Medical diagnoses are made on the basis of history taking, the signs observed upon physical examination, and the results of laboratory or radiographic tests. Despite advancements in modern technology, history taking is still considered a key diagnostic tool.
1 Fever patterns are classified as remittent, intermittent, continuous, or relapsing.
2 Although fever pattern is not useful in differentiating the etiologies of fever, some infectious diseases have characteristic fever patterns.
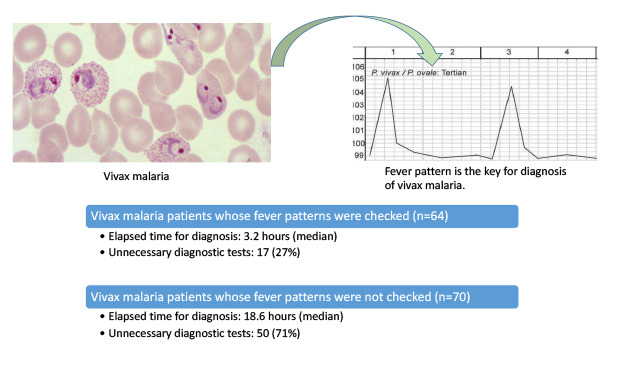
Plasmodium vivax causes fever every third day and
P. malariae, every fourth day, which is very helpful for diagnosis.
3
Fever and chills were manifested in all patients with vivax malaria in Korea.
4 Some patients had myalgia, nausea, diarrhea, and headache. Leukopenia (WBC counts < 4,000/µL) was observed in 19.9% of patients and thrombocytopenia (platelet counts < 150,000/µL) in 85.1% of patients with vivax malaria.
4 Considering the periodic pattern of fever accompanying leukopenia or thrombocytopenia, we hypothesized that vivax malaria could be highly suspected by proper history taking and by investigating the results of complete blood counts. We evaluated the impact of history taking of fever patterns on the time elapsed for diagnosis and the diagnostic testing of patients with vivax malaria.
We retrospectively reviewed the medical records of patients with vivax malaria who were admitted to three university-affiliated hospitals between January 2001 and June 2018. All the hospitals were tertiary referral centers and had 800–1,900 beds. Patients with malaria caused by other Plasmodium species were excluded from analysis, and patients with vivax malaria already diagnosed at other hospitals were also excluded. Vivax malaria was diagnosed either through thin blood smears, polymerase chain reaction (PCR), or both. When merozoites or gametocytes of P. vivax were observed on blood smears, vivax malaria was diagnosed. PCR amplification of parasite nucleic acid was used to detect Plasmodium species of P. vivax, P. malariae, and P. falciparum. All the three hospitals used the same method of malaria PCR tests. 18S ribosomal ribonucleic acid (rRNA) was used as the first target gene for identification of Plasmodium genus. If a parasite from a blood sample was determined as Plasmodium genus by 18S rRNA PCR, specific genes such as PFR364 (for P. falciparum) and malaria DHFR (dihydrofolate reductase) (for P. vivax/ovale/malariae) were used as the second target genes for differentiation of malarial species.
We investigated whether fever pattern or periodicity was recorded in the medical records of a physician who initially examined the patient. We collected data about the tests during diagnosis, the time interval between patient's visit and diagnosis, and the specialty of a physician who initially examined the patient. The time interval between the patient's visit and diagnosis was defined by elapsed time from the visit to the confirmation of diagnosis of vivax malaria by either thin blood smears or PCR.
Complete blood counts, liver function tests, and kidney function tests were considered necessary diagnostic tests. In contrast, computed tomography (CT), sonography, positron emission tomography, cerebrospinal fluid (CSF) tapping, bone marrow examination, echocardiography, and endoscopic examinations were considered as unnecessary tests. The physicians who initially interviewed the patient were classified as infectious disease (ID) specialists or other than ID specialists on the basis of their specialty.
Mann-Whitney U test was used for the comparison of the continuous variables and χ2 test was implemented for the analysis of the proportions. All P values were two-tailed, with P < 0.05 being considered statistically significant.
During the study period, a total of 186 patients were diagnosed with malaria; 52 were excluded (19 patients diagnosed with falciparum malaria and 33 patients diagnosed with vivax malaria at other hospitals initially), and 134 patients with vivax malaria were investigated.
Of 134 patients 58 (43.3%) patients were diagnosed on the basis of thin blood smears only and 76 (56.7%) patients on the basis of both thin blood smears and PCR. The results of thin blood smears and PCR were concordant in all patients who were diagnosed using both tests. Also, 116 (86.6%) patients were male and the median age of all the engaged patients was 29 years old. Out of 116 male patients, four were in military service and 46 have been discharged from military service within 1 year at the time of diagnosis. Ninety-eight patients were diagnosed at emergency rooms, 34 at outpatient clinics (33 at the department of internal medicine and 1 at the department of family medicine), and 2 at hospital wards. A total of 109 patients have visited hospitals between June and September.
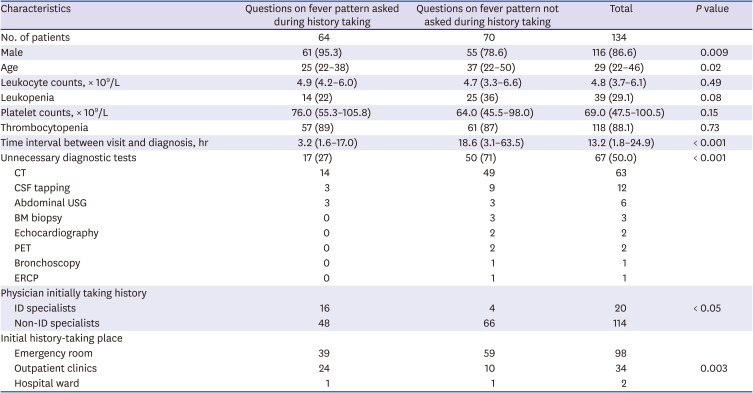
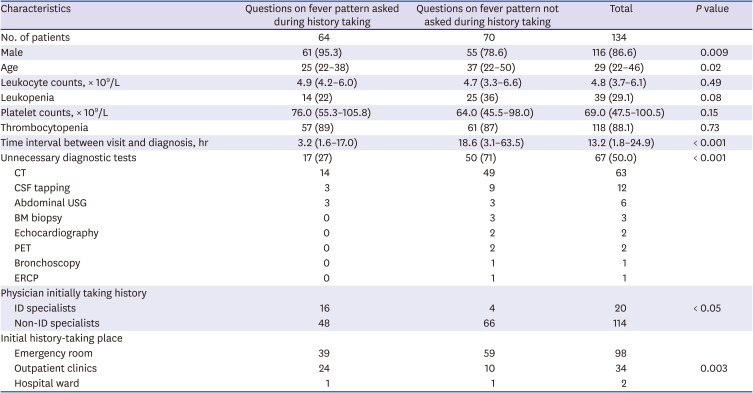
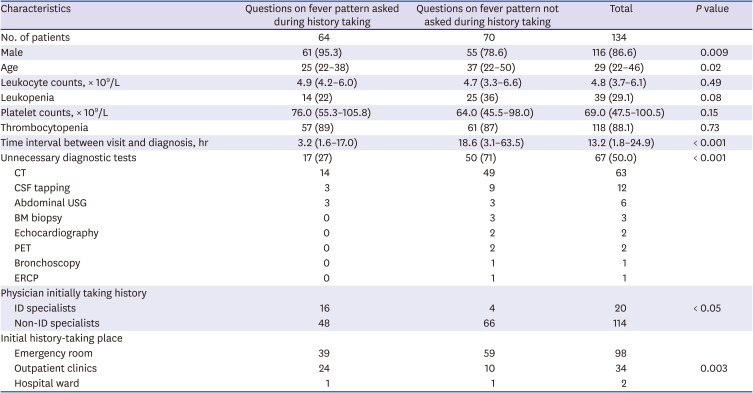
All patients had a history of fever; questions about the fever pattern or periodicity were asked in 64 patients (47.8%) and 25 (39.1%) of these 64 patients whose fever pattern was recorded had developed a fever every 48 hours. Complete blood counts were obtained for all patients; leukopenia and thrombocytopenia were observed in 39 (29.1%) and 118 (88.1%) of the 134 patients, respectively (
Table 1).
Table 1
Demographic and clinical characteristics of patients with vivax malaria according to asking a fever pattern
|
Characteristics |
Questions on fever pattern asked during history taking |
Questions on fever pattern not asked during history taking |
Total |
P value |
|
No. of patients |
64 |
70 |
134 |
|
|
Male |
61 (95.3) |
55 (78.6) |
116 (86.6) |
0.009 |
|
Age |
25 (22–38) |
37 (22–50) |
29 (22–46) |
0.02 |
|
Leukocyte counts, × 109/L |
4.9 (4.2–6.0) |
4.7 (3.3–6.6) |
4.8 (3.7–6.1) |
0.49 |
|
Leukopenia |
14 (22) |
25 (36) |
39 (29.1) |
0.08 |
|
Platelet counts, × 109/L |
76.0 (55.3–105.8) |
64.0 (45.5–98.0) |
69.0 (47.5–100.5) |
0.15 |
|
Thrombocytopenia |
57 (89) |
61 (87) |
118 (88.1) |
0.73 |
|
Time interval between visit and diagnosis, hr |
3.2 (1.6–17.0) |
18.6 (3.1–63.5) |
13.2 (1.8–24.9) |
< 0.001 |
|
Unnecessary diagnostic tests |
17 (27) |
50 (71) |
67 (50.0) |
< 0.001 |
|
CT |
14 |
49 |
63 |
|
CSF tapping |
3 |
9 |
12 |
|
Abdominal USG |
3 |
3 |
6 |
|
BM biopsy |
0 |
3 |
3 |
|
Echocardiography |
0 |
2 |
2 |
|
PET |
0 |
2 |
2 |
|
Bronchoscopy |
0 |
1 |
1 |
|
ERCP |
0 |
1 |
1 |
|
Physician initially taking history |
|
|
|
|
|
ID specialists |
16 |
4 |
20 |
< 0.05 |
|
Non-ID specialists |
48 |
66 |
114 |
|
|
Initial history-taking place |
|
|
|
|
|
Emergency room |
39 |
59 |
98 |
|
|
Outpatient clinics |
24 |
10 |
34 |
0.003 |
|
Hospital ward |
1 |
1 |
2 |
|

The median of time interval between the patient's visit and diagnosis was significantly shorter among patients who had been questioned about their fever pattern during history taking (3.2 hours vs. 18.6 hours; P < 0.001). Unnecessary diagnostic tests were conducted in 17 (27%) of 64 patients who were questioned about their fever pattern during history-taking and 50 (71%) of 70 patients who were not (P < 0.001). The most common unnecessary diagnostic test was CT (63 cases, 47.0%), followed by CSF examination (12 cases, 9.0%), abdominal ultrasonography (6 cases, 4.5%), bone marrow examination (3 cases, 2.2%), echocardiography (2 cases, 1.5%), positron emission tomography (2 cases, 1.5%), bronchoscopy (1 case, 0.7%), and endoscopic retrograde cholangiopancreatography (1 case, 0.7%).
No alternative diagnosis of fever was found in patients undergoing unnecessary diagnostic tests. Whereas twelve patients were lost to follow-up, one hundred twenty-two patients had been followed up at an outpatient clinic, and all of those patients fully recovered from their fever and leukopenia/thrombocytopenia. When ID specialists interviewed the patients initially, information on fever pattern was obtained from 16 (80%) and unnecessary tests were conducted in 2 (10%) of 20 patients. In contrast, information on fever pattern was obtained in 48 (42.1%) and unnecessary tests were conducted in 65 (57.0%) of 114 patients who were not interviewed by ID specialists initially.
A periodic fever spikes as a result of synchronization of the developmental stages of parasites in patients with vivax malaria.
3 Several previous studies have reported that fever had a low specificity for the diagnosis of malaria.
56 However only the presence of a fever or the peak temperature was investigated as an indicator of malaria, and fever pattern was not investigated in those studies. Periodic fever patterns every 48 hours are quite unique to vivax malaria.
78 We suggest that asking questions on the fever pattern or periodicity is as important as asking questions on the presence of fever.
In this study questioning patients about their fever pattern or periodicity was associated with the shorter median of time interval between the patient's visit and diagnosis (3.2 hours vs. 18.6 hours) and fewer unnecessary diagnostic tests (27% vs. 71%). If vivax malaria was not considered, hematologic malignancies or meningitis might be suspected due to cytopenia or headache. Abdominal CT and bone marrow examination were performed to exclude hematologic malignancies, and spinal tapping was used to exclude meningitis in several patients. Unnecessary testing is a waste of money; furthermore, they increase the time required to obtain an appropriate diagnosis and can be harmful to the patients. CT scans did not improve the diagnosis of vivax malaria and were a radiologic hazard to patients.
9 Spinal tapping is associated with post-dural puncture headache, and bone marrow examinations cause unnecessary discomfort and trauma to patients.
10
Appropriate medical knowledge of clinician is essential for proper history-taking. Non-ID specialists might have less knowledge about periodic fever in patients with malaria than ID specialists. In this study, ID specialists had a high suspicion of vivax malaria by history-taking and therefore order less unnecessary diagnostic tests. Among 64 patients from whom information on fever pattern was obtained, 25 (39%) had a tertian fever and 39 patients (61%) did not. Interestingly, the time delay in making a diagnosis (2.0 hours vs. 3.3 hours, respectively P = 0.38) and the proportion of unnecessary diagnostic tests (16% vs. 31%, respectively; P = 0.24) were not significantly different from those in patients from whom information on the fever pattern was obtained, regardless of the periodicity of fever. We assumed that malaria might still be suspected in 24 patients who did not have tertian fever by considering of fever combined with leukopenia/thrombocytopenia. Malaria could be diagnosed relatively easily by thin blood smears and/or PCR, and diagnostic tests for malaria might be conducted in the early period of work up in these patients. Also, it might suggest that experience and knowledge of competent doctors could be more important than history taking about fever pattern in diagnosis of vivax malaria.
With the rapid growth in new diagnostic technologies, the importance of history taking tends to be overlooked.
11 Moreover, the information from laboratory and radiographic tests can be more accurate than information obtained through history taking and physical examination. However, the proper choice of laboratory and radiographic tests depends on a differential diagnosis based on history-taking and physical examination. And appropriate history-taking depends on the depth of a physician's clinical knowledge.
In conclusion, asking questions on fever pattern during history-taking is an important diagnostic method in patients with vivax malaria and medical knowledge is required for proper history-taking despite advances in diagnostic technology.
Ethics Statement
This study was ethically approved by the Institutional Review Board (IRB) of the Seoul National University Hospial (IRB No. H-1901-009-999). The informed consent requirement was waived, since this study was retrospective, involved no interaction with patients, and was considered to be of minimal risk.
Go to :