This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Following the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China, a total of 637 patients had been diagnosed with the disease in Seoul as of May 2, 2020. Our study aimed to describe the impact of the 3T strategies (preemptive testing, prompt tracing and proper treatment) on the epidemiological characteristics of COVID-19 in Seoul.
Methods
The descriptive and explanatory analysis was carried out on critical indicators such as epidemiological characteristics and key duration of patient status change from January 24 to May 2 in Seoul before and after preemptive testing for patients under investigation associated with COVID-19 clusters.
Results
Preemptive testing increased the positive test rate (3.9% to 4.2%), an asymptomatic case at diagnosis (16.9% to 30.6%), and reduced the time from symptom onset to quarantine (4.0 to 3.0 days). Prompt tracing decreased unknown sources of infection (6.9% to 2.8%), the mean number of contacts (32.2 to 23.6), and the time-varying reproduction number R(t) (1.3 to 0.6). With proper treatment, only 2 cases of mortality occurred, resulting in a fatality rate of just 0.3%.
Conclusion
In the first wave of the COVID-19 pandemic lasting 100 days, the effect of the 3T strategies flattened the curve and decreased the time during which infected individuals were contagious, thereby lowering the R(t) below 1 in Seoul.
Go to :

Graphical Abstract
Go to :

Keywords: SARS-CoV-2, COVID-19, Outbreak, Response, Seoul, Korea
INTRODUCTION
Since the first patient was identified in Wuhan, China, in December 2019, coronavirus disease 2019 (COVID-19) has spread rapidly worldwide.
1 As of May 2, 2020, with the approximate fatality rate of 7.0%, 3.2 million cases were confirmed with COVID-19 globally.
2 In Korea, the first patient was diagnosed on January 20. As of May 2, a total of 10,799 patients had been identified, with a fatality rate of 2.4% (4.94 case fatalities per million).
At the beginning of the epidemic, the Seoul Metropolitan Government (SMG) established the testing-tracing-treatment (3T) strategy in public health, in collaboration with Korea Centers for Disease Control and Prevention (KCDC), currently renamed as Korea Disease Control and Prevention Agency (KDCA). For widespread testing, the KCDC provided the guideline to open COVID-19 screening stations in isolated areas within health centers, medical institutions, drive-through sites, and glove-wall testing booths in order to identify carriers at the earliest possible to detect suspected case showing symptoms of COVID-19 such as cough or fever or patients under investigation. In addition to screening stations testing, preemptive testing is defined as a strategy of conducting complete testing on all cluster-associated patients under investigation who are working, living, or visiting in the confined environment where the cluster was found with an unknown source of infection including asymptomatic cases. Prompt tracing strategy is to prevent secondary and tertiary infections in the community and across the country, as those who were contacts of confirmed patients were immediately identified and notified to undertake testing.
To prevent further community spread of COVID-19, the SMG COVID-19 Rapid Response team (SCoRR team) was formed, including epidemiologists, SMG judicial police (SMG Special Judicial Police Bureau for Public Safety), and administrative experts such as public health officers, which support epidemiological investigation and operated countermeasures in case of hospital infections or group outbreaks due to unknown source of origin.
3 The SCoRR team not only relied on subjective in-depth interviews for contact tracing but also objective data, such as global positioning system data, credit card transaction logs, drug utilization review, and closed-circuit television. Lastly, to ensure appropriate and timely treatment, when the test result is positive, the confirmed patient is promptly transferred to a medical institution equipped with a negative pressure room to start early treatment considering severity. In addition, firstly community treatment centers were established for patients with mild illness or no symptoms, and municipal hospital containment wards were set up to treat severely ill patients with COVID-19. To this end, SMG secured 996 beds of negative pressure treatment with cooperation of hospitalization and 217 beds in Taereung community treatment center.
3
This study was conducted with two objectives. First, we aimed to describe the epidemiological characteristics of COVID-19 in Seoul as the background of the application of 3T strategies, consisting of preemptive testing, prompt tracing, and proper treatment. Second, we estimated key epidemiologic indexes after the implementation of the 3T strategies, particularly focusing on the two components of testing part of the 3T strategy that were essential for flattening the epidemic curve in Seoul.
Go to :

METHODS
Classification of 3 time periods; the 1st 100 days in Seoul
We conducted a descriptive and explanatory analysis of COVID-19 patients during the first 100 days since the first case in Seoul (from January 24 to May 2) by using 2 testing strategies. These strategies involved the screening station testing and preemptive testing started by the SMG. Screening station testing is defined as a testing on suspected case showing symptoms of COVID-19 such as cough or fever or patients under investigation. As of April 8, 2020, 638 public health centers and screening stations at medical institutions were operated in Korea.
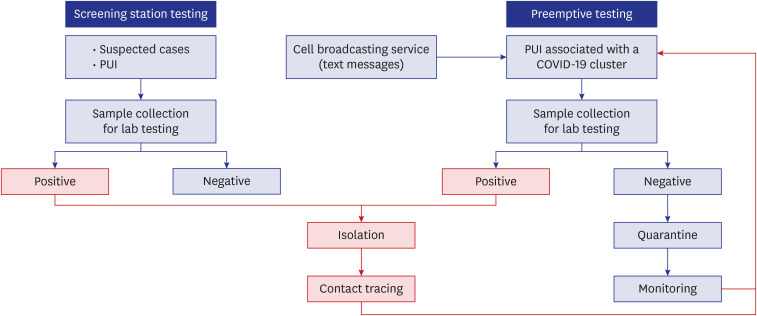
4 Preemptive testing is defined as a strategy of conducting complete testing on all cluster-associated patients under investigation who are working, living, or visiting in the confined environment where the cluster was found with an unknown source of infection including asymptomatic cases. A flowchart outlining the 2 testing strategies of the SMG is shown in
Fig. 1.
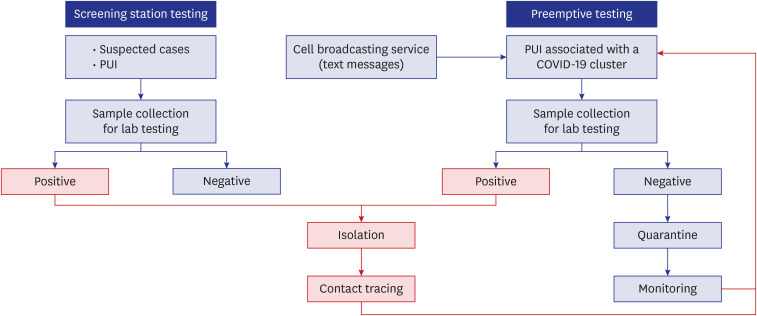 | Fig. 1
COVID-19 response process and platforms, Seoul, Korea.
COVID-19 = coronavirus disease 2019, PUI = patients under investigation.

|
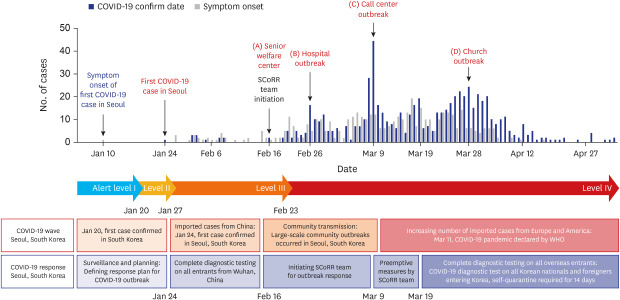
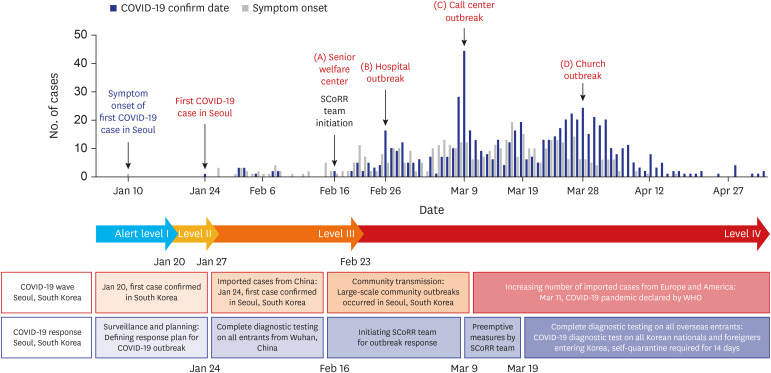
To describe the epidemiological features of the COVID-19 pandemic and the corresponding response, we divided the first 100 days into three periods according to the dates of important events that could have affected viral transmission in Seoul. In the first phase, the patients mostly arrived from Wuhan, China, and were confirmed as COVID-19 positive at the Incheon Airport National Quarantine Station. The second phase started with a 36-year-old Korean male diagnosed with COVID-19 at a senior welfare center (A) on February 16; he was the first patient with community-acquired COVID-19 and no travel history to Wuhan, China. In this phase, several cluster outbreaks occurred at a senior welfare center (A), hospital (B), call center (C), and church (D). The third phase started on March 11 with the WHO declaration of a global pandemic. During this phase, COVID-19 patients were overseas entrees, including students studying abroad, immigrants, and returning travelers. To prevent community transmission by these carriers, the SMG is currently conducting mandatory COVID-19 testing for overseas entrants and returnees (
Fig. 2).
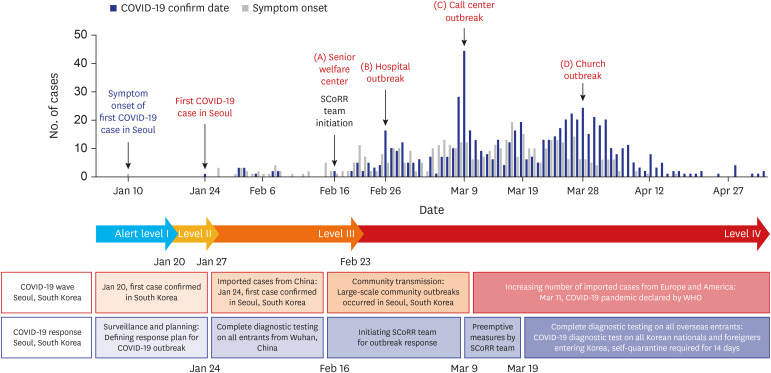 | Fig. 2
Pandemic curve and COVID-19 response, Seoul, Korea.
COVID-19 = coronavirus disease 2019, SCoRR team = Seoul Metropolitan Government COVID-19 Rapid Response team, WHO = World Health Organization.

|
Data source
When a case was confirmed, epidemiologists interviewed the patient to track the route of infection and paths based on the preliminary report by municipal health officials. The contacts identified on the path were verified through the use of objective big data.
5 Data were collected through this process for 100 days from January 24 to May 2, 2020. Every case was given a unique identification code, so that there were no overlapping data. All patients were included in the data set; neither sampling nor eligibility criteria were used.
Variables and analysis
We conducted an analysis of the epidemiological characteristics of the COVID-19 outbreak in Seoul based on a total of 637 in-depth epidemiological surveys from January 24 to May 2. We investigated the 3T strategy application of three phases (entry from Wuhan, China – community transmission –overseas inflow) of the COVID-19 pandemic in Seoul. In addition to the 3T strategy, preemptive testing was implemented by the SMG for patients associated with COVID-19 clusters beginning on March 9, with the start of an outbreak in a call center (C), a closed office environment with an unknown initial path of infection. Key indicators such as sex, age group, symptoms, and source of infection were compared using χ2 tests, fisher's exact tests, and Mann-Whitney U tests according to variable distribution. The severity of COVID-19 was measured using a case fatality rate. The distribution of patients according to the presumed source of infection was identified, i.e., spread between families, association with clusters such as churches and call centers, international travel history, and history of multiuse facility visits. The current patient status was classified into 4 groups: hospital admission, readmission, community treatment center, and discharged.
Four key time-to-event intervals were calculated and evaluated using Student's t-tests: 1) symptom onset to quarantine of travel-associated patients, 2) symptom onset to quarantine of non-travel-associated patients, 3) symptom onset to hospital admission of travel-associated patients, and 4) hospital admission to discharge. The effect of the SMG 3T strategy was evaluated by analyzing the changes in intervals mentioned above. Analysis of COVID-19 confirmed cases' characteristics were conducted with using SAS 9.4 software (SAS Institute Inc., Cary, NC, USA) and reproduction number were performed by R studio 1.3 (RStudio, PBC, Boston, MA, USA).
Ethics statement
This study was reviewed and approved by the Institutional Review Board of Seoul Metropolitan Government-Seoul National University Boramae Medical Center (approval No. 20200403/07-2020-12/043). The need of obtaining the informed consent was waived by the board.
Go to :

RESULTS
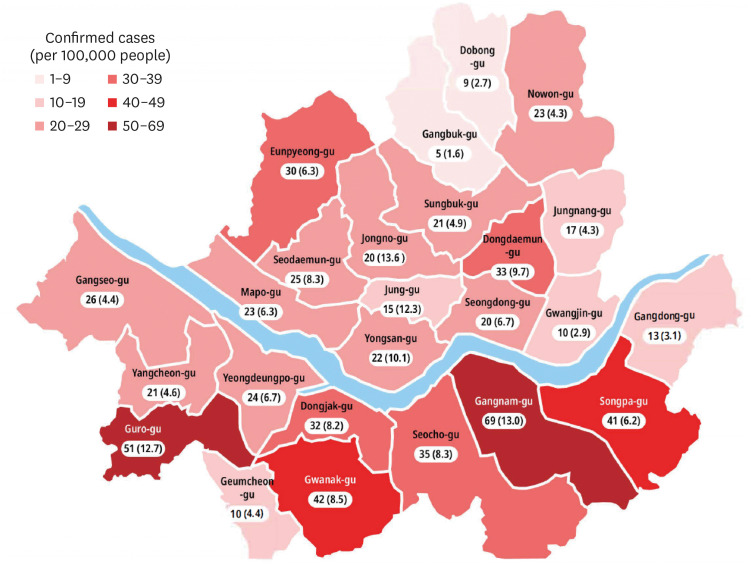
As of May 2, 2020, 637 of 16,176 tested individuals were diagnosed with COVID-19 and all confirmed cases were included in this analysis. Among 25 municipal districts in Seoul, Gangnam-gu had the highest number of confirmed cases (69 confirmed cases, 13.0 cases per 100,000) (
Fig. 3).
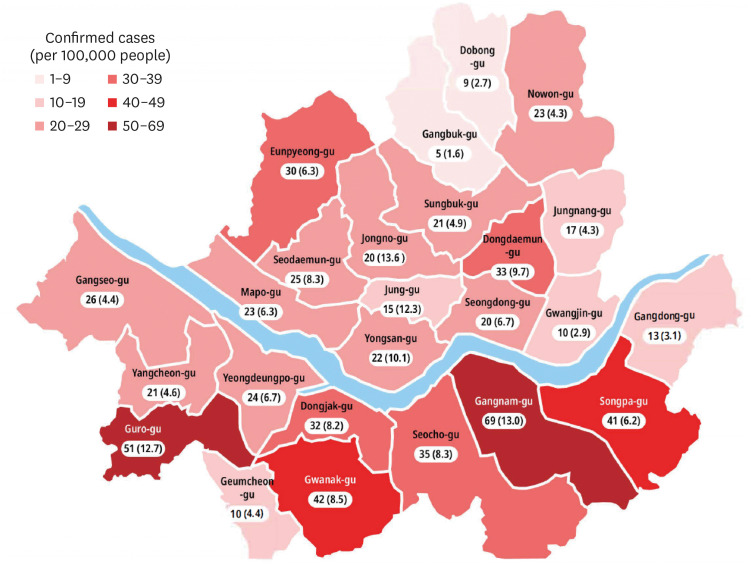 | Fig. 3
Total number of COVID-19 cases in each district, Seoul, Korea.
COVID-19 = coronavirus disease 2019.

|
Eight employees at a call center (C) were confirmed to be COVID-19 positive on March 9, 2020,
6 and the SMG immediately dispatched the SCoRR team to carry out an immediate lockdown of the building and preemptive testing. Even for people with negative test results, self-quarantine and daily monitoring for symptoms were conducted to prevent the transmission of COVID-19 within the community during the maximum incubation period of 14 days (
Fig. 1). As the SCoRR team had responded with rapid deployment since March 9, we were able to compare several epidemiological features of patients before and after the implementation of this countermeasure.
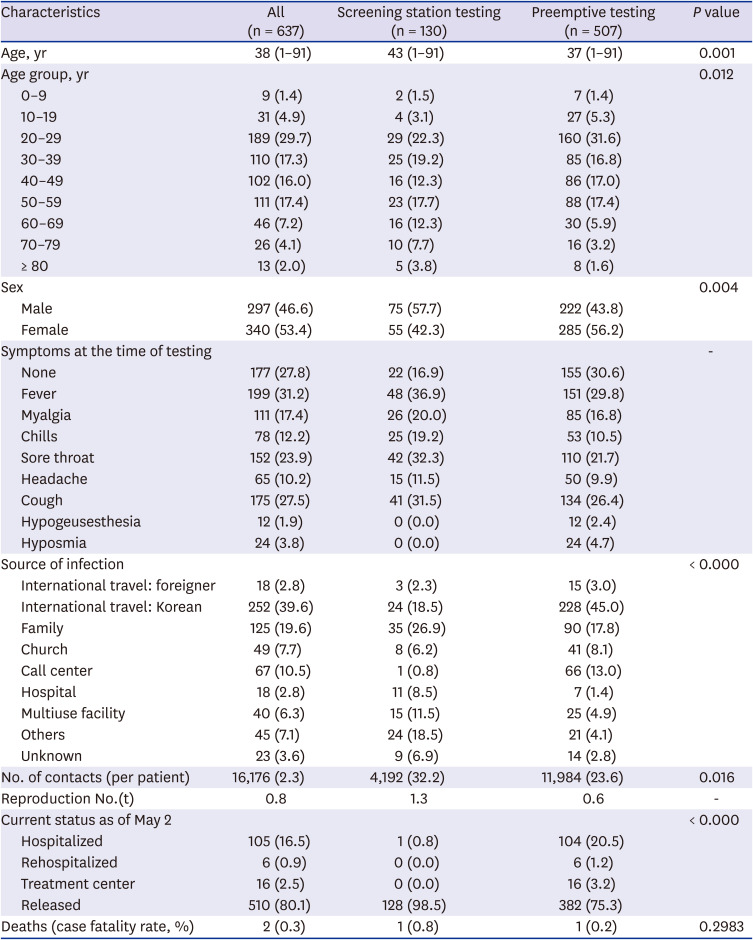
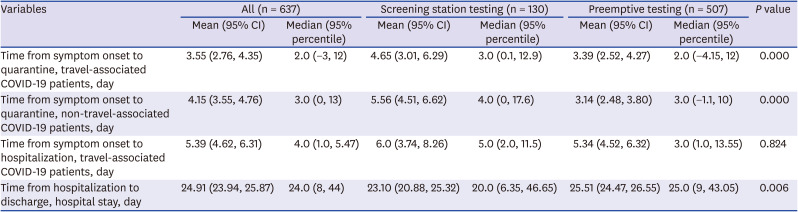
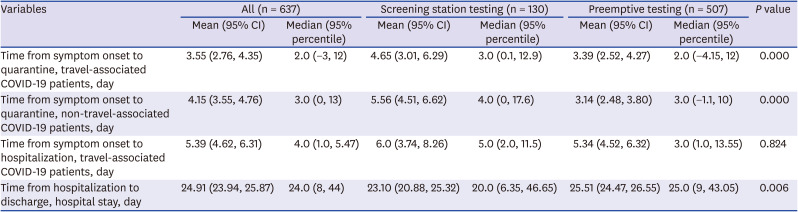
The baseline characteristics of the confirmed cases (n = 637) are shown in
Table 1. Most cases (n = 507, 79.6%) were diagnosed after preemptive testing. The median age of the 637 patients was 38.0 years (range 1–91 years); the median age for screening station testing was 43.0 years and that for preemptive testing was 37.0 years. Most cases were in the 20- to 29-year group, and by implementing preemptive testing, the proportion of cases in this group increased (160, 31.6%). Among cases, 57.7% were male in screening station testing, although the proportion of females increased after preemptive testing (285, 56.2%). Observed symptoms included common symptoms of COVID-19, such as fever, myalgia, sore throat, and cough. Unusual symptoms were also observed, such as hypogeusesthesia and hyposmia. Identification of asymptomatic patients (155, 30.6%) increased with preemptive testing.
Table 1
Characteristics of laboratory-confirmed COVID-19 cases in Seoul, Korea stratified by 2 testing strategies
|
Characteristics |
All (n = 637) |
Screening station testing (n = 130) |
Preemptive testing (n = 507) |
P value |
|
Age, yr |
38 (1–91) |
43 (1–91) |
37 (1–91) |
0.001 |
|
Age group, yr |
|
|
|
0.012 |
|
0–9 |
9 (1.4) |
2 (1.5) |
7 (1.4) |
|
10–19 |
31 (4.9) |
4 (3.1) |
27 (5.3) |
|
20–29 |
189 (29.7) |
29 (22.3) |
160 (31.6) |
|
30–39 |
110 (17.3) |
25 (19.2) |
85 (16.8) |
|
40–49 |
102 (16.0) |
16 (12.3) |
86 (17.0) |
|
50–59 |
111 (17.4) |
23 (17.7) |
88 (17.4) |
|
60–69 |
46 (7.2) |
16 (12.3) |
30 (5.9) |
|
70–79 |
26 (4.1) |
10 (7.7) |
16 (3.2) |
|
≥ 80 |
13 (2.0) |
5 (3.8) |
8 (1.6) |
|
Sex |
|
|
|
0.004 |
|
Male |
297 (46.6) |
75 (57.7) |
222 (43.8) |
|
Female |
340 (53.4) |
55 (42.3) |
285 (56.2) |
|
Symptoms at the time of testing |
|
|
|
- |
|
None |
177 (27.8) |
22 (16.9) |
155 (30.6) |
|
Fever |
199 (31.2) |
48 (36.9) |
151 (29.8) |
|
Myalgia |
111 (17.4) |
26 (20.0) |
85 (16.8) |
|
Chills |
78 (12.2) |
25 (19.2) |
53 (10.5) |
|
Sore throat |
152 (23.9) |
42 (32.3) |
110 (21.7) |
|
Headache |
65 (10.2) |
15 (11.5) |
50 (9.9) |
|
Cough |
175 (27.5) |
41 (31.5) |
134 (26.4) |
|
Hypogeusesthesia |
12 (1.9) |
0 (0.0) |
12 (2.4) |
|
Hyposmia |
24 (3.8) |
0 (0.0) |
24 (4.7) |
|
Source of infection |
|
|
|
< 0.000 |
|
International travel: foreigner |
18 (2.8) |
3 (2.3) |
15 (3.0) |
|
International travel: Korean |
252 (39.6) |
24 (18.5) |
228 (45.0) |
|
Family |
125 (19.6) |
35 (26.9) |
90 (17.8) |
|
Church |
49 (7.7) |
8 (6.2) |
41 (8.1) |
|
Call center |
67 (10.5) |
1 (0.8) |
66 (13.0) |
|
Hospital |
18 (2.8) |
11 (8.5) |
7 (1.4) |
|
Multiuse facility |
40 (6.3) |
15 (11.5) |
25 (4.9) |
|
Others |
45 (7.1) |
24 (18.5) |
21 (4.1) |
|
Unknown |
23 (3.6) |
9 (6.9) |
14 (2.8) |
|
No. of contacts (per patient) |
16,176 (2.3) |
4,192 (32.2) |
11,984 (23.6) |
0.016 |
|
Reproduction No.(t) |
0.8 |
1.3 |
0.6 |
- |
|
Current status as of May 2 |
|
|
|
< 0.000 |
|
Hospitalized |
105 (16.5) |
1 (0.8) |
104 (20.5) |
|
Rehospitalized |
6 (0.9) |
0 (0.0) |
6 (1.2) |
|
Treatment center |
16 (2.5) |
0 (0.0) |
16 (3.2) |
|
Released |
510 (80.1) |
128 (98.5) |
382 (75.3) |
|
Deaths (case fatality rate, %) |
2 (0.3) |
1 (0.8) |
1 (0.2) |
0.2983 |

Seoul had a low fatality rate (0.3%, 2 patients) for a metropolitan area with 1/5 of the total population of Korea, compared to the national fatality rate of 2.4% (256 patients). The recent proportion of cases with a travel history was 18.5% (24/130 patients) before preemptive testing, but it increased to 45.0% (228/507 patients) after the implementation of preemptive testing during the third phase following a global pandemic declaration, presented in
Fig. 2. Regarding family transmission, the incidence decreased from 26.9% (35/130 patients) using screening station testing to 17.8% (90/507 patients) using preemptive testing.
The number of cases with an unknown transmission route was reduced by more than half from 6.9% (9/130 patients) to 2.8% (14/507 patients) after preemptive testing. By May 2, 105 patients (16.5%) were hospitalized, 510 (80.1%) discharged, 6 (0.9%) rehospitalized after diagnosis again, and 16 patients admitted in the community treatment center.
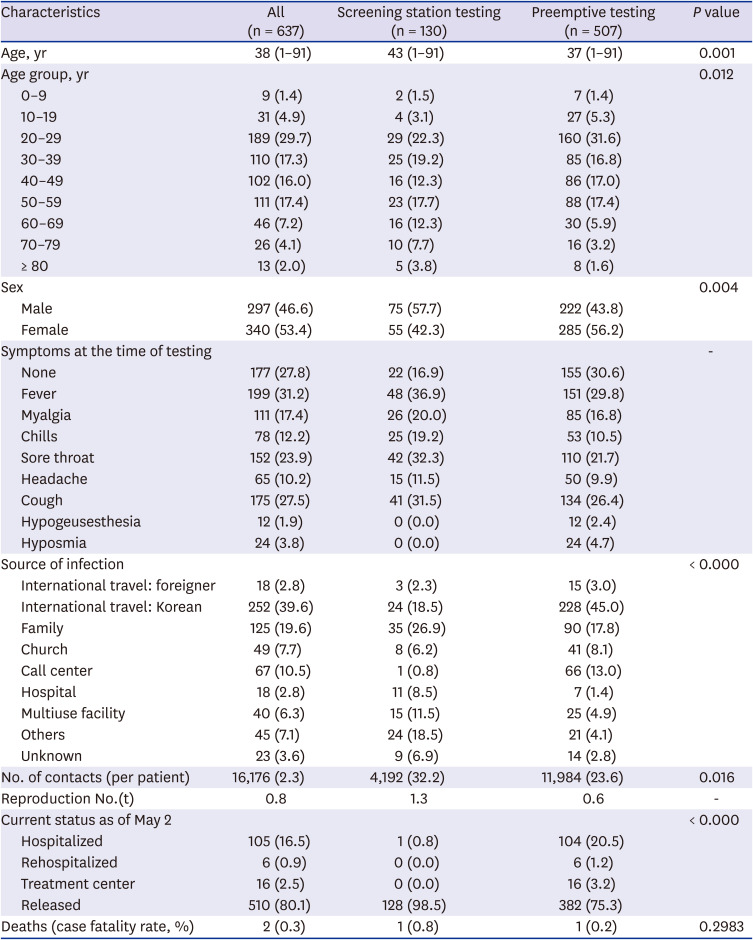
Regarding symptomatic patients with international travel history, the average time from the first symptom to quarantine was 4.65 days (95% confidence interval, 3.01–6.29) on screening station testing, which significantly decreased to 3.39 days (2.52–4.27) on preemptive testing (
P < 0.001). People with no travel history had a substantial difference: 5.56 days (4.51–6.62) on screening station testing to 3.14 days (2.48–3.80) on preemptive testing (
P < 0.001). The average hospital stay was 23.10 days from hospitalization to discharge (20.88–25.32), which increased to 25.51 days (24.47–26.55) with preemptive testing (
Table 2).
Table 2
Key time-to-event intervals for laboratory-confirmed COVID-19 cases stratified by the 2 testing strategies
|
Variables |
All (n = 637) |
Screening station testing (n = 130) |
Preemptive testing (n = 507) |
P value |
|
Mean (95% CI) |
Median (95% percentile) |
Mean (95% CI) |
Median (95% percentile) |
Mean (95% CI) |
Median (95% percentile) |
|
Time from symptom onset to quarantine, travel-associated COVID-19 patients, day |
3.55 (2.76, 4.35) |
2.0 (−3, 12) |
4.65 (3.01, 6.29) |
3.0 (0.1, 12.9) |
3.39 (2.52, 4.27) |
2.0 (−4.15, 12) |
0.000 |
|
Time from symptom onset to quarantine, non-travel-associated COVID-19 patients, day |
4.15 (3.55, 4.76) |
3.0 (0, 13) |
5.56 (4.51, 6.62) |
4.0 (0, 17.6) |
3.14 (2.48, 3.80) |
3.0 (−1.1, 10) |
0.000 |
|
Time from symptom onset to hospitalization, travel-associated COVID-19 patients, day |
5.39 (4.62, 6.31) |
4.0 (1.0, 5.47) |
6.0 (3.74, 8.26) |
5.0 (2.0, 11.5) |
5.34 (4.52, 6.32) |
3.0 (1.0, 13.55) |
0.824 |
|
Time from hospitalization to discharge, hospital stay, day |
24.91 (23.94, 25.87) |
24.0 (8, 44) |
23.10 (20.88, 25.32) |
20.0 (6.35, 46.65) |
25.51 (24.47, 26.55) |
25.0 (9, 43.05) |
0.006 |

Go to :

DISCUSSION
An assessment of the transmission dynamics and epidemiological characteristics of the COVID-19 outbreak in Seoul was conducted in this study. Findings suggest that Seoul has developed key strategies to interrupt transmission chains of COVID-19, such as preemptive testing, isolation of cases, quarantine and strict restrictions of contacts, and providing proper treatments.
Preemptive testing coverage can be assessed by the total number of tests, the positivity rate, and the asymptomatic rate. Through aggressive large-scale testing and easy access to screening sites, the total number of tests administered in Seoul was 116,435, with a positive test rate of 0.54%. This figure increased slightly after preemptive testing was implemented (from 0.48% to 0.57%). The time from symptom onset to quarantine (median, days) decreased from 4.0 to 3.0 days. This reduction is consistent with the time required from symptom onset to quarantine (from 4.4 to 2.6 days) reported in a Chinese study, driving the time-varying reproduction number R(t) below 1.
7 Moreover, the rate of identification of asymptomatic cases at diagnosis was 27.8%; after the implementation of preemptive testing, it increased significantly from 16.9% to 30.6%. By testing patients under investigation associated with a COVID-19 cluster alongside their contacts, isolating presymptomatic and asymptomatic COVID-19 patients, transmission chains have been interrupted.
The epidemiological indicators confirm that prompt tracing can be measured by the proportion of an unknown source of infection and the time-varying reproduction number R(t). Rapid investigation and testing significantly reduced the proportion of cases with an unknown source of infection from 6.9% to 2.8%. This is significant because secondary patients were managed within the quarantine network. Also, the mean number of contacts decreased from 32.2 to 23.6, and R(t) decreased from 1.3 to 0.6. Prompt tracing was conducted by the SMG SCoRR team specially trained for contact tracing; the SCoRR team participated in a transparent and rapid evaluation of the process. The effect of prompt contact tracing has decreased the number of contacts and R(t) and flattened the curve of COVID-19.
The indicator of proper treatment is the time required from the onset of symptoms to hospitalization and the case fatality rate. Compared with before the preemptive testing was implemented, after preemptive testing, the time required from the onset of symptoms to hospitalization was reduced from 5.0 to 3.0 days. In addition, the SMG operates the community treatment centers, which serve as hospitals for isolation, treatment, and disease surveillance of patients with asymptomatic and mild symptoms similar to the Fangcang shelter hospitals.
8 The appropriate distribution of medical resources according to disease severity is an essential strategy in megacities with high population densities. This strategy allows critically ill patients to receive treatment early, while early-stage patients with mild COVID-19 are not overlooked; the result is a fatality rate of 0.3% in Seoul, the lowest among all megacities worldwide.
The median age of the patients was 38.0 years; the median age was 43.0 years old before preemptive testing and 37.0 years old after the initiation of preemptive testing. Patients in their 20s accounted for the highest percentage, which increased from 22.3% to 31.6%. This is a unique characteristic of Seoul compared to other cities such as New York (where people in their 60s account for the highest)
9 and Beijing (people in their 40s).
10 The majority of these young patients traveled from abroad; this reflects the fact that the students returning from studying overseas were not overlooked and that there was widespread testing across all age groups.
Our study has several limitations. First, determining the date of symptom onset relied on patient memory at the time of diagnosis of COVID-19 although some had medical records. Thus, potential recall bias could lead to under-ascertainment of the analysis. Secondly, we reviewed the data from the first 100 days, so the current and future assessments of SMG measures may be different, and COVID-19 is still an ongoing pandemic. Nevertheless, by presenting Seoul's systems and policies, insight into second waves of the COVID-19 response strategy is provided for megacities. Further study regarding second wave will be needed.
This study describes the epidemiological features and characteristics in Seoul according to the SMG 3T strategy of preemptive testing, prompt tracing, and proper treatment. During the first 100 days of the COVID-19 pandemic, the effectiveness of the 3T strategies flattened the curve and drove R(t) below 1 through the changes in the 3T indicators, which were established at the time of the call center (C) cluster on March 9. It is particularly meaningful to show the effectiveness of preemptive measures for preventing COVID-19 transmission using epidemiological analysis of Seoul based on the unknown sources of infection, especially in group outbreaks within a confined environment.
Go to :

ACKNOWLEDGMENTS
The authors thank the 25 public health centers in Seoul for their efforts in responding to the COVID-19 outbreak.
Go to :

Notes
Go to :

References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382(8):727–733. PMID:
31978945.

3. Na BJ, Park Y, Huh IS, Kang CR, Lee J, Lee JY. Seventy-two hours, targeting time from first COVID-19 symptom onset to hospitalization. J Korean Med Sci. 2020; 35(20):e192. PMID:
32449328.

5. Park S, Choi GJ, Ko H. Information technology–based tracing strategy in response to COVID-19 in South Korea—privacy controversies. JAMA. 2020; 323(21):2129–2130. PMID:
32324202.

6. Park SY, Kim YM, Yi S, Lee S, Na BJ, Kim CB, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020; 26(8):1666–1670. PMID:
32324530.

7. Zhang J, Litvinova M, Wang W, Wang Y, Deng X, Chen X, et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect Dis. 2020; 20(7):793–802. PMID:
32247326.

8. Fang D, Pan S, Li Z, Yuan T, Jiang B, Gan D, et al. Large-scale public venues as medical emergency sites in disasters: lessons from COVID-19 and the use of Fangcang shelter hospitals in Wuhan, China. BMJ Glob Health. 2020; 5(6):e002815.

9. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020; 323(20):2052–2059. PMID:
32320003.

10. Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020; 80(4):401–406. PMID:
32112886.

Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download