organ donation process in PBD and ED were analyzed respectively to focus on which factor affected a more prominent change in the decrease in brain-dead organ donation.
Go to :

RESULTS
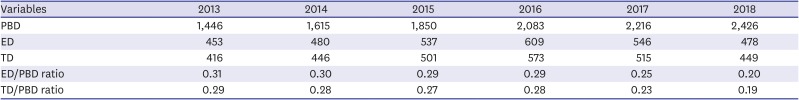
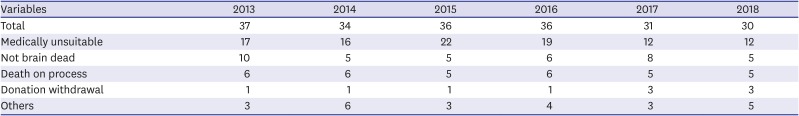
The number of PBD who registered in the KODA system consistently increased from 1,446 in 2013 to 2,426 in 2018 (
Table 1). However, the numbers of ED and TD declined after peaking in 2016. This trend is clearly presented with an ED/PBD ratio that abruptly and continuously decreased from 0.29 in 2016 to 0.25 in 2017. The ratio dropped even further to 0.20 in 2018. This shows that brain death incidence was not a factor for decrease in TD. There were several events that may have caused the decrease in TD. Abolishment of compensation, mistreated donor remains, the pilot program and nationwide implementation of the Life-Sustaining Treatment Act, implementation of an 80-hour work week for residents, and the amended Labor Standards Act all coincided with the decrease in TD. The first three events are related to family consent factor, and the others are associated with donor management process factor. The change in TD each incident was analyzed in chronological order (
Fig. 1).
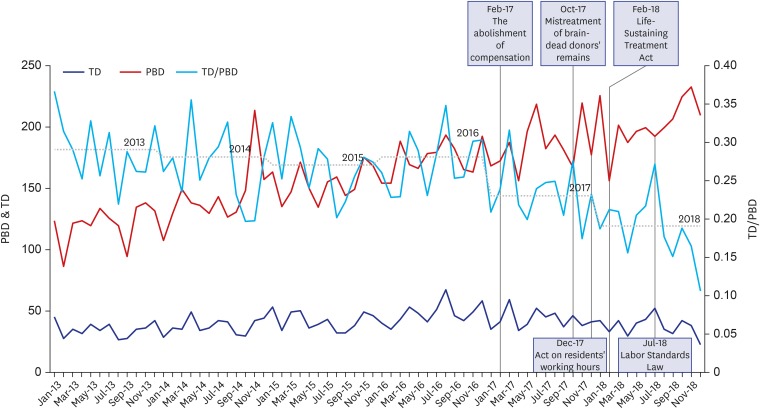 | Fig. 1
Relationship among monthly change of PBDs, TDs, and the ratio between them depending on events associated with the family consent factor and donor management process factor.
PBD = brain-dead potential organ donor, TD = transplanted donor.

|
Table 1
Annual change of PBD, ED, TD, and the ratios between them (2013–2018)
|
Variables |
2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
|
PBD |
1,446 |
1,615 |
1,850 |
2,083 |
2,216 |
2,426 |
|
ED |
453 |
480 |
537 |
609 |
546 |
478 |
|
TD |
416 |
446 |
501 |
573 |
515 |
449 |
|
ED/PBD ratio |
0.31 |
0.30 |
0.29 |
0.29 |
0.25 |
0.20 |
|
TD/PBD ratio |
0.29 |
0.28 |
0.27 |
0.28 |
0.23 |
0.19 |

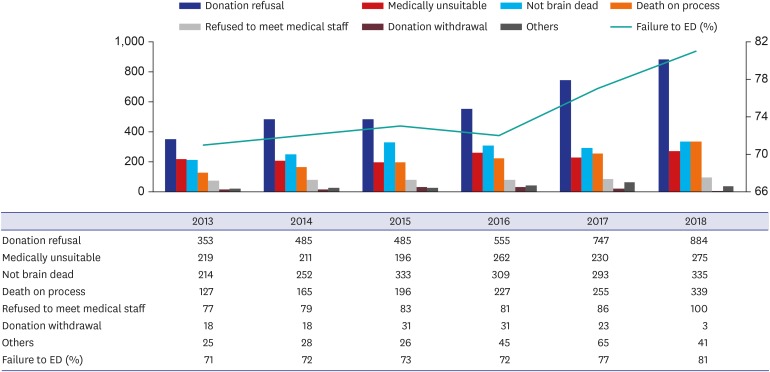
To determine the effect of family consent factor on decreased ED during the increment of PBD, this study analyzed the number of patients who dropped out of PBD during the process (
Fig. 2). The number of donation refusals increased from 353 (2013) to 555 (2016) and increased more rapidly from 747 (2017) to 884 (2018). The increment in donation refusal continued to worsen year after year from 2016 to 2018, when the events related to family consent factors occurred. The number of death on process soared in 2018, which implies that life-sustaining treatment has been forgone in more PBD, resulting in death. Patients who experienced withdrawal of life-sustaining treatment rather than organ donation most likely were recorded in “death” statistics. The same inference can be drawn from the sharp decrease in number of patients whose family withdrew willingness to donate in 2018. As families have had the new option of forgoing life-sustaining treatment since 2018, patient's family may not express their willingness to donate, in the first place, which makes no need to withdraw from that expressed willingness afterward.
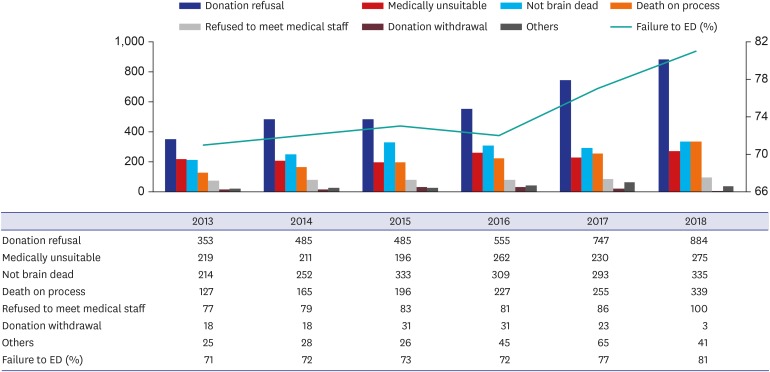 | Fig. 2
Change of causes of failure to proceed to EDs from brain-dead potential organ donors from 2013 to 2018.
ED = eligible donor.

|
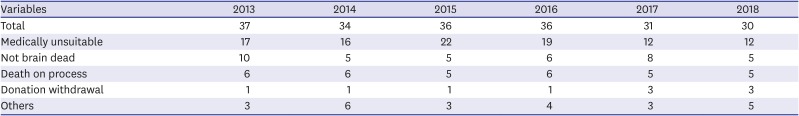
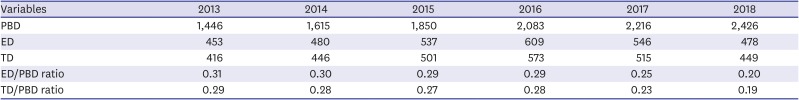
To understand the causes of withdrawal during the donor management process, this paper examined the number of each type of failure during the process (
Table 2). The total number of failures decreased consistently from 2013 to 2018, showing that overall quality of the management process improved during that time. In particular, the number of potential donors judged unsuitable has decreased since 2016. Therefore, donor management process factor is less likely the substantial cause of reducing TD.
Table 2
Causes of donation failure in eligible donors during the donor management process (2013–2018)
|
Variables |
2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
|
Total |
37 |
34 |
36 |
36 |
31 |
30 |
|
Medically unsuitable |
17 |
16 |
22 |
19 |
12 |
12 |
|
Not brain dead |
10 |
5 |
5 |
6 |
8 |
5 |
|
Death on process |
6 |
6 |
5 |
6 |
5 |
5 |
|
Donation withdrawal |
1 |
1 |
1 |
1 |
3 |
3 |
|
Others |
3 |
6 |
3 |
4 |
3 |
5 |

Go to :

DISCUSSION
In this study, the numbers of ED and TD decreased since 2017, while the number of PBD has constantly increased since 2013. The steady rise in PBD suggests that the brain-death incidence factor was not the significant cause of the decreases in ED and TD. Rather, it was primarily due to the decrease in family consent, which contributed to a reduction of TD in 2017 and 2018, considering that family consent is essential to be ED. The study chronologically listed events that may have led to the reduction in TD, comprising abolishment of compensation, mistreated donor remains, the pilot program and nationwide implementation of the Life-Sustaining Treatment Act, the 80 hours work week regulation for residents, and the amended Labor Standards Act. The first three possible causes could have had a direct impact on family consent. The latter two causes may delay or reduce quality in the donor management process. Although it cannot be conclusively determined which event caused the decrease in TD and how much decrease it caused, it could be shown that the influence of the family consent factor was important. This factor is likely responsible for the increased number of dropouts when proceeding from PBD to ED with a decrease in number of dropouts when proceeding from ED to TD. There was indirect evidence that led us to suspect that more families chose to forgo life-sustaining treatment according to the Life-sustaining Treatment Act, instead of donating organs. The donation refusal rate, which has increased in the past five years, increased even more in 2017 and 2018.The proportion of deaths before becoming an ED increased in 2018, and the number of withdrawals from willingness to donate decreased simultaneously. Considering that the people in TD were diagnosed with the diseases that can lead them both to brain death and to end-of-life process,
1415 the Life-sustaining Treatment Act seems to provide an alternative for a brain-dead patient's family. However, the decrease in ED began even before implementation of the Life-sustaining Treatment Act, indicating that abolishment of compensation or mistreated donor's remains may have also contributed to the decrease in family consent.
Donor willingness or family provision of consent is essential for organ donation, because it justifies the inevitable harm caused by the donation process.
16 For donation, a patient must undergo the process for determining brain-death, which has nothing to do with recovery of health, and the physical integrity of the body is damaged. This harm can only be justified by patient consent as an altruistic motive. Unless the process of organ donation is based on a donor's voluntary intention, or the legal equivalent thereof, the legitimate grounds for donation can be severely undermined even though the recipient could benefit hugely from receiving the donated organ.
The decline in number of brain-dead organ donors in 2017 and 2018 resulted from decrease in donor family consent rate. One possible cause that may have contributed to this reduction is legislation of the Life-Sustaining Treatment Act in 2016,
9 which provided a legal procedure whereby brain-dead patients could die without having to donate their organs. Therefore, we presume that, before enactment of the Life-Sustaining Treatment Act, at least some brain-dead organ donations were carried out to legally allow the patient to die, not primarily for the purpose of organ donation. The act of organ donation may have been the only choice for family members who did not wish to leave the brain-dead patient on life-sustaining treatment with no chance of recovery. In these circumstances, the decision to donate organs cannot be seen as made either by the previously stated free will of the brain-dead patient or by the family based on the patient's inferred desires. The current trend of declining brain-dead organ donation indicates that brain-dead donors and their families were forced into making unwanted decisions due to a loophole in the law.
Another possible cause behind the decline in brain-dead organ donation since 2017 is report of an incident in which brain-dead donor remains were mistreated and the subsequent media coverage.
13 When the voluntary altruistic behavior of a donor and family is answered with disrespectful and thoughtless responses, the bereaved family can suffer intense pain and produce loss of faith in the system. However, showing respect to brain-dead donors and their families is different from offering financial incentives. Even if discontinuing compensation since February 2017 resulted in decrease in TD, this suggests that compensation induced families to provide consent
17 out of “financial considerations” or for “material gain”
18 which are unjustifiable.
Fortunately, having understood the direness of the situation of donor shortage, the government and concerned institutions are seeking to address the decrease in number of brain-dead donors. A part of this effort is to establish a legal framework that allows the Life-Sustaining Treatment Act and OTA to work together. There is an attempt to legalize donation after circulatory death (DCD) based on prior patient consent, especially from patients who will die due to withdrawal of life-sustaining treatment.
13 If the Act is amended to include questions on organ donation in advance directives on Life-sustaining Treatment Plan or Advance Statement on Life-sustaining Treatment, patients must be provided sufficient information to give informed consent. In addition, promotion of government policy and education on organ donation is needed to enhance the understanding of organ donation.
19 The government is also making efforts to ensure that organ donors and bereaved families are treated with respect. KONOS released an integrated guideline on respectful treatment of organ donors and their families,
20 and KODA extended its support program for donor families of the hospitals contracted with KODA to include all donor families nationwide. If these efforts succeed, the consent of patients and families will increase to ultimately increase the number of TD.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download