Infectious diseases (ID) physicians perform various essential roles, ranging from prevention, diagnosis, and treatment of ID, outpatient-based antibiotics therapy, infection prevention and control, antimicrobial stewardship, education, research, and response to emerging ID.
1 In Korea, the influenza pandemic of 2009 and the Middle East respiratory syndrome pandemic of 2015 highlighted the importance of expertise in ID. Further, the deadly outbreak of coronavirus disease 19 (COVID-19) has again raised public interest in the ID physician workforce.
23
In Korea, the Infectious Diseases Division was established in 1946. After 70 years, there are currently 275 registered ID physicians, accounting for 3.4% of 7,905 sub-specialists of the Internal Medicine Department, and only 86 are registered ID pediatricians.
4 The shortage of ID physicians is also a rising concern in other countries. In the United States (US), the number of ID physician applications declined to about 40% in 2017 compared to 2009 and failed to meet the yearly quota.
5 As the global threat of antibiotic-resistant organisms and emerging ID increases, the roles of ID physicians have been emphasized, and several countries have reported their ID physician workforce.
6789 However, there is limited information regarding the ID physician workforce in Korea. This study aimed to evaluate the ID physicians' current working status and distribution according to location, healthcare delivery system, and types of medical institutions to provide fundamental data on ID physicians.
We retrospectively investigated sex, workplace (by 17 administrative districts), and type of medical institution (by healthcare delivery system and category of medical institutions) of each ID physician as of June 2020. We investigated physicians' acquisition with ID sub-specialty from 1992 to 2019 for the first time since the sub-specialty was established in Korea. We also investigated the annual number of total specialists and internal medicine specialists between 2009 and 2019.
10 Population data were obtained from the Population Census Division of the National Statistical Office.
10 To calculate the number of beds per ID physician, we investigated data on the number of beds available in each medical institution, based on facility data reported to the Health Insurance Review and Assessment Service.
11 The number of beds calculated excluded those in the delivery room, operation room, and physical therapy clinic.
An ID physician was defined as a physician who has passed the ID board examination recognized by the Korean Association of Internal Medicine. The medical institutions were classified into four subtypes based on their healthcare delivery system: 1) tertiary-care hospital, 2) general hospital, 3) hospital, and 4) medical clinic. Based on the medical service act, the medical institutions were categorized into four subtypes: 1) private/university-affiliated hospital, 2) public/university-affiliated hospital, 3) private/non-university-affiliated hospital, 4) public/non-university-affiliated hospital. The public hospital criterion was based on lists of current public health care institutions' situations, announced on 31st December 2018 by the Ministry of Health and Welfare.
12 Active ID physicians were defined as physicians working at hospitals, including tertiary-care and general hospitals, except medical clinics or non-clinical services. In this study, we considered ID physicians working at medical clinics as not playing ID physicians' roles; therefore, we excluded them. ID physician density was defined as the number of ID physicians per 100,000 population at the country level.
Statistical analysis was performed using Rex version 3.3.2.3 (RexSoft Inc., Seoul, Korea). We compared annual numbers of total specialists, internal medicine specialists, and ID physicians from 2009 to 2019, using negative binomial regression analyses. Continuous variables were expressed as median (interquartile range [IQR]), whereas categorical variables were expressed as frequencies and percentages. Variables with P values ≤ 0.05 were considered statistically significant.
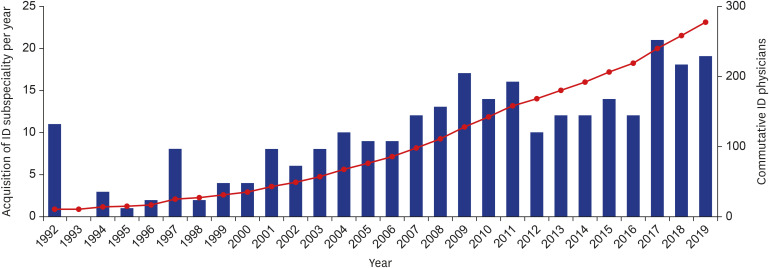
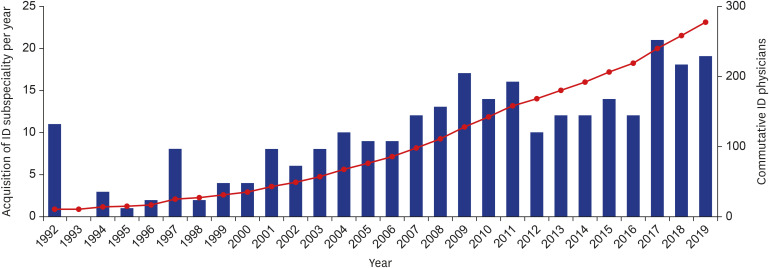
In total, 275 physicians completed the ID sub-specialty training from 1992 to 2019 (
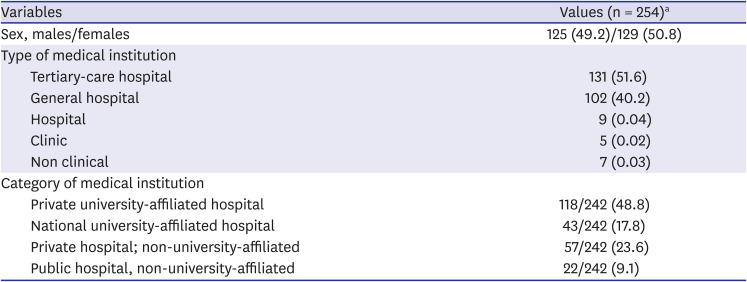
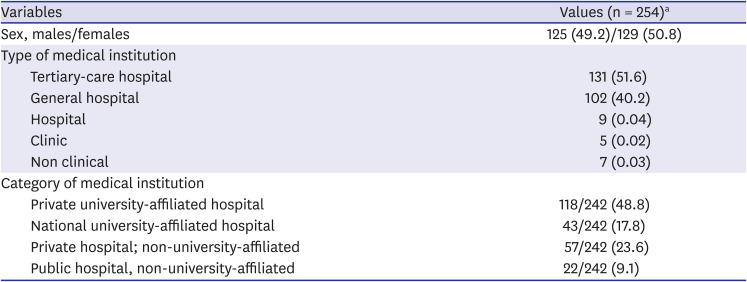
Fig. 1). The median number of ID sub-specialty physicians acquired each year was 10, ranging from 0 to 21. Among them, 242 were currently active ID physicians, excluding those who were not-identified (n = 11), deceased (n = 5), retired (n = 3), taking time off (n = 2), working at medical clinics (n = 5), and undertaking non-clinical employment (n = 7). Working place of non-clinical employments were governmental agencies (n = 2), pharmaceutical companies (n = 2), non-governmental organization (n = 1), chief executive officer (n = 1), and research institution (n = 1). We observed that 91.8% of ID physicians were employed in tertiary-care or general hospitals. In terms of the category of medical institutions, 47.8% of ID physicians worked in private/university hospitals, followed by 25.9% in private/non-university hospitals (
Table 1).
Fig. 1
The accumulated acquisition of physicians with ID sub-specialty by year.
ID = infectious diseases.

Table 1
Status of infectious diseases physicians in Korea
|
Variables |
Values (n = 254)a
|
|
Sex, males/females |
125 (49.2)/129 (50.8) |
|
Type of medical institution |
|
|
Tertiary-care hospital |
131 (51.6) |
|
General hospital |
102 (40.2) |
|
Hospital |
9 (0.04) |
|
Clinic |
5 (0.02) |
|
Non clinical |
7 (0.03) |
|
Category of medical institution |
|
|
Private university-affiliated hospital |
118/242 (48.8) |
|
National university-affiliated hospital |
43/242 (17.8) |
|
Private hospital; non-university-affiliated |
57/242 (23.6) |
|
Public hospital, non-university-affiliated |
22/242 (9.1) |

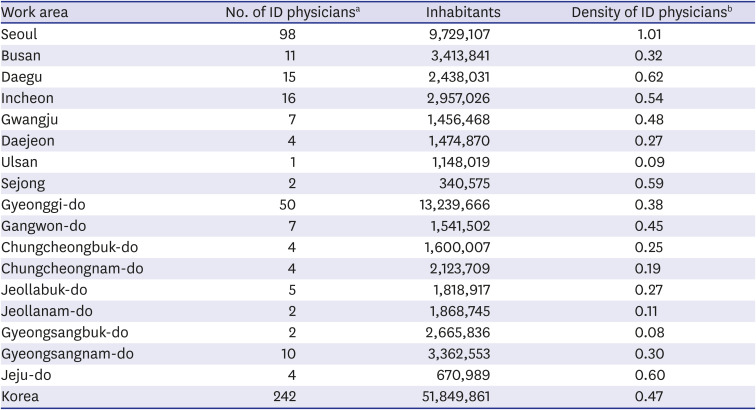
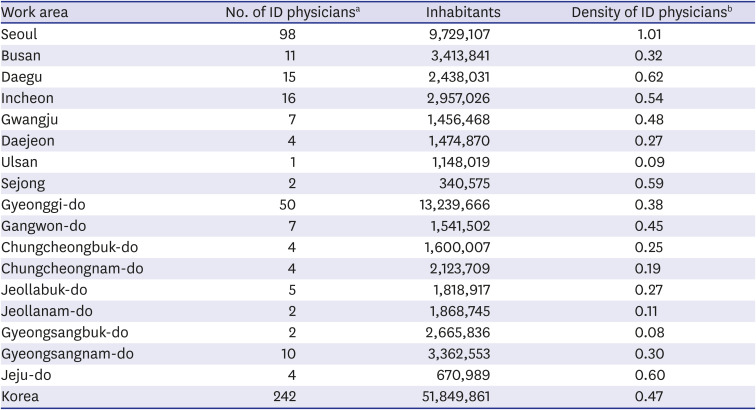
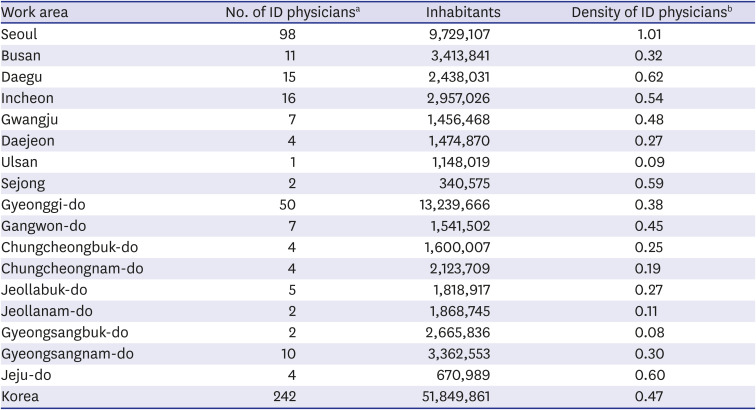
The density of ID physicians who were currently active in 2019 was 0.47 per 100,000 population. In terms of geographical distribution, Seoul had the highest density of the workforce (1.01), followed by Daegu (0.62) and Jeju Island (0.60). Gyeongsangbuk-do had the lowest density of 0.08 (
Table 2 and
Supplementary Fig. 1). Eleven administrative districts (64.7%) out of seventeen did not attain the average ratio of 0.47. There were 131 hospitals with Infectious Diseases Division, and the median number of beds per ID physician was 372 (IQR, 280–507) (
Supplementary Table 1). General hospitals had the highest number of beds per ID physician, followed by tertiary-care hospitals. For the medical institution category, the highest number of ID physicians (65.1%) worked at university hospitals, and up to three quarters (73.6%) of ID physicians practiced at private hospitals.
Table 2
Distribution of active infectious diseases physicians by region
|
Work area |
No. of ID physiciansa
|
Inhabitants |
Density of ID physiciansb
|
|
Seoul |
98 |
9,729,107 |
1.01 |
|
Busan |
11 |
3,413,841 |
0.32 |
|
Daegu |
15 |
2,438,031 |
0.62 |
|
Incheon |
16 |
2,957,026 |
0.54 |
|
Gwangju |
7 |
1,456,468 |
0.48 |
|
Daejeon |
4 |
1,474,870 |
0.27 |
|
Ulsan |
1 |
1,148,019 |
0.09 |
|
Sejong |
2 |
340,575 |
0.59 |
|
Gyeonggi-do |
50 |
13,239,666 |
0.38 |
|
Gangwon-do |
7 |
1,541,502 |
0.45 |
|
Chungcheongbuk-do |
4 |
1,600,007 |
0.25 |
|
Chungcheongnam-do |
4 |
2,123,709 |
0.19 |
|
Jeollabuk-do |
5 |
1,818,917 |
0.27 |
|
Jeollanam-do |
2 |
1,868,745 |
0.11 |
|
Gyeongsangbuk-do |
2 |
2,665,836 |
0.08 |
|
Gyeongsangnam-do |
10 |
3,362,553 |
0.30 |
|
Jeju-do |
4 |
670,989 |
0.60 |
|
Korea |
242 |
51,849,861 |
0.47 |

Total specialists increased from 56,903 in 2009 to 84,470 in 2019, and internal medicine specialists increased from 9,808 in 2009 to 15,697 in 2019. In the same period, the ID physicians increased from 127 in 2009 to 275 in 2019 (
Supplementary Fig. 2). The number of ID physicians showed a higher increase rate than total specialists and internal medicine specialties (
P < 0.001).
This study showed 242 ID physicians currently in practice: 0.47 ID physicians per 100,000 population and a median of 372 beds per ID physician. Two-thirds of ID physicians worked in the national capital region (Seoul, Gyeonggi-do, and Incheon). Most ID physicians were with general or tertiary-care hospitals when classified by the healthcare delivery system level. Most ID physicians in Korea were clinically active in their role as ID specialists.
Only seven ID physicians were in a non-clinical position. Among them, only two were working for a government institution. Due to the lack of ID physicians in government agencies, policy decisions may not reflect the opinions of ID physicians. Since ID physicians assume many exclusive roles, including education, research, antimicrobial stewardship, hospital infection control, and management of complicated and severe ID, it is reasonable that most ID physicians are seen in large-scale hospitals with sufficient medical resources. However, the field of ID specialty is not limited to clinical work. To effectively deal with emerging and epidemic ID outbreaks, more effort is needed to support non-clinical ID physician workforce, such as ID physician-scientists, journalists, and administrators.
The geographical distribution of ID physicians was uneven. Such uneven distribution was also noted in the distribution of other specialists in Korea.
1314 The reasons for uneven distribution might be lack of training hospitals in rural areas or individuals' lifestyle decisions. The factors influencing uneven distribution can be objective and subjective, including income according to regions and lifestyle preferences. Further studies are needed on the causes of uneven distribution of ID physician workforce.
There is no authorized standard of staffing for ID physicians, but a few studies suggest guidelines for optimal numbers. According to the survey of 567 hospitals in 61 countries in Europe, between April and July 2015, the median number of ID physicians/Clinical microbiologists/Infection control physicians was 1.12 per 100 beds (IQR, 0.56–2.13).
7 In hospitals performing regular antimicrobial stewardship programs and infection control activity, the ratio was 1.21 (IQR, 0.56–2.14).
7 A multicenter retrospective study in Korea revealed that each medical institution required 3 personnel per 1,000 beds to review 25% of the hospitalized cases that underwent antibiotic therapy as an antimicrobial stewardship activity.
15 Based on recent research from the US, the national average density of ID physicians was 1.76 per 100,000 population in 2017.
9 In Brazil, the number of ID physicians was 3,229, with a density of 16.06 per million inhabitants.
8 Although the number of ID physicians in Korea has been increasing more rapidly than internal medicine and total specialists over the past decade, the current workforce seems to be far lesser (0.47 per 100,000 populations) than in other countries.
We suggest establishing reasonable policies that can attract physicians to choose ID as their specialty is necessary. For example, fair compensation is needed in the economic evaluation of the invisible activities of ID physicians, especially activities of infection control and antimicrobial stewardship. Moreover, as the importance of infection control is more evident due to continuous epidemics of emerging ID, designating the required number of ID physicians according to the number of beds, apart from infection control doctors, might be a strategy to overcome the current situation.
This study had some limitations. The study population was limited to ID physicians treating adults only; therefore, we could not estimate the infection-related specialist workforce, including pediatric ID specialists and clinical microbiologists. Second, we did not assess all aspects of the assignment, such as the actual scope of work, workloads, and compensations. Further studies with in-depth surveillance or interview are needed to overcome these limitations.
The increasing significance, scarcity, and wide regional disparity of ID physicians have been highlighted, emphasizing the current domestic status, particularly with the COVID-19 pandemic. It is crucial to secure qualified experts to properly deal with community and hospital-acquired ID, antimicrobial resistance, and emerging ID, including COVID-19, and execute exclusive tasks of ID physicians.
Ethics statement
This study was approved by the Institutional Review Board (IRB) and Ethics Committee of Soonchunhyang University Seoul Hospital (IRB No. 2020-05-016). Informed consent was waived by the board.