This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Longitudinal integrated clerkships (LICs) have been adopted by medical schools to overcome the limitations of traditional block clerkship rotations and to promote continuity of care. In 2018, Seoul National University College of Medicine introduced a patient-centered LIC program as part of a new curriculum in parallel with traditional block rotation clerkships. The purpose of this study was to present the patient-centered LIC program and to investigate its educational effects.
Methods
In 2018 and 2019, a total of 298 third-year medical students participated in the LIC program. We divided the students into groups of eight, which were organized into corresponding discussion classes. Throughout the academic year, students followed up patients by interviewing them at the hospital or reviewing their electric medical records. Discussion classes on set topics were held seven times per year with facilitators and clinical faculites. Students completed a course evaluation questionnaire at the end of the academic year. The questionnaire included 22 items measured on a 5-point scale and two open-ended questions asking about the benefits and limitations of the program. The items covered three domains: student experience, satisfaction, and self-assessment. Final reflective essays were collected as both student assessments and data for qualitative analysis.
Results
During the study period, the overall experience of the students improved. We increased the number of faculty members and patients and decreased the number of students in each discussion class. We also provided additional feedback through an e-portfolio. Students' satisfaction changed positively. Compared to the rotational clerkship, students answered that the LIC provided additional help in learning the two core competencies. During the first 2 years of the program, the percentage of students who answered that the program was more helpful than the rotational clerkship increased from 23.7% to 46.4% for continuity of care (P < 0.001), and from 20.5% to 50.7% for patient-centered care (P < 0.001).
Conclusion
Our patient-centered LIC, in parallel with traditional block rotation clerkships, had a positive effect on students' experience of continuity of care and patient-centered care.
Go to :

Graphical Abstract
Go to :

Keywords: Longitudinal Integrated Clerkship, Continuity of Patient Care, Patient-centered Care
INTRODUCTION
Despite the remarkable changes that have occurred in the healthcare environment and the practice of medicine, the fundamental model of clinical education in medical schools has changed little for decades.
1 With increasing recognition of the social, ethical, and economic aspects of healthcare, the concept of continuity of care has been emphasized. Continuity of care has become an important goal for healthcare policy in many countries, and several studies have investigated associations between continuity of care and health outcomes.
2 Higher levels of continuity of care have been found to be associated with reduced risks of hospital and emergency department use and lower healthcare costs. Another important change is the paradigm shift towards patient-centered care. The movement to overcome the limitations of disease-centered and doctor-centered healthcare has influenced healthcare policy initiatives launched by the World Health Organization.
34 In the US, the Hospital Consumer Assessment of Healthcare Providers and Systems survey has affected Centers for Medicare and Medicaid reimbursement to hospitals since 2013.
5 In Korea, with the increasing recognition of the importance of patient experience, studies on patient satisfaction have been conducted and the Korean Health Insurance Review and Assessment Service published a report evaluating patients' experience in 2017.
67
However, traditional clerkships, which consist of a series of short rotations in specialty disciplines, have several limitations in terms of helping students to learn about the concepts of continuity of care and patient-centered care.
8 Shortened inpatient stays and the shift toward ambulatory management have had a negative impact on student learning.
910 Due to the need to ensure patient safety, it is difficult for students to practice their skills; to overcome this, the number of outpatient clinic clerkships has increased and simulations have been more frequently implemented prior to practice. In order to overcome these limitations, several medical schools have developed longitudinal integrated clerkships (LICs) as a model for the structural redesign of clinical education.
The LIC is an innovative approach in medical education that emphasizes continuity as a key principle to provide student-centered experience and learning. Unlike a traditional clerkship, medical students participate in the comprehensive care of patients over time and have continuing learning relationships with the patients' clinicians.
11 According to the Association of American Medical Colleges Curriculum Inventory and Reports, the LIC model is growing in popularity, increasing from 29 schools during the 2010–2011 academic year to 44 in 2014–2015.
12 Internationally, rapid growth in LICs has been documented in seven countries on four continents. However, LICs have not been widely adopted in Asian countries.
The Seoul National University College of Medicine introduced a patient-centered LIC into the curriculum in 2018. In our pilot studies with 22 students in 2016 and 2017,
13 we discussed issues related to the successful implementation of LICs in Korea. Two core competencies of our LIC program are to understand the continuity of the patient's medical experience and the concept of patient-centered care. The purpose of this study is to describe the implementation of a patient-centered LIC program at Seoul National University College of Medicine and to investigate its educational effects.
Go to :

METHODS
As described in our prior study, the LIC program aimed to benchmark previously described reported LIC programs, but was implemented in combination with traditional clerkships in the form of block rotations.
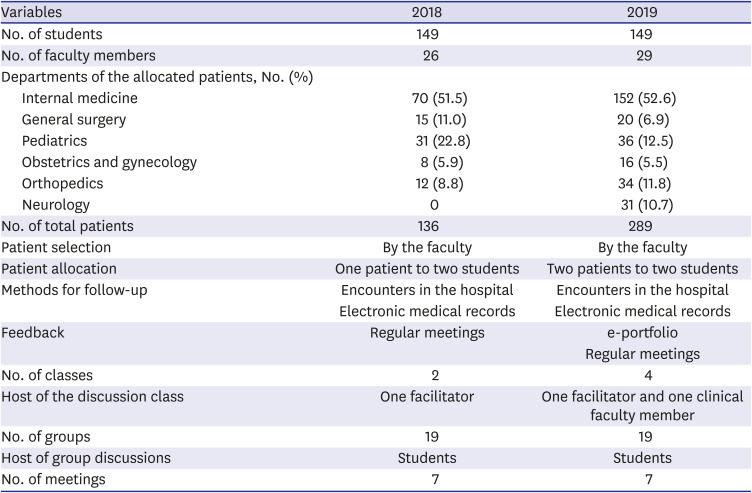
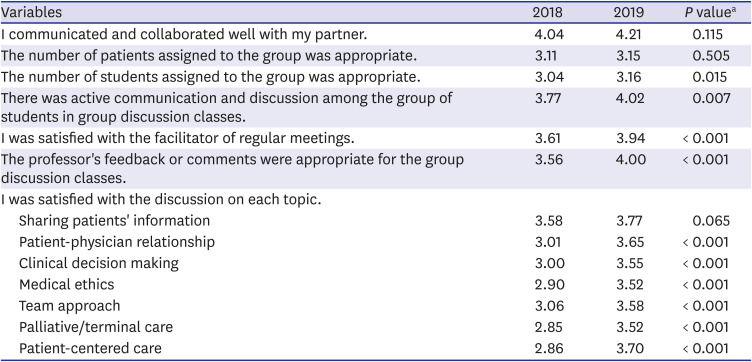
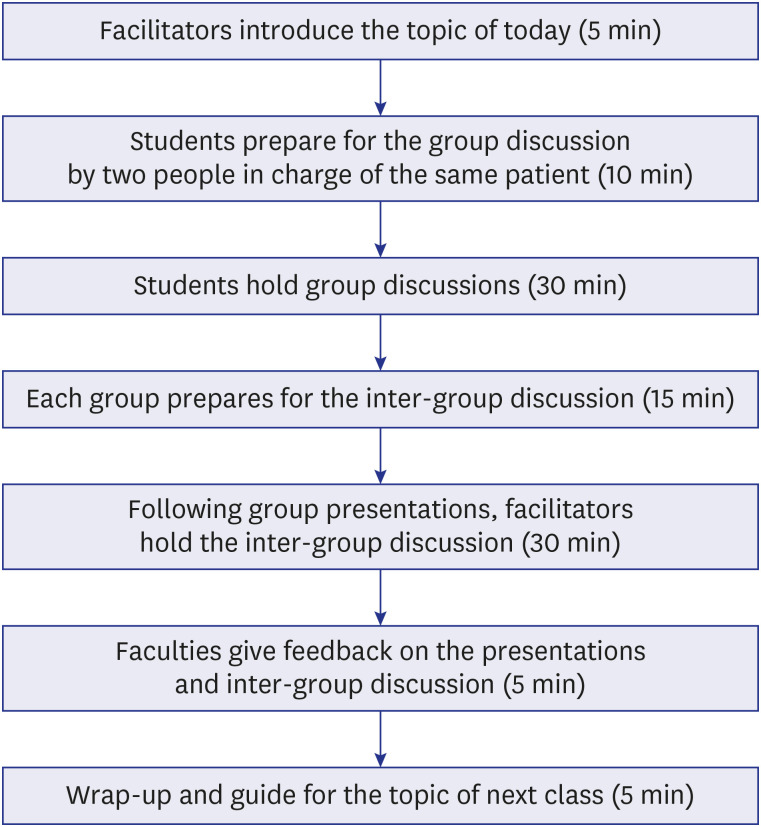
13 Before the semester began, we recruited participating clinical faculty members and held a meeting of the LIC committee. We divided the students into groups of eight, which were organized into corresponding discussion classes. At the beginning of the LIC program, we presented students with an overall overview of the program, including the concept of patient-centered care, the concept of continuity of care, and the procedures of the small-group discussion classes. When block rotation clerkship began, each participating professor provided the office of medical education with a list of hospitalized patients suitable for long-term follow-up. One or two patients were allocated to a pair of two students, and long-term follow-up began. The students met patients when patients visited the hospital, and if doing so was not possible, students followed up their patients by reviewing the patients' electronic medical records. Patient allocation was carried out for 1–2 months, and the discussion classes began when all students had been assigned a patient. The discussion classes were held seven times a year, with one facilitator and/or one clinical faculty member in each class, according to a set topic (
Fig. 1). The topics were case sharing, the patient-physician relationship, clinical decision-making, medical ethics, team care, end-of-life-palliative care, and patient-centered care. Before and after the discussion classes, clinical faculty members and facilitators met to debrief and share feedback on each class. Students received feedback from the clinical faculty member who assigned the patient, and feedback was provided during the discussion class. The structure of the 2018 and 2019 LIC programs is summarized in
Table 1.
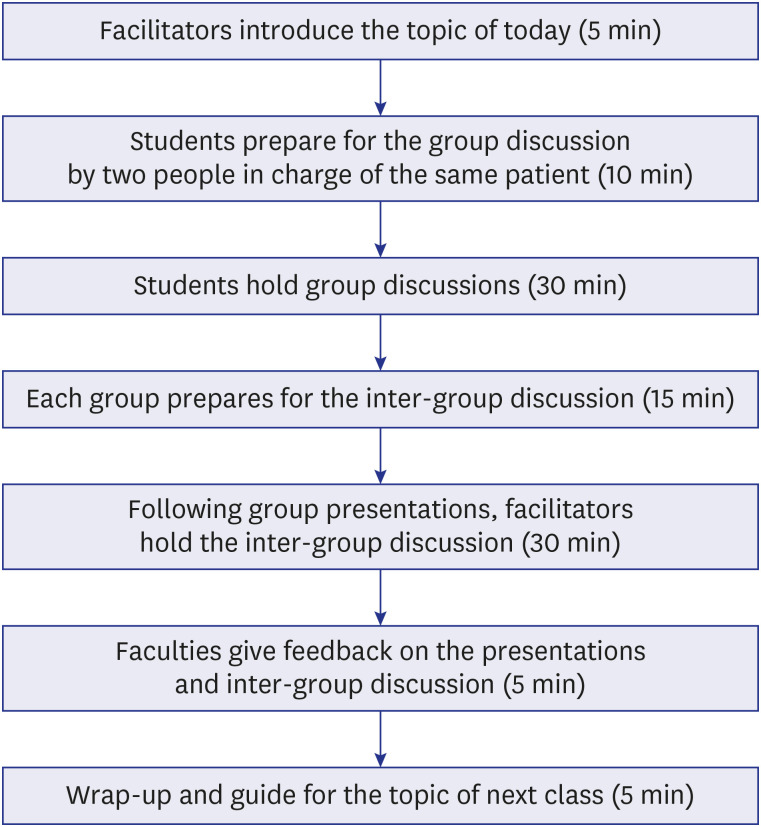 | Fig. 1 Procedures of the group discussion classes in the longitudinal integrated clerkship. Each discussion class took about 2 hours, including a 10-minute break.
|
Table 1
Structure of the program in 2018 and 2019
|
Variables |
2018 |
2019 |
|
No. of students |
149 |
149 |
|
No. of faculty members |
26 |
29 |
|
Departments of the allocated patients, No. (%) |
|
|
|
Internal medicine |
70 (51.5) |
152 (52.6) |
|
General surgery |
15 (11.0) |
20 (6.9) |
|
Pediatrics |
31 (22.8) |
36 (12.5) |
|
Obstetrics and gynecology |
8 (5.9) |
16 (5.5) |
|
Orthopedics |
12 (8.8) |
34 (11.8) |
|
Neurology |
0 |
31 (10.7) |
|
No. of total patients |
136 |
289 |
|
Patient selection |
By the faculty |
By the faculty |
|
Patient allocation |
One patient to two students |
Two patients to two students |
|
Methods for follow-up |
Encounters in the hospital |
Encounters in the hospital |
|
Electronic medical records |
Electronic medical records |
|
Feedback |
Regular meetings |
e-portfolio |
|
Regular meetings |
|
No. of classes |
2 |
4 |
|
Host of the discussion class |
One facilitator |
One facilitator and one clinical faculty member |
|
No. of groups |
19 |
19 |
|
Host of group discussions |
Students |
Students |
|
No. of meetings |
7 |
7 |

Subjects
The study was conducted among the 298 students at Seoul National University Collage of Medicine who participated in the LIC program in 2018 and 2019. The course evaluation questionnaire was completed by third-year medical students. The questionnaire included 22 items measured on a 5-point scale and two open-ended questions asking about the benefits and limitations of the program. The items covered three domains; student experience (patient characteristics and continuity), discussion classes (peers, faculty members, satisfaction with each topic), and self-assessment (comparisons with traditional clerkships). A frequency analysis of responses to the items was first conducted to identify key features.
Final reflective essays were collected as both student assessments and data for qualitative analysis. The facilitators assessed the essay reports at the end of the semester.
Statistical analysis
The statistical analysis was performed using SPSS version 23 (IBM Corp., Armonk, NY, USA). The Shapiro-Wilk normality test was performed before comparisons were made between groups using the unpaired Student's t-test. P values of < 0.05 were considered to indicate statistically significant differences.
Ethics statement
The Institutional Review Board of Seoul National University College of Medicine and Seoul National University Hospital exempted this study from review since it was an analysis of de-identified data (E-2001-016-1091).
Go to :

RESULTS
Based on the experience and feedback we received during 2018, we changed some of the programs in 2019 (
Table 1). Clinical faculty members and facilitators recommended that the patients should have suitable characteristics for the LIC program, and that the size of the discussion classes should be decreased. Among the differences between the 2018 and 2019 programs, we increased the number of faculty members and patients, with the goal of including a greater variety of cases. Based on this, the number of patients assigned to students was more than doubled (from 136 patients to 289 patients). Second, the meetings were changed to comprise four classes with fewer students to ensure that discussions were active. Third, we combined additional feedback through an e-portfolio as well as feedback through face-to-face discussions to enhance the interactions.
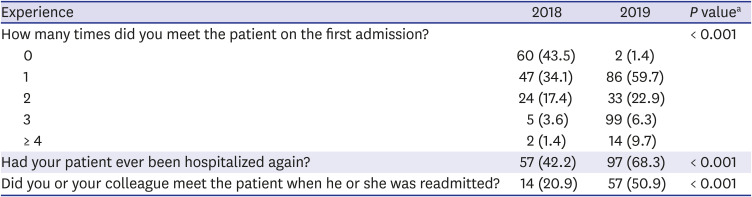
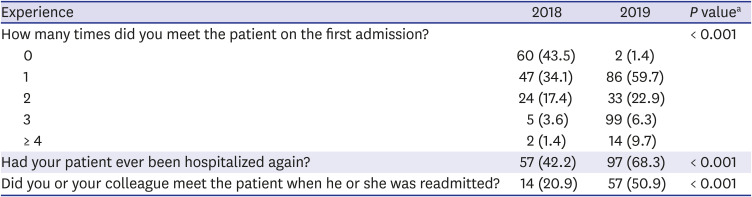
Nearly all (95.3%; 284/298) students answered the questionnaire. The survey results, presented in
Table 2, show a comparison of students' experience in 2018 and 2019. In 2019, the number of times students met their assigned patients significantly increased (
P < 0.001). The students were able to meet a wider range of patients. The proportion of assigned patients who were re-hospitalized increased from 42.2% to 68.3% (
P < 0.001). The rate of face-to-face follow-up with those patients also increased by 2.5-fold (
P < 0.001).
Table 2
Survey results on patient experience in 2018 and 2019
|
Experience |
2018 |
2019 |
P valuea
|
|
How many times did you meet the patient on the first admission? |
|
|
< 0.001 |
|
0 |
60 (43.5) |
2 (1.4) |
|
1 |
47 (34.1) |
86 (59.7) |
|
2 |
24 (17.4) |
33 (22.9) |
|
3 |
5 (3.6) |
99 (6.3) |
|
≥ 4 |
2 (1.4) |
14 (9.7) |
|
Had your patient ever been hospitalized again? |
57 (42.2) |
97 (68.3) |
< 0.001 |
|
Did you or your colleague meet the patient when he or she was readmitted? |
14 (20.9) |
57 (50.9) |
< 0.001 |

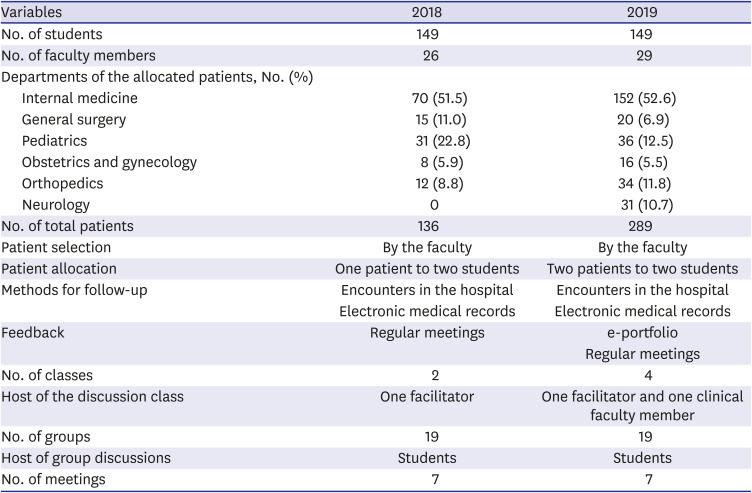
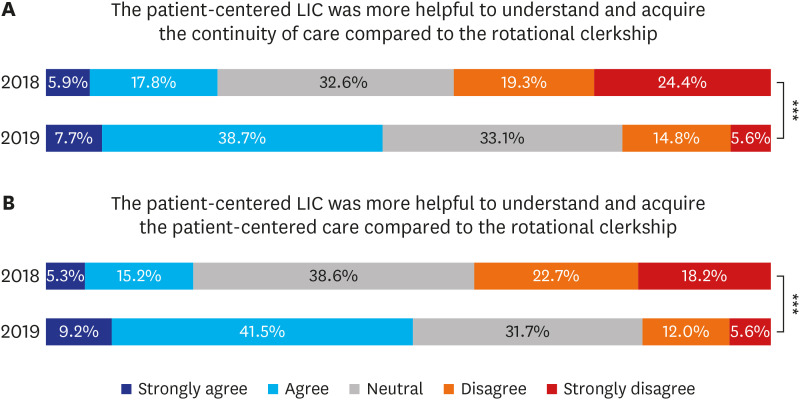
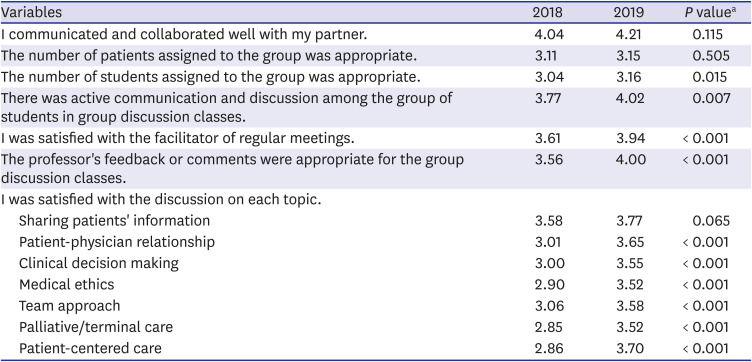
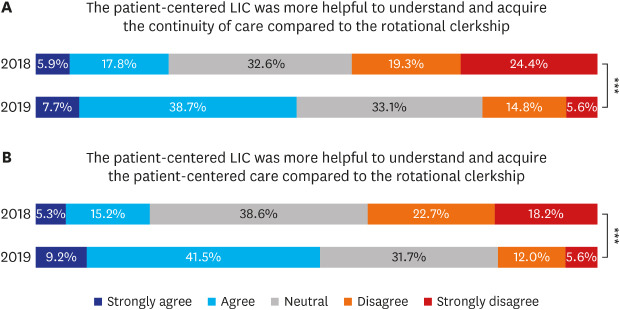
The overall satisfaction of the students improved (
Table 3). In 2018, the satisfaction of students was neutral or near-dissatisfied. In contrast, most of the students in 2019 were satisfied with active communication among students (4.02/5) and with the facilitator (3.94/5). The perceived appropriateness of the professor's feedback significantly increased from 2018 (3.56/5) to 2019 (4.00/5). Compared to the rotational clerkship, students answered that the LIC provided additional help with learning the two core competencies (continuity of the patient's medical experience and the concept of patient-centered care) (
Fig. 2). The percentage of students who answered that the program was more helpful than the rotational clerkship to learn these two core competencies increased from 23.7% to 46.4% for continuity of care and from 20.5% to 50.7% for patient-centered care.
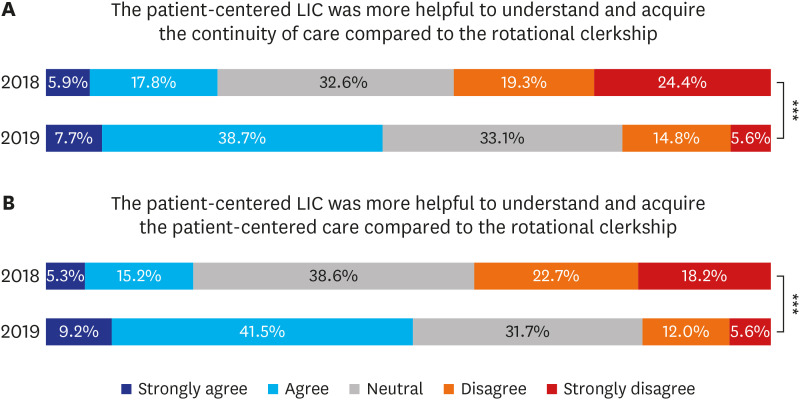 | Fig. 2
Self-assessment of the educational effect of the patient-centered LIC in 2018 and 2019. (A) The patient-centered LIC was more helpful to understand and acquire the continuity of care compared to the rotational clerkship. (B) The patient-centered LIC was more helpful to understand and acquire the patient-centered care compared to the rotational clerkship. P value is calculated by χ2 test.
LIC = longitudinal integrated clerkship.
***P < 0.001.

|
Table 3
Satisfaction with group discussion classes
|
Variables |
2018 |
2019 |
P valuea
|
|
I communicated and collaborated well with my partner. |
4.04 |
4.21 |
0.115 |
|
The number of patients assigned to the group was appropriate. |
3.11 |
3.15 |
0.505 |
|
The number of students assigned to the group was appropriate. |
3.04 |
3.16 |
0.015 |
|
There was active communication and discussion among the group of students in group discussion classes. |
3.77 |
4.02 |
0.007 |
|
I was satisfied with the facilitator of regular meetings. |
3.61 |
3.94 |
< 0.001 |
|
The professor's feedback or comments were appropriate for the group discussion classes. |
3.56 |
4.00 |
< 0.001 |
|
I was satisfied with the discussion on each topic. |
|
|
|
|
Sharing patients' information |
3.58 |
3.77 |
0.065 |
|
Patient-physician relationship |
3.01 |
3.65 |
< 0.001 |
|
Clinical decision making |
3.00 |
3.55 |
< 0.001 |
|
Medical ethics |
2.90 |
3.52 |
< 0.001 |
|
Team approach |
3.06 |
3.58 |
< 0.001 |
|
Palliative/terminal care |
2.85 |
3.52 |
< 0.001 |
|
Patient-centered care |
2.86 |
3.70 |
< 0.001 |

Participants provided open-ended answers to questions on the benefits and limitations of the LIC, as well as any suggestions that they might have. Students expressed that the benefits of LIC were tracking patients over the course of long-term follow-up, studying a variety of topics (e.g., the patient-physician relationship and clinical decision-making), and learning from each other through group discussions.
“It was good to be able to think about the patient-physician relationship, clinical decision-making, and other discussion topics in addition to disease.”
“I was able to see changes in the patient's medical condition and emotional changes for a year and also learned to build rapport with a patient.”
The limitations identified by the students were being unable to meet patients due to schedule conflicts with block rotations and not having suitable patients for certain discussion topics or long-term follow-up. They suggested enhancing ways of obtaining information on patients' scheduled visits in advance, ensuring that each group had a sufficient variety of patients, and having fewer students in each discussion class.
“It is difficult to meet with assigned patients during the existing rotation clerkship schedule.”
“For a specific discussion topic, there were situations where there were no patients with relevant issues.”
“It would be nice to know in advance the patient's schedule for outpatient visits and readmission.”
Peers in the discussion group compared the patient-experience of their assigned patients to that of other members.
The final reflective essays provided data on students' clinical experience of seeing actual patients. Students commented that the LIC program with discussion classes helped them to understand the concepts of continuity of care and patient-centered care.
“…During the long-term observation of an aplastic anemia patient for a year, it was beneficial to experience the patient's diagnosis, treatment, and the entire recovery through the integrated clinical practice process. In the rotation clerkship, I could meet the patient for about a week in most cases. In my case, I met the patient with aplastic anemia and I could see and learn from the entire process, starting with the initial diagnosis and subsequent observation, immunotherapy, allogeneic stem cell transplantation preparation, and ultimately the management of complications after transplantation... Peers in the discussion group compared their patient to the cases of other members, depending on the nature of the disease the patients experienced, and we saw that the burden imposed on each individual varied even for patients with the same condition depending on their social and economic circumstances. We also believe that a sufficient and rich understanding of individual cases should be pursued in order to achieve integrated care, taking into account the circumstances surrounding the patient without being hindered by the disease…”
Go to :

DISCUSSION
In this study, we describe the LIC program implemented at Seoul National University Collage of Medicine, the process of improving the program from 2018 to 2019, and the educational effects of the program. This is the first LIC program to be introduced into the regular curriculum in Korea, and our experience with its development and improvement will help other medical schools considering the introduction of LIC. Through improvements in the program, student satisfaction and self-assessment of educational effects have changed in a positive direction.
In 2018, the first year of the program, there were a variety of problems. First, we provided students with insufficient patient experience. Some patients assigned to students were not appropriate for the topics of the discussion classes, and it was difficult for students to find time to meet with other patients. Another problem was that there were too many students in each discussion class. To solve these problems, we increased the number of assigned patients, added clinical faculty participants, and recruited a wider range of clinical departments. We also increased the number of facilitators staffing the discussion classes and changed them to small group discussions. These efforts dramatically improved the challenges regarding satisfaction and educational effectiveness faced in the second year of the LIC program.
Our newly developed LIC program is somewhat different from the LICs that have been reported to date. In 2017, the International Consortium of LICs proposed a consensus definition of LIC, according to which LICs share three common elements: 1) medical students participate in the comprehensive care of patients over time; 2) medical students have continuing learning relationships with these patients' clinicians, and 3) medical students meet the majority of the academic year's core clinical competencies across multiple disciplines simultaneously through the experience.
11 Currently, three distinct types of programs have been identified according to program length and disciplinary coverage: comprehensive LICs, blended LICs, and LIC-like amalgamative clerkships. Blended LICs account for 50%–89% of the duration of the academic year, all or the majority of disciplines are covered, linked complementary rotations external to the LIC complete the academic year, and these LICs usually take place in the penultimate year. In the present study, long-term patient tracking and continuous learning with medical staff are consistent with the consensus definition, but core clinical competencies were also acquired through a block rotation clerkship. The LIC program of our institution is closer to a blended LIC, but it is not complemented by the block-rotation clerkship; instead, the block-rotation clerkship is complemented by the LIC.
In 2019, we introduced additional e-portfolio feedback, unlike in 2018. Students wrote a report for their e-portfolio as they prepared for each discussion class, and received one-on-one feedback from their assigned clinical faculty members. E-portfolios are used in various fields of medical education.
14 In the LIC program, e-portfolios can be used to collect evidence of performance and reflections on that performance, before, during, and after the LIC to document learners' personal and professional development.
15 In the present study, the use of an e-portfolio was able to compensate for the limitation of there being relatively few opportunities for faculty and students to meet together. Furthermore, the e-portfolio may have motivated students to meet with their patients more frequently. The use of an e-portfolio could make program leaders to monitor student-faculty relationships to ensure students' educational and professional outcomes, which are important in the LIC program.
16
Some areas still need to be improved in the LIC program that we developed. First, we need to arrange for students to be able to have in-person meetings when their assigned patients visit the hospital. Our blended LIC and the rotational clerkship have a complementary relationship. When schedule conflicts occur, it is necessary to secure a separate time or the student may not be able to meet the assigned patient. Second, we plan to develop a system to notify students of their patients' schedule. Sometimes students were unaware of their patients' hospital visits or changes in the patients' schedule. With the introduction of the notification system, we believe that these shortcomings will be improved.
There are several limitations of this study. First, this study does not have a case-control design between the LIC and the rotational clerkship, and we compared parallel experience among students. Second, the results are based on self-reporting. Third, our blended LIC is a kind of complementary clerkship, in which relatively few patients are encountered. However, the traditional rotation clerkship compensates for these shortcomings because patient encounters are done at the same time. It is also complemented by active discussion classes and enhanced feedback. It is important for students to learn competencies that are difficult to experience in rotational clerkships. Thus, this LIC focused on the two core competencies of continuity of the patient's medical experience and the concept of patient-centered care.
Ongoing changes are needed in medical education to accompany changes in the medical environment. The need for patient-centered care has been causing changes, such as in-depth consultations in the outpatient clinic.
17 Traditional block rotation clerkships, in which students experience patients in a fragmented way with a focus on the disease, have many limitations. The patient-centered LIC had a positive effect on students' experience of continuity of care and patient-centered care. Nonetheless, some areas for improvement remain.
The patient-centered LIC was helpful to understand and acquire the continuity of care compared to the rotational clerkship.
Go to :

ACKNOWLEDGMENTS
The authors acknowledge all students, professors, and teaching assistants at Seoul National University College of Medicine that participated in this study.
Go to :

Notes
Go to :

References
1. Hirsh DA, Ogur B, Thibault GE, Cox M. “Continuity” as an organizing principle for clinical education reform. N Engl J Med. 2007; 356(8):858–866. PMID:
17314348.

2. Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J Korean Med Sci. 2010; 25(9):1259–1271. PMID:
20808667.

3. World Health Organization. People-centered health care: technical papers: international symposium on people-centered health care: reorienting health systems in the 21st century, the Tokyo International Forum, 25 November 2007. Manila: WHO Regional Office for the Western Pacific;2008.
4. Epstein RM, Fiscella K, Lesser CS, Stange KC. Why the nation needs a policy push on patient-centered health care. Health Aff (Millwood). 2010; 29(8):1489–1495. PMID:
20679652.

5. Merlino JI, Kestranek C, Bokar D, Sun Z, Nissen SE, Longworth DL. HCAHPS survey results: impact of severity of illness on hospitals' performance on HCAHPS survey results. J Patient Exp. 2014; 1(2):16–21. PMID:
28725804.

6. Hwang SM, Lee JJ, Jang JS, Gim GH, Kim MC, Lim SY. Patient preference and satisfaction with their involvement in the selection of an anesthetic method for surgery. J Korean Med Sci. 2014; 29(2):287–291. PMID:
24550660.

8. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med. 2006; 355(13):1339–1344. PMID:
17005951.

9. Im SJ. Strategies for effective teaching in clinical clerkship. Hanyang Med Rev. 2012; 32(1):51–58.

10. Yang E, Suh DJ, Lee Y, Lee S, Kim S, Lee E, et al. Status of clerkship education and its evaluation in Korean medical schools. Korean J Med Educ. 2007; 19(2):111–121.

11. Worley P, Couper I, Strasser R, Graves L, Cummings BA, Woodman R, et al. A typology of longitudinal integrated clerkships. Med Educ. 2016; 50(9):922–932. PMID:
27562892.

13. Yoon HB, Moon SH, Myung SJ, Park JB, Park WB. Pilot study results of a longitudinal integrated clerkship in a single institution. Korean Med Educ Rev. 2018; 20(1):15–19.
14. Bleasel J, Burgess A, Weeks R, Haq I. Feedback using an ePortfolio for medicine long cases: quality not quantity. BMC Med Educ. 2016; 16(1):278. PMID:
27769240.

15. Alliance for Clinical Education, Poncelet A, Hirsh D. Longitudinal Integrated Clerkships: Principles, Outcomes, Practical Tools, and Future Directions. North Syracuse, NY: Gegensatz Press;2016.
16. Osman N, Atalay A, Ghosh A, Saravanan Y, Shagrin B, Singh T, et al. Structuring medical education for workforce transformation: continuity, symbiosis and longitudinal integrated clerkships. Educ Sci. 2017; 7(2):58.

17. Sohn KH, Nam S, Joo J, Kwon YJ, Yim JJ. Patient-centeredness during in-depth consultation in the outpatient clinic of a tertiary hospital in Korea: paradigm shift from disease to patient. J Korean Med Sci. 2019; 34(15):e119. PMID:
31001936.

Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download