1. Bauer TW, Parvizi J, Kobayashi N, Krebs V. Diagnosis of periprosthetic infection. J Bone Joint Surg Am. 2006; 88(4):869–882. PMID:
16595481.

2. Parvizi J, Zmistowski B, Adeli B. Periprosthetic joint infection: treatment options. Orthopedics. 2010; 33(9):659. PMID:
20839679.

3. Pina M, Gaukhman AD, Hayden B, Smith EL. Three concurrent periprosthetic joint infections: a case report and literature review. Hip Pelvis. 2019; 31(1):57–62. PMID:
30899716.

4. Lamagni T.Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother. 2014; 69(Suppl 1):i5–10. PMID:
25135091.

5. Tan TL, Kheir MM, Rondon AJ, Parvizi J, George J, Higuera CA, et al. Determining the role and duration of the “antibiotic holiday” period in periprosthetic joint infection. J Arthroplasty. 2018; 33(9):2976–2980. PMID:
29866503.

6. Spivey JC, Guild GN 3rd, Scuderi GR. Use of articulating spacer technique in revision total knee arthroplasty complicated by sepsis: a systematic meta-analysis. Orthopedics. 2017; 40(4):212–220. PMID:
28195606.

7. Wang Q, Goswami K, Kuo FC, Xu C, Tan TL, Parvizi J. Two-stage exchange arthroplasty for periprosthetic joint infection: the rate and reason for the attrition after the first stage. J Arthroplasty. 2019; 34(11):2749–2756. PMID:
31285090.

8. Park HJ, Kim HJ, Kim S, Kim SM, Mun JU, Kim J, et al. Safety of temporary use of recycled autoclaved femoral components in infected total knee arthroplasty: confirming sterility using a sonication method. Clin Orthop Surg. 2018; 10(4):427–432. PMID:
30505410.

9. Huddleston JI, Wang Y, Uquillas C, Herndon JH, Maloney WJ. Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res. 2012; 470(2):490–496. PMID:
21796477.

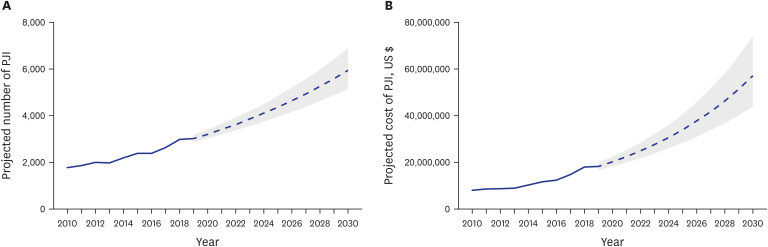
10. O'Toole P, Maltenfort MG, Chen AF, Parvizi J. Projected increase in periprosthetic joint infections secondary to rise in diabetes and obesity. J Arthroplasty. 2016; 31(1):7–10.
11. Kurtz SM, Lau EC, Son MS, Chang ET, Zimmerli W, Parvizi J. Are we winning or losing the battle with periprosthetic joint infection: trends in periprosthetic joint infection and mortality risk for the medicare population. J Arthroplasty. 2018; 33(10):3238–3245. PMID:
29914821.

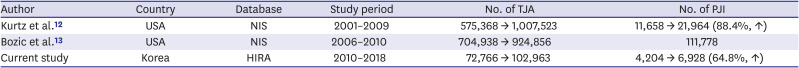
12. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012; 27(8 Suppl):61–65.e1. PMID:
22554729.

13. Bozic KJ, Kamath AF, Ong K, Lau E, Kurtz S, Chan V, et al. Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res. 2015; 473(6):2131–2138. PMID:
25467789.

14. Roth VR, Mitchell R, Vachon J, Alexandre S, Amaratunga K, Smith S, et al. Periprosthetic infection following primary hip and knee arthroplasty: the impact of limiting the postoperative surveillance period. Infect Control Hosp Epidemiol. 2017; 38(2):147–153. PMID:
27834161.

15. Bourne RB, Maloney WJ, Wright JG. An AOA critical issue. The outcome of the outcomes movement. J Bone Joint Surg Am. 2004; 86(3):633–640. PMID:
14996894.

16. Yoon PW, Lee YK, Ahn J, Jang EJ, Kim Y, Kwak HS, et al. Epidemiology of hip replacements in Korea from 2007 to 2011. J Korean Med Sci. 2014; 29(6):852–858. PMID:
24932089.

17. Akindolire J, Morcos MW, Marsh JD, Howard JL, Lanting BA, Vasarhelyi EM. The economic impact of periprosthetic infection in total hip arthroplasty. Can J Surg. 2020; 63(1):E52–6. PMID:
31995337.

18. Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008; 466(7):1710–1715. PMID:
18421542.

19. Perfetti DC, Boylan MR, Naziri Q, Paulino CB, Kurtz SM, Mont MA. Have periprosthetic hip infection rates plateaued? J Arthroplasty. 2017; 32(7):2244–2247. PMID:
28318862.

20. Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014; 472(2):464–470. PMID:
23801061.

21. Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014; 472(1):181–187. PMID:
23645339.

22. Garrido-Gómez J, Arrabal-Polo MA, Girón-Prieto MS, Cabello-Salas J, Torres-Barroso J, Parra-Ruiz J. Descriptive analysis of the economic costs of periprosthetic joint infection of the knee for the public health system of Andalusia. J Arthroplasty. 2013; 28(7):1057–1060. PMID:
23523484.

23. Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J Bone Joint Surg Br. 2012; 94(5):619–623. PMID:
22529080.
24. Wu C, Qu X, Liu F, Li H, Mao Y, Zhu Z. Risk factors for periprosthetic joint infection after total hip arthroplasty and total knee arthroplasty in Chinese patients. PLoS One. 2014; 9(4):e95300. PMID:
24748009.

25. Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008; 23(7):984–991. PMID:
18534466.

26. Hackett DJ, Rothenberg AC, Chen AF, Gutowski C, Jaekel D, Tomek IM, et al. The economic significance of orthopaedic infections. J Am Acad Orthop Surg. 2015; 23(Suppl):S1–S7. PMID:
25808964.

27. Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, et al. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010; 10(1):230. PMID:
20438644.

28. Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM. Fasting serum glucose level and cancer risk in Korean men and women. JAMA. 2005; 293(2):194–202. PMID:
15644546.

29. Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther. 2009; 31(6):1309–1320. PMID:
19695396.

30. Lee YK, Byun DW, Jung SM, Kwon HY, Kim HY, Kim SH, et al. Bisphosphonates use and risk of subtrochanteric and diaphyseal femur fractures in Korea: results from the National Claim Registry. Calcif Tissue Int. 2019; 104(3):313–319. PMID:
30446771.

31. Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013; 24(2):707–711. PMID:
22618268.

32. Park SM, Ahn SH, Kim HY, Jang S, Ha YC, Lee YK, et al. Incidence and mortality of subsequent vertebral fractures: analysis of claims data of the Korea National Health Insurance Service from 2007 to 2016. Spine J. 2020; 20(2):225–233. PMID:
31589928.

33. Brochin RL, Phan K, Poeran J, Zubizarreta N, Galatz LM, Moucha CS. Trends in periprosthetic hip infection and associated costs: a population-based study assessing the impact of hospital factors using national data. J Arthroplasty. 2018; 33(7):Suppl. S233–S238. PMID:
29573912.

34. Brochin R, Poeran J, Vig KS, Keswani A, Zubizarreta N, Galatz LM, et al. Trends in periprosthetic knee infection and associated costs: a population-based study using national data. J Knee Surg. Forthcoming 2020. DOI:
10.1055/s-0040-1701516.

35. Korea National Statistical Office. Updated 2020. Accessed September 19, 2020.
http://www.kosis.kr/.
36. Kamath AF, Ong KL, Lau E, Chan V, Vail TP, Rubash HE, et al. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015; 30(9):1492–1497. PMID:
25865815.

37. Xu C, Goswami K, Li WT, Tan TL, Yayac M, Wang SH, et al. Is treatment of periprosthetic joint infection improving over time? J Arthroplasty. 2020; 35(6):1696–1702.e1. PMID:
32192834.

38. Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J. What are the causes of revision total knee arthroplasty in Japan? Clin Orthop Relat Res. 2013; 471(5):1533–1538. PMID:
23385774.

39. Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018; 33(5):1309–1314.e2. PMID:
29551303.





 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download