Abstract
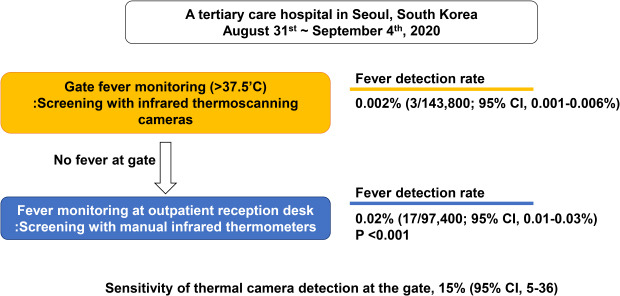
Between August 31st and September 4th 2020 in a tertiary care hospital in Seoul, the fever detection rate by infrared thermoscanning camera at the gates was 0.002% (95% confidence interval [CI], 0.001%–0.006%) and that by manual fever check at the outpatient clinics was 0.02% (95% CI, 0.01%–0.03%) (P < 0.001). The difference strongly suggests that sensitivity of the thermoscanning camera in the market must be upgraded.
Go to : 
Graphical Abstract
Go to : 
Since coronavirus disease 2019 (COVID-19) pandemic, infrared thermoscanning cameras that generate heat map images have been widely implemented in airports, shopping centers, schools, and office buildings as well as in nursing homes and hospitals to identify febrile individuals and screen for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection at the entrance. Previous studies have investigated the sensitivity of infrared thermoscanners for identifying febrile travelers in international airports during the 2009 influenza pandemic123; however, similar data in hospital settings during the COVID-19 pandemic is limited. We therefore compared the performance of infrared thermoscanning cameras with manual infrared thermometers.
This study was performed in a 2,700-bed tertiary care hospital in Seoul, Korea. This center has 8,800 healthcare workers, and receives approximately 12,000 outpatients and 300 new inpatients on a daily basis. Since January 29th, 2020, we have monitored everyone coming through the seven main entrances of the hospital building using infrared thermoscanning cameras (DPS-TC-160KP, AC&T system, Anyang, Korea). A total of 14 personnel (2 for each entrance) manned the infrared cameras. If a fever (defined as the temperature above > 37.5oC, as guided by Korea Centers for Disease Control and Prevention) was detected, additional temperature check was performed with manual infrared thermometers, and those still showing fever were prohibited from further entry or instructed to visit the screening clinic to be tested for SARS-CoV-2. Between January 29th and August 30th, the infrared thermoscanning cameras identified a total of 356 (mean ± standard deviation, 2.1 ± 2.6 per day) patients and visitors with fever.
Between August 31st and September 4th, 2020, Korea showed a sharp increase in the community spread of SARS-CoV-2 and we started to additionally screen all outpatients and their accompanying guardians using manual infrared thermometers at 21 reception desks in the outpatient clinic after the clearance of infrared thermoscanning cameras at the gates. Those showing fever with manual infrared thermometers were again screened with manual measurement of the tympanic membrane temperature. Patients or guardians with fever were instructed to go home or visit the screening clinic to be tested for SARS-CoV-2. Additional 31 nurses were needed to perform these manual fever screening at the outpatient clinics.
We retrospectively reviewed the number of patients with fever detected by infrared thermoscanning camera at the gate and by manual infrared therometers at the reception desks in the outpatient clinic. We used Poisson regression models for comparing the fever detection rate between measurement by infrared thermoscanning camera and by handheld thermometers using MedCalc Statistical Software version 18.10.2 (MedCalc Software Bvba, Sotend, Belgium).
During this period, approximately 143,800 individuals were screened at the gates and 97,400 individuals were screened at the outpatient clinics. As a result, gate screening and outpatient clinic screening identified 3 and 17 individuals with fever, respectively. Except for three individuals screened at the outpatient clinic who were instructed to go home, all other individuals with fever were screened at the on-campus clinics for SARS-CoV-2 from nasopharyngeal swabs, all of which revealed negative results. As a result, the fever detection rate by infrared thermoscanning camera at the gates was 0.002% (95% confidence interval [CI], 0.001–0.006%) and that by manual fever check at the outpatient clinics was 0.02% (95% CI, 0.01–0.03%) (P value by Poisson regression analysis < 0.001). The sensitivity of thermal camera detection at the gates was 15% (95% CI, 5–36) when using manual fever detection by handheld infrared thermometers followed by tympanic temperature measurement as the reference standard.
Infrared thermoscanners are widely used in airports, public facilities, and hospitals because their non-invasive nature allows for massive screening.2 However, infrared thermoscanners are easily influenced by the outside temperature, and previous studies during the 2009 influenza pandemic reported that the sensitivity of infrared thermoscanners for detecting influenza infection was as low as 5.8% in New Zealand1 and 6.6% in Japan.3 As such, the U.S. Food and Drug Administration (FDA) recommends using handheld infrared thermometers for fever screening and states that infrared thermoscanners should not be used as a standalone screening tool.4 In contrast, one study reported that thermal camera screening at airport gates was as sensitive as manual tympanic temperature measurement in detecting febrile arrivals.5 However, there have been limited data on the performance of infrared thermoscanner in comparison with handheld infrared thermometers in hospitals during the COVID-19 pandemic.
We found that handheld thermometers detected significantly more febrile patients than did infrared thermoscanners in a large-sized tertiary hospital. Despite its high sensitivity, manual fever screening requires additional human resources and its cost-effectiveness in each setting should be considered. It should also be noted that neither screening method can detect fever in patients who are taking antipyretic medications. Therefore, self-reported questionnaires on fever and epidemiologic links should be incorporated in screening the risk of SARS-CoV-2 infection in outpatient clinics.
In conclusion, manual fever screening detected about 10 times more patients than infrared thermoscanning camera at a hospital during the COVID-19 pandemic. We have to consider how to upgrade sensitivity of the thermoscanning camera in the market in Korea.
Notes
Funding: This study was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant No. HW20C2062).
Go to : 
References
1. Hale MJ, Hoskins RS, Baker MG. Screening for influenza A(H1N1)pdm09, Auckland International Airport, New Zealand. Emerg Infect Dis. 2012; 18(5):866–868. PMID: 22516105.

2. Nishiura H, Kamiya K. Fever screening during the influenza (H1N1-2009) pandemic at Narita International Airport, Japan. BMC Infect Dis. 2011; 11(1):111. PMID: 21539735.

3. Sakaguchi H, Tsunoda M, Wada K, Ohta H, Kawashima M, Yoshino Y, et al. Assessment of border control measures and community containment measures used in Japan during the early stages of Pandemic (H1N1) 2009. PLoS One. 2012; 7(2):e31289. PMID: 22355354.

4. Pannu J. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-international travel-related measures. Emerg Infect Dis. 2020; 26(9):2298–2299.

5. Cho KS, Yoon J. Fever screening and detection of febrile arrivals at an international airport in Korea: association among self-reported fever, infrared thermal camera scanning, and tympanic temperature. Epidemiol Health. 2014; 36:e2014004. PMID: 25045577.

Go to : 




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download