INTRODUCTION
Humidifier disinfectant-related lung injury (HDLI) is a severe form of lung damage that only occurred in Korean individuals who were exposed to a specific humidifier disinfectant (HD). The antimicrobial biocide, polyhexamethylene guanidine phosphate, was the causative ingredient in the commercial product, and Korea banned this product in 2011. Previous study described that the symptoms of HDLI are cough, dyspnea, and occasionally fever, and the progression may be subacute or rapid, similar to acute respiratory distress syndrome (ARDS).
12
The chest multidetector computed tomography (MDCT) images indicated that HDLI is characterized by diffuse centrilobular ground-glass opacity and nodules, which spare the subpleural spaces. There are often spontaneous air leaks, such as a pneumothorax or pneumomediastinum, but no evidence of air trapping or reticular opacity. The histopathologic features typically include bronchocentric distribution of fibroinflammatory lesions, which become more pronounced over time. Epidemiological studies indicated that HDLI onset was mostly during dry seasons (when humidifiers are most used) and clustered within families.
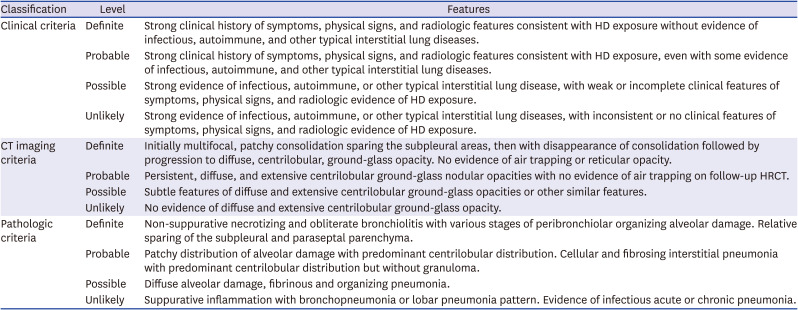
345678 Analysis of the pathologic, radiologic, and clinical features of HDLI cases and the lung histopathology of HD-exposed experimental animals led to refinement of the diagnostic criteria for HDLI in 2013 (
Table 1).
69 The first three rounds of our investigation, conducted from July 2013 to December 2015, found that 38% (n = 453) of 1,196 individuals who claimed that HD exposure was related to their diseases had confirmed HDLI. Among them, children under eight years-old accounted for 62% of cases, and pregnant women accounted for 7% of cases.
11
Table 1
Diagnostic criteria for HDLI6
|
Classification |
Level |
Features |
|
Clinical criteria |
Definite |
Strong clinical history of symptoms, physical signs, and radiologic features consistent with HD exposure without evidence of infectious, autoimmune, and other typical interstitial lung diseases. |
|
Probable |
Strong clinical history of symptoms, physical signs, and radiologic features consistent with HD exposure, even with some evidence of infectious, autoimmune, and other typical interstitial lung diseases. |
|
Possible |
Strong evidence of infectious, autoimmune, or other typical interstitial lung disease, with weak or incomplete clinical features of symptoms, physical signs, and radiologic evidence of HD exposure. |
|
Unlikely |
Strong evidence of infectious, autoimmune, or other typical interstitial lung diseases, with inconsistent or no clinical features of symptoms, physical signs, and radiologic evidence of HD exposure. |
|
CT imaging criteria |
Definite |
Initially multifocal, patchy consolidation sparing the subpleural areas, then with disappearance of consolidation followed by progression to diffuse, centrilobular, ground-glass opacity. No evidence of air trapping or reticular opacity. |
|
Probable |
Persistent, diffuse, and extensive centrilobular ground-glass nodular opacities with no evidence of air trapping on follow-up HRCT. |
|
Possible |
Subtle features of diffuse and extensive centrilobular ground-glass opacities or other similar features. |
|
Unlikely |
No evidence of diffuse and extensive centrilobular ground-glass opacity. |
|
Pathologic criteria |
Definite |
Non-suppurative necrotizing and obliterate bronchiolitis with various stages of peribronchiolar organizing alveolar damage. Relative sparing of the subpleural and paraseptal parenchyma. |
|
Probable |
Patchy distribution of alveolar damage with predominant centrilobular distribution. Cellular and fibrosing interstitial pneumonia with predominant centrilobular distribution but without granuloma. |
|
Possible |
Diffuse alveolar damage, fibrinous and organizing pneumonia. |
|
Unlikely |
Suppurative inflammation with bronchopneumonia or lobar pneumonia pattern. Evidence of infectious acute or chronic pneumonia. |
Centrilobular distribution and subpleural sparing are the main pathologies of HDLI.
2 Subpleural sparing is considered in the differential diagnosis of HDLI, idiopathic pulmonary fibrosis, and ARDS. Furthermore, HDLI is characterized by radiological changes over time. It begins with areas of patchy consolidation involving the upper lung periphery and posterior lower lung zones, but sparing the subpleural areas. These areas evolve into centrilobular opacities, and the consolidation disappears about 5 years after the cessation of HD exposure.
912 However, there are limited radiological long-term follow-up data of patients with advanced HDLI.
2912 In particular, little is known about radiological differences between children and adults long after cessation of exposure to HD.
Thus, we aimed to compare chest computed tomography (CT) images of children and adults in families with clusters of HDLI long after cessation of exposure to HD.
METHODS
Data were from the Korea Environmental Industry & Technology Institute, which officially collected information on individuals with lung disease, each of whom claimed that the disease was related to use of HD. Each registered claimant was clinically examined for diagnosis and confirmation of HDLI. The combination of clinical manifestations, natural disease course, exposure to HD, and radiological and pathological findings were used for confirmation.
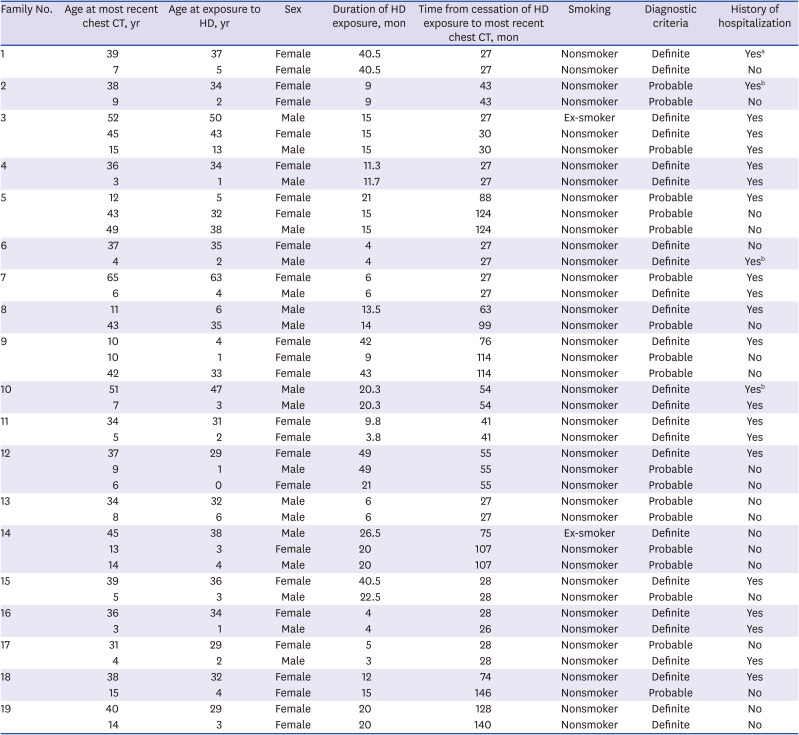
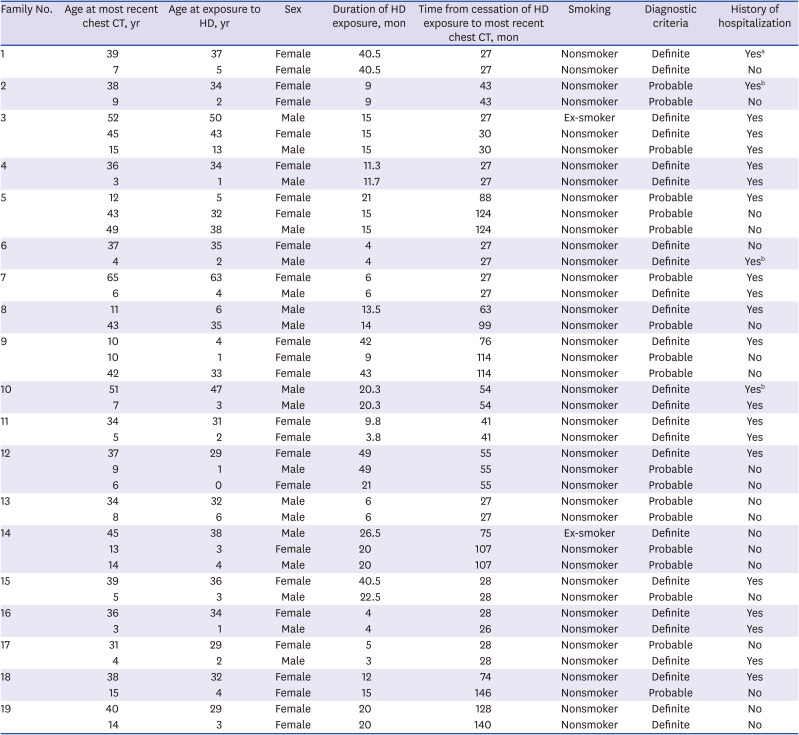
A total of 1,196 individuals from 748 families claimed that HD exposure was related to their diseases during the first three rounds of investigations (July 2013 to December 2015). The medical records and exposure histories of families that had at least two patients with definite or probable HDLI (“confirmed HDLI”) were identified (200 individuals from 64 families). Then, families were selected for the present study if they had both children and adults among the confirmed HDLI patients. Finally, 19 families with 43 patients (21 adults, 22 children) were analyzed. Each included family had at least one adult and one child with HDLI. Fourteen families (28 patients) had one adult and one child; two families (6 patients) had two adults and one child; and three families (9 patients) had one adult and two children. The age, sex, history of smoking, duration of using HD exposure, history of hospitalization and clinical course during acute HDLI period, chest CT taken during acute and chronic HDLI period, and time from cessation of HD exposure to chest CT examination was recorded for each of the 43 patients (
Table 2).
Table 2
General characteristics of patients with chronic HDLI (n = 43)
|
Family No. |
Age at most recent chest CT, yr |
Age at exposure to HD, yr |
Sex |
Duration of HD exposure, mon |
Time from cessation of HD exposure to most recent chest CT, mon |
Smoking |
Diagnostic criteria |
History of hospitalization |
|
1 |
39 |
37 |
Female |
40.5 |
27 |
Nonsmoker |
Definite |
Yesa
|
|
7 |
5 |
Female |
40.5 |
27 |
Nonsmoker |
Definite |
No |
|
2 |
38 |
34 |
Female |
9 |
43 |
Nonsmoker |
Probable |
Yesb
|
|
9 |
2 |
Female |
9 |
43 |
Nonsmoker |
Probable |
No |
|
3 |
52 |
50 |
Male |
15 |
27 |
Ex-smoker |
Definite |
Yes |
|
45 |
43 |
Female |
15 |
30 |
Nonsmoker |
Definite |
Yes |
|
15 |
13 |
Male |
15 |
30 |
Nonsmoker |
Probable |
Yes |
|
4 |
36 |
34 |
Female |
11.3 |
27 |
Nonsmoker |
Definite |
Yes |
|
3 |
1 |
Male |
11.7 |
27 |
Nonsmoker |
Definite |
Yes |
|
5 |
12 |
5 |
Female |
21 |
88 |
Nonsmoker |
Probable |
Yes |
|
43 |
32 |
Female |
15 |
124 |
Nonsmoker |
Probable |
No |
|
49 |
38 |
Male |
15 |
124 |
Nonsmoker |
Probable |
No |
|
6 |
37 |
35 |
Female |
4 |
27 |
Nonsmoker |
Definite |
No |
|
4 |
2 |
Male |
4 |
27 |
Nonsmoker |
Definite |
Yesb
|
|
7 |
65 |
63 |
Female |
6 |
27 |
Nonsmoker |
Probable |
Yes |
|
6 |
4 |
Male |
6 |
27 |
Nonsmoker |
Definite |
Yes |
|
8 |
11 |
6 |
Male |
13.5 |
63 |
Nonsmoker |
Definite |
Yes |
|
43 |
35 |
Male |
14 |
99 |
Nonsmoker |
Probable |
No |
|
9 |
10 |
4 |
Female |
42 |
76 |
Nonsmoker |
Definite |
Yes |
|
10 |
1 |
Female |
9 |
114 |
Nonsmoker |
Probable |
No |
|
42 |
33 |
Female |
43 |
114 |
Nonsmoker |
Probable |
No |
|
10 |
51 |
47 |
Male |
20.3 |
54 |
Nonsmoker |
Definite |
Yesb
|
|
7 |
3 |
Male |
20.3 |
54 |
Nonsmoker |
Definite |
Yes |
|
11 |
34 |
31 |
Female |
9.8 |
41 |
Nonsmoker |
Definite |
Yes |
|
5 |
2 |
Female |
3.8 |
41 |
Nonsmoker |
Definite |
Yes |
|
12 |
37 |
29 |
Female |
49 |
55 |
Nonsmoker |
Definite |
Yes |
|
9 |
1 |
Male |
49 |
55 |
Nonsmoker |
Probable |
No |
|
6 |
0 |
Female |
21 |
55 |
Nonsmoker |
Probable |
No |
|
13 |
34 |
32 |
Male |
6 |
27 |
Nonsmoker |
Probable |
No |
|
8 |
6 |
Male |
6 |
27 |
Nonsmoker |
Probable |
No |
|
14 |
45 |
38 |
Male |
26.5 |
75 |
Ex-smoker |
Definite |
No |
|
13 |
3 |
Female |
20 |
107 |
Nonsmoker |
Probable |
No |
|
14 |
4 |
Male |
20 |
107 |
Nonsmoker |
Probable |
No |
|
15 |
39 |
36 |
Female |
40.5 |
28 |
Nonsmoker |
Definite |
Yes |
|
5 |
3 |
Male |
22.5 |
28 |
Nonsmoker |
Probable |
No |
|
16 |
36 |
34 |
Female |
4 |
28 |
Nonsmoker |
Definite |
Yes |
|
3 |
1 |
Male |
4 |
26 |
Nonsmoker |
Definite |
Yes |
|
17 |
31 |
29 |
Female |
5 |
28 |
Nonsmoker |
Probable |
No |
|
4 |
2 |
Male |
3 |
28 |
Nonsmoker |
Definite |
Yes |
|
18 |
38 |
32 |
Female |
12 |
74 |
Nonsmoker |
Definite |
Yes |
|
15 |
4 |
Female |
15 |
146 |
Nonsmoker |
Probable |
No |
|
19 |
40 |
29 |
Female |
20 |
128 |
Nonsmoker |
Definite |
No |
|
14 |
3 |
Female |
20 |
140 |
Nonsmoker |
Definite |
No |
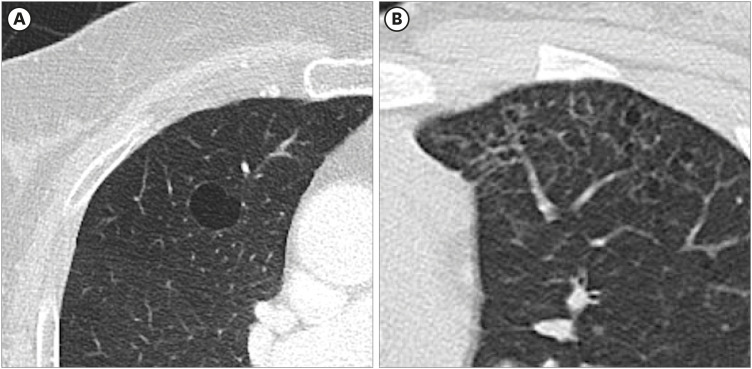
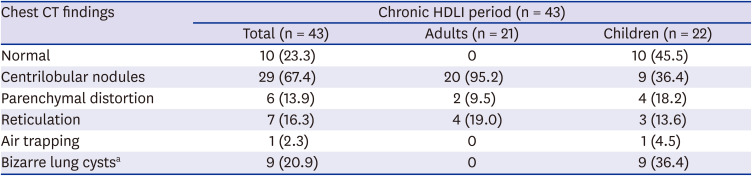
Each patient received chest CT examination at different hospitals in Korea for evaluation of the lung manifestations of HDLI. Various MDCT scanners were used for this study, for example, 16 channel MDCT (Somatom Sensation 16; Siemens Healthcare, Erlangen, Germany), 64 channel MDCT (Aquillion 64; Toshiba, Tokyo, Japan) or 128 channel multidetector CT (Somatom Definition Flash; Siemens Healthcare). Tube voltage between 80–120 kVp, 100–120 effective mAs with dose modulation were used. All exams included a high-resolution axial image with a thickness of less than 2 mm, and analysis at a window width of 1,500 HU and a window level of −600 HU. Two chest radiologists with 5 and 16 years of experience evaluated CT results in consensus. They classified chest CT findings during acute HDLI period as consolidation, subpleural sparing, ground-glass opacity, and air leak. Follow-up CT findings were classified as normal, centrilobular nodule, parenchymal distortion, reticulation, and air trapping based on the guidelines of the Fleischner Society.
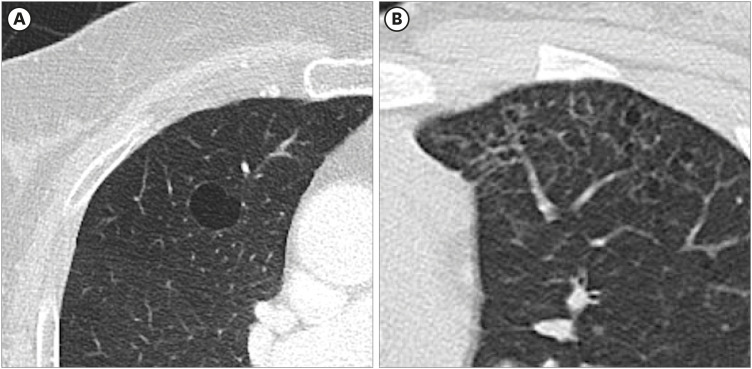
13 In our cases, multiple cystic parenchymal lucency were found in children, with irregular and bizarre in shape. The Fleischner Society described lung cyst as a round parenchymal lucency with a well-defined interface with normal lung.
13 So we categorized those finding as bizarre lung cysts and included them in the analysis (
Fig. 1).
Fig. 1
Comparison of the shape of classic lung cyst and bizarre lung cyst. (A) The Fleischner Society described lung cyst as a round parenchymal lucency with a well-defined interface with normal lung. (B) A 11 years old girl with bizarre lung cysts (family No.19). Variable shaped lung cysts and relatively well-defined interface with normal lung.
Statistical analysis was performed using IBM SPSS version 21.0 (IBM Corp., Armonk, NY, USA). The demographic characteristics of all patients are presented, and a Fisher's exact test was used to compare differences between adults and children.
Ethics statement
After receiving an explanation of the survey, all participants provided written informed consent for participation. This survey was approved by the Institutional Review Board of the National Institute of Environmental Research (NIER-2018-04-02-075).
RESULTS
We enrolled 19 families with 21 adults (6 men and 15 women) and 22 children (12 boys and 10 girls), 4 of whom were exposed to HD during gestation (
Tables 3 and
4). The overall mean duration of HD exposure was 17.6 ± 13.1 months (17.0 ± 13.1 months in adults and 15.9 ± 11.9 months in children). The mean duration from cessation of exposure to HD to the latest CT exam was 55.4 months (duration: 27–128 months) for adults and 58.5 months (duration: 27–146 months) for children. All 22 children had no prior hospitalization for congenital or perinatal period disorder, or lung-related disease such as pneumonia or bronchiolitis.
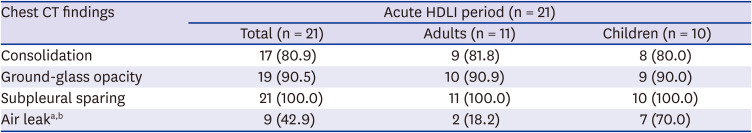
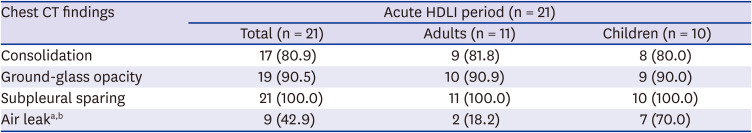
Table 3
Chest CT findings of adults and children during acute HDLI period
|
Chest CT findings |
Acute HDLI period (n = 21) |
|
Total (n = 21) |
Adults (n = 11) |
Children (n = 10) |
|
Consolidation |
17 (80.9) |
9 (81.8) |
8 (80.0) |
|
Ground-glass opacity |
19 (90.5) |
10 (90.9) |
9 (90.0) |
|
Subpleural sparing |
21 (100.0) |
11 (100.0) |
10 (100.0) |
|
Air leaka,b
|
9 (42.9) |
2 (18.2) |
7 (70.0) |
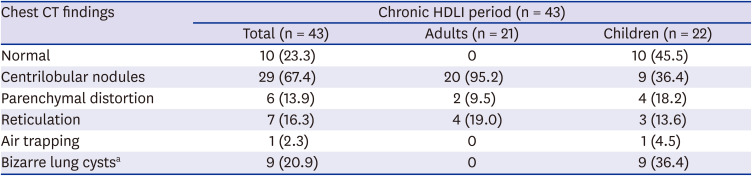
Table 4
Chest CT findings of adults and children during chronic HDLI period
|
Chest CT findings |
Chronic HDLI period (n = 43) |
|
Total (n = 43) |
Adults (n = 21) |
Children (n = 22) |
|
Normal |
10 (23.3) |
0 |
10 (45.5) |
|
Centrilobular nodules |
29 (67.4) |
20 (95.2) |
9 (36.4) |
|
Parenchymal distortion |
6 (13.9) |
2 (9.5) |
4 (18.2) |
|
Reticulation |
7 (16.3) |
4 (19.0) |
3 (13.6) |
|
Air trapping |
1 (2.3) |
0 |
1 (4.5) |
|
Bizarre lung cystsa
|
9 (20.9) |
0 |
9 (36.4) |
Of the 43 patients, 11 adults and 10 children were hospitalized during acute HDLI period. Two adults and a child underwent intensive treatment including a mechanical ventilator at the ICU. Their length of stay was 10 and 62 days in adults and 54 days in a child. The duration of ventilator use was 10, 36, and 35 days, respectively. No patients suffered from infectious diseases such as pneumonia during their hospital stay. All 21 patients underwent chest CT during their acute HDLI period. The most common findings in these patients were subpleural sparing (100%), followed by ground-glass opacity (90.4%) and consolidation (80.9%). Air leak was observed in 9 patients (42.9%). One patient underwent chest tube insertion due to pneumothorax. Interestingly, the incidence of air leak was significantly higher in children than in adults (
P = 0.03) (
Tables 3 and
4).
Among the 6 categories of chronic CT findings, the most frequent pattern overall was centrilobular nodules (67.4%) (
Tables 3 and
4), and this finding was especially predominant in adults (95.2%). However, 45.5% of children had normal chest CT results, followed by 36.4% with centrilobular nodules, 36.4% with bizarre lung cysts, and 13.6% with reticulation. Fisher's exact test indicated the incidence of bizarre lung cysts was significantly greater in children than adults (
P = 0.001).
DISCUSSION
The current diagnostic criteria for HDLI are highly specific, in that they focus on rapidly progressive and severe lung injury. These criteria were developed to exclude patients whose clinical signs and symptoms may be similar, but not caused by HD exposure. Radiologically, HLDI is characterized by diffuse centrilobular ground-glass opacity and nodules, sparing of subpleural spaces, and often with spontaneous air leaks, such as a pneumothorax or pneumomediastinum, but with no evidence of air trapping or reticular opacity. There is evidence that the radiologic features of HDLI change over time.
78 More specifically, there are initially areas of patchy consolidation involving the upper lung periphery and posterior lower lung zones, but sparing of the subpleural areas. As disease progressed, spontaneous air leak such as pneumothorax, pneumomediastinum or interstitial emphysema could be occurred.
14 Over time, these areas evolve into centrilobular opacities with a gradual disappearance of the consolidation at about 5 years after cessation of HD exposure.
78 Thus, a bronchocentric distribution of nodules is considered the most characteristic CT feature of HDLI in chronic period, and the causative mechanism of bronchocentric injury pattern was an inhalation of HD.
789
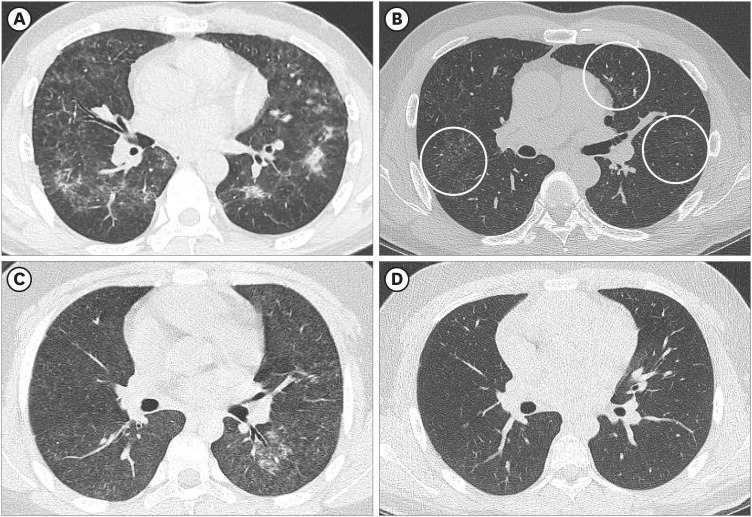
We found that centrilobular nodules were very common (95.2%) in adults with HDLI at an average of 55 months after cessation of exposure to HD. However, normal radiologic findings were most common (45.5%) (
Fig. 2), followed by centrilobular nodules in children with HDLI after long term follow-up (36.4%) (
Fig. 3). However, Yoon and her colleagues found that centrilobular nodule were the most common finding in chronic HDLI children.
8 This discrepancy is probably due to the differences in the average follow-up periods; those in the present study was twice as long as those in the previous study. (58.5 months vs. 27.4 months). Furthermore, the lungs of children were still undergoing development. For example, the alveolar ducts of the lungs continue to mature until age 19 months, and microvascular structure matures until about age 21 years.
15 Thus, the centrilobular nodules in children with HDLI may disappear several years after cessation of exposure to HD due to their continuing lung development. If this interpretation is correct, then diagnosis of HDLI in children can be problematic when based on chest CT imaging that is performed several years after the cessation of exposure to HD.
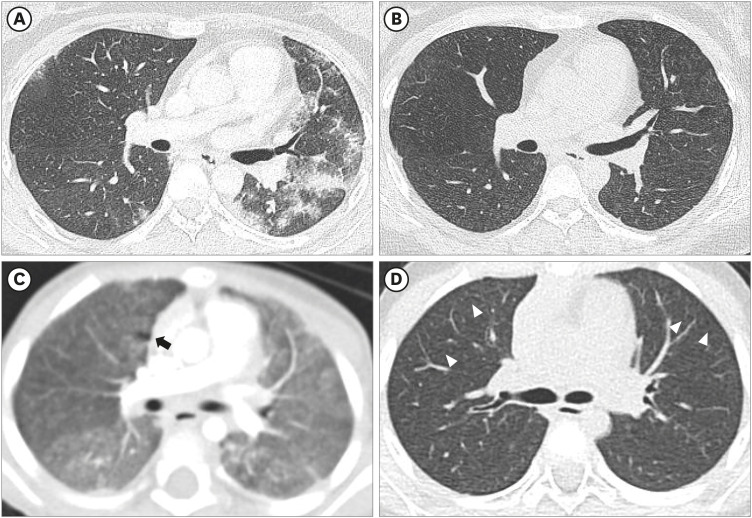
Fig. 2
Comparison of acute and chronic HDLI image between adult and child patients (family No. 3). (A, B) Chest CT of a 50-year-old man with 15 months' HD exposure. (A) Bilateral ill-defined centrilobular nodules, patchy consolidations with subpleural sparing indicates typical acute HDLI finding. (B) Two years after HD exposure cessation. Tiny, ill-defined centrilobular nodules were noted in bilateral lungs (circle). (C, D) Chest CT of a 13-year-old boy with HDLI exposure. (C) Diffuse, ill-defined centrilobular nodules, ground-glass opacity with subpleural sparing and some consolidations involving both lungs. (D) Two years after HD exposure cessation. Previous findings disappeared and showed normal lung parenchyma.
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
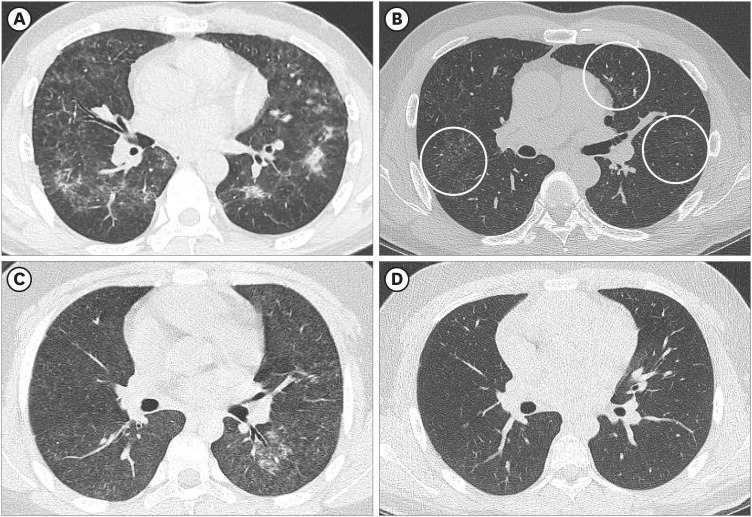
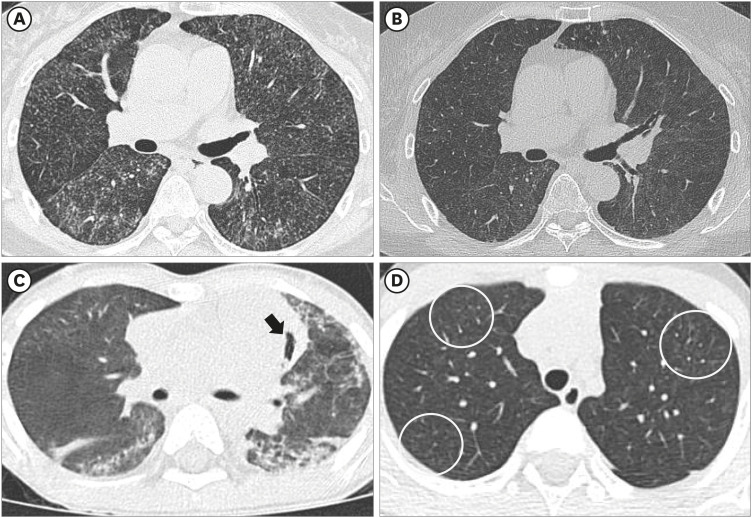
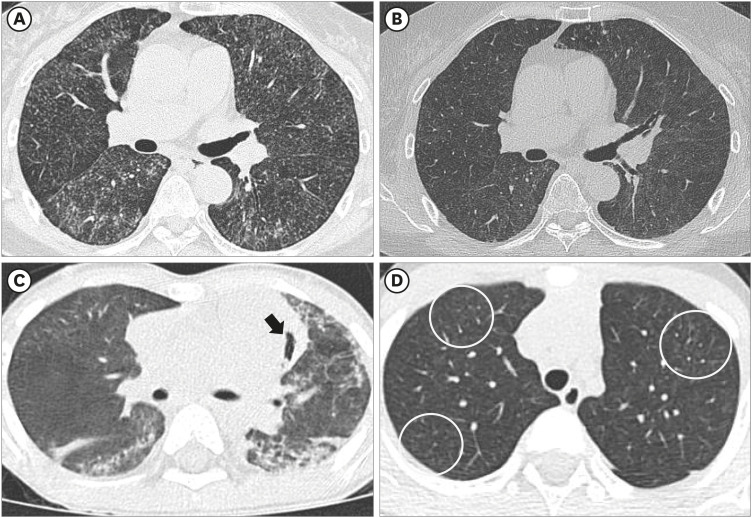
Fig. 3
Comparison of acute and chronic HDLI image between adult and child patients (family No. 7). (A, B) CT of a 63-year-old woman with 6 months HD exposure. (A) Bilateral ill-defined centrilobular nodules and ground-glass opacity with subpleural sparing indicates acute to subacute stage HDLI finding. (B) Two years after HD exposure cessation. Tiny, extensive centrilobular nodules were noted in bilateral lungs. (C, D) CT of a 4-year-old boy with acute HDLI exposure. (C) Bilateral, multifocal consolidations and ground-glass opacity involving both lung parenchyma. Pneumomediastinum also was noted (black arrow). (D) Two years after HD exposure cessation. Subtle, subpleural ill-defined centrilobular nodules remained in both upper lobes (circles).
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
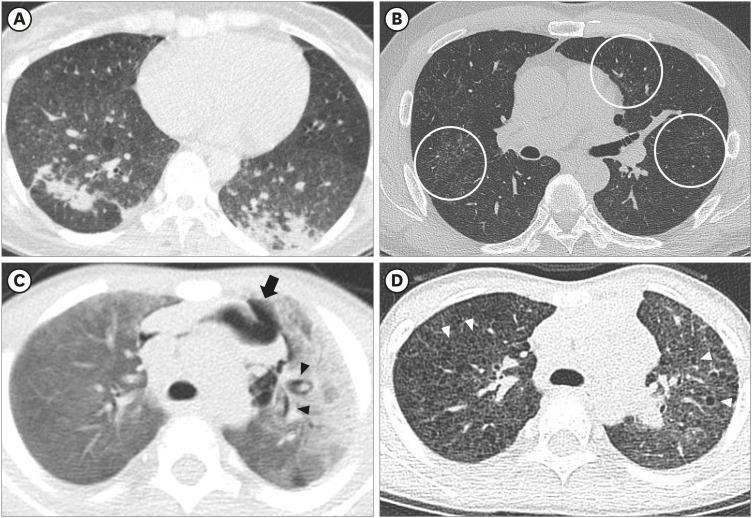
The frequency of bizarre lung cysts in long-term follow-up was significantly greater in children than adults (
Figs. 4-
7). Our finding that bizarre lung cysts observed in in the long term follow-up, especially in children, could be another key CT finding to determine chronic HDLI. Classic lung cyst is one of well-known parenchymal change after infection, especially bacterial lobar pneumonia or pneumocystis pneumonia. Cystic lung disease such as Langerhans cell histiocytosis or lymphocytic interstitial pneumonia can present bizarre shaped lung cysts in adults.
1617 However, those diseases are very rare in childhood.
18 In the present study, bizarre lung cysts were more frequently observed in children than adults after cessation of similar exposure to HD in the same room, even if adults demonstrated chronic, typical centrilobular nodules. Thus, bizarre lung cysts may be useful as another novel finding of chronic HDLI in children who have no history of pulmonary infection, or other perinatal disorder such as hyaline membrane disease.
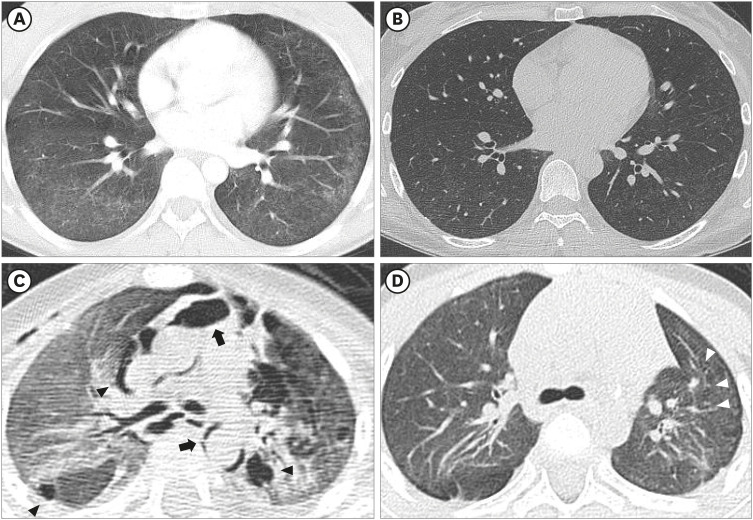
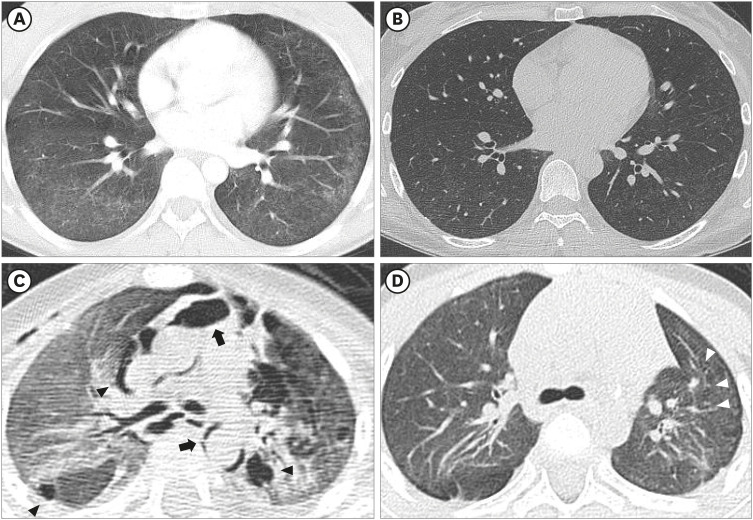
Fig. 4
Comparison of acute and chronic HDLI image between adult and child patients (family No. 6). (A, B) CT of a 35-year-old woman with 4 months HD exposure. (A) Bilateral ill-defined centrilobular nodules, consolidation and subpleural sparing indicates typical acute HDLI finding. (B) Two years after HD exposure cessation. Tiny, ill-defined centrilobular nodules were noted in the subpleural portion of the bilateral lower lobes (circles). (C, D) CT of a 2-year-old boy with HD exposure. (C) Bilateral extensive consolidation and ground-glass opacity involving both lungs. Pneumomediastinum (black arrow) and interstitial emphysema (black arrowheads). (D) Two years after HD exposure cessation. Numerous bizarre lung cysts (white arrowheads) are scattered in bilateral lungs.
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
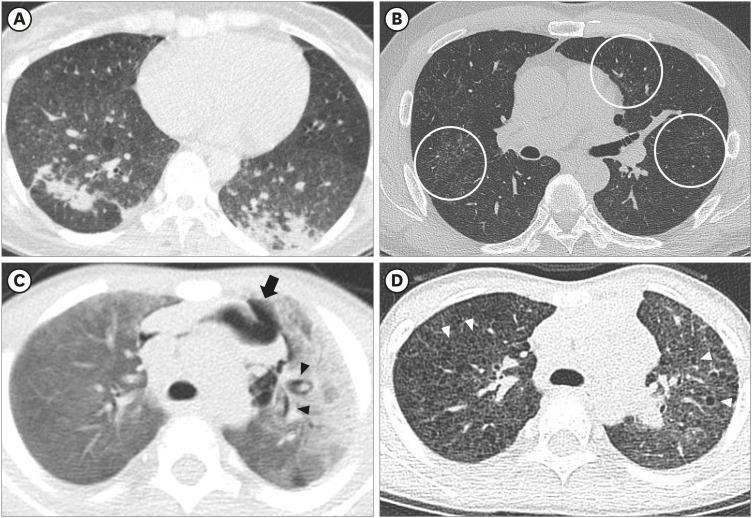
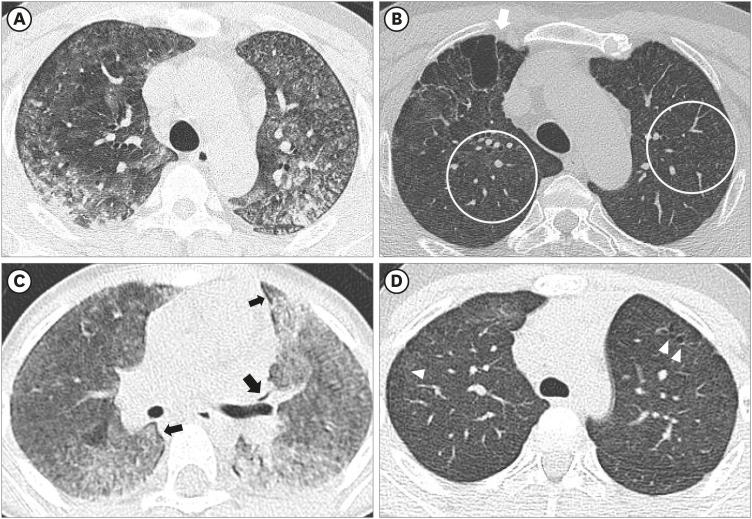
Fig. 5
Comparison of acute and chronic HDLI image between adult and child patients (family No. 10). (A, B) CT of a 47-year-old man with 20.3 months HD exposure. (A) Bilateral, extensive ground-glass opacity with subpleural sparing and irregular consolidations involving both lungs, indicates acute HDLI finding. (B) Four years after HD exposure cessation. Tiny, extensive centrilobular nodules were noted in bilateral lungs (circles). Due to previous lung damage, parenchymal distortion and bullae developed in the right upper lobe (white arrow). (C, D) CT of a 4-year-old boy with HD exposure. (C) Bilateral, extensive ground glass opacity and consolidation involve bilateral lungs. Interstitial emphysema was also noted (black arrow). (D) Four years after HD exposure cessation. Several bizarre lung cysts are noted in bilateral upper lobes (white arrowheads).
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
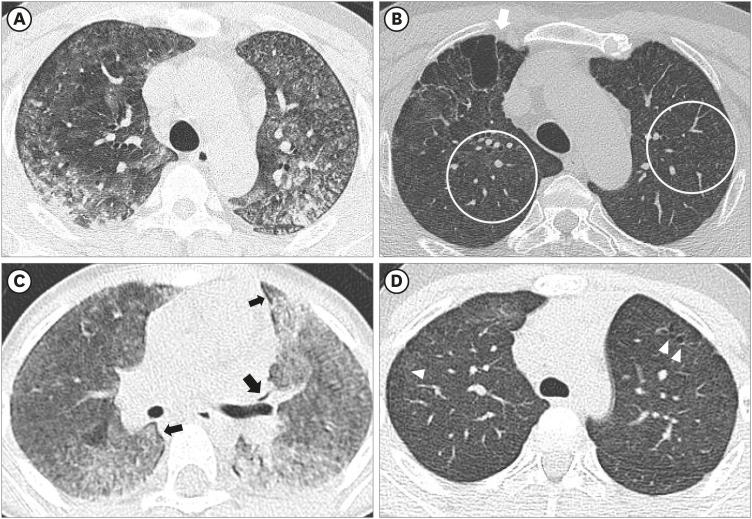
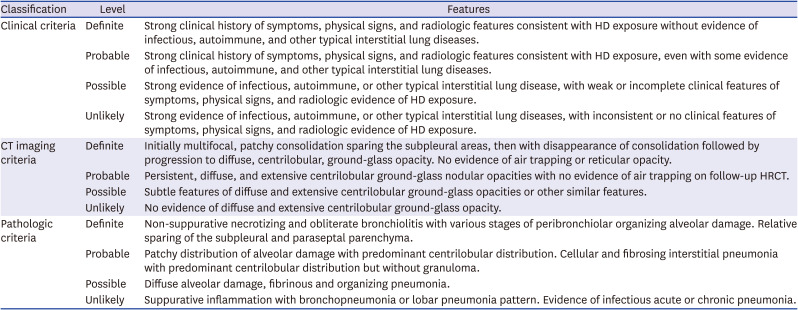
Fig. 6
Comparison of acute and chronic HDLI image between adult and child patients (family No. 11). (A, B) CT of a 34-year-old woman with 9.8 months HD exposure. (A) Ill-defined centrilobular nodules and some consolidations were noted in bilateral lungs. (B) Three years after HD exposure cessation. Tiny, extensive centrilobular nodules were noted in bilateral lungs. (C, D) CT of a 2-year-old girl with HD exposure. (C) Bilateral, extensive ground glass opacity and ill-defined centrilobular nodules involve bilateral lungs. Interstitial emphysema was also noted (black arrow). (D) Three years after HD exposure cessation. Subtle bizarre lung cysts were noted in bilateral upper lobes (white arrowheads).
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
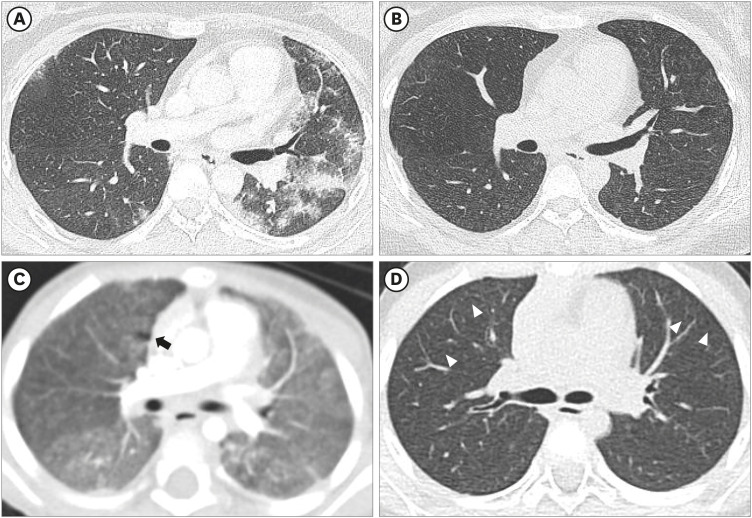
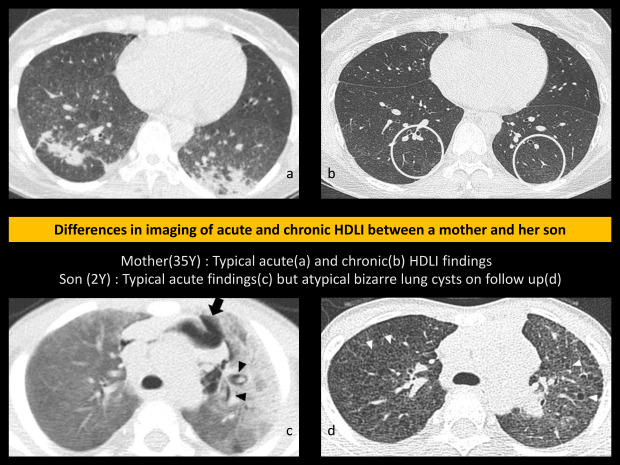
Fig. 7
Comparison of acute and chronic HDLI image between adult and child patients (family No. 16). (A, B) CT of a 34-year-old woman with 4 months' HD exposure. (A) Extensive, ill-defined tiny centrilobular nodules were noted in bilateral lungs, presumed to be subacute stage of HDLI. (B) Two years after HD exposure cessation. Very tiny centrilobular nodules remain in lung parenchyma. (C, D) CT of a 1-year-old boy with HDLI exposure. (C) Bilateral, extensive ground glass opacity and consolidations, indicates acute HDLI finding. Pneumomediastinum (black arrows) and interstitial emphysema (black arrowheads) were also found. (D) Two years after HD exposure cessation. Distortion of bilateral lungs suggest post-inflammatory parenchymal changes. Subtle bizarre lung cysts were noted in the left upper lobe (white arrowheads).
HDLI = humidifier disinfectant-related lung injury, CT = computed tomography, HD = humidifier disinfectant.
We observed reticulation in 4 adults (19.0%) and 3 children (13.6%), and air trapping in an adult and a child. Findings of these patients are not compatible with the current diagnostic criteria of HDLI, which do not include air trapping and reticular opacity. As shown in previous papers, reticulation is considered as findings frequently shown in other interstitial lung disease such as usual interstitial pneumonia or chronic hypersensitivity pneumonitis (HP) rather than HDLI.
3510 However, clinical disorders in which reticulation frequently is observed are rare in children, contrasted with adults, and thus, reticulation are probably due to HDLI. Moreover, familial clustering is seldom identified in other interstitial lung disease during childhood.
14 Thus, abnormal lung lesion such as bizarre lung cysts or reticulation in a suspected child who have history of HD exposure or HD victim in family should be considered as late sequelae of HDLI.
It is difficult to distinguish HDLI from HP because ill-defined centrilobular nodules, which are characteristic findings of subacute HP, resemble those in HDLI.
19 In chronic HP cases, chest CT image shows reticulation, traction bronchiectasis, and bronchiolectasis, which mainly involves the subpleural or peribronchovascular region.
20 Although pathologic findings and response to corticosteroid therapy are different for patients with HP and HDLI, subpleural reticulation and traction bronchiectasis may also be late sequelae of HDLI.
359
Air trapping or bronchial wall thickening, the main CT findings of asthma, was rare among our patients.
21 However, a recent study proposed a possibly causal association between exposure to HD and asthma, especially in pediatric patients.
22 Thus, the possibility of HDLI should be considered when asthma-related findings are seen in the CT of a patient who has evidence of significant exposure to HD.
The present study is the first to compare chest CT images of children and adults after cessation of exposure to HD in families with clusters of HDLI, in which family members were exposed to high levels of HD in the same room (homogenous exposure group). Little is known about differences between children and adults about the long-term natural history of HDLI. Therefore, long-term follow-up of children and adults with HDLI after cessation of exposure to HD will provide a basis for improved understanding of the natural history of HDLI and the difference between children and adults.
The present study has several clinical implications. First, based on chest radiology after cessation of exposure to HD, we showed that HDLI may have diverse progression over time. In particular, children have a markedly different radiologic course of changes than adults, a finding that should be considered with other diagnostic radiologic criteria. Thus, the diagnosis of HDLI in children with past exposure to HD appears more challenging.
The present study had several strengths. We examined patients with confirmed HDLI (definite or probable) within the same family who had similar exposures to high levels of HD in the same environment (homogenous exposure group). Familial clustering of HDLI reliably indicates common exposure to a high concentration of HD. Thus, we were able to make a direct comparison between adults and children regarding radiologic changes long after the cessation of exposure.
The present study also had several limitations. First, the number of patients was small, and we did not apply statistical analysis due to the low statistical power. A large-scale follow-up imaging study is needed to examine additional patients recognized in the fourth round of this investigation.
Second, we used family clustering of HDLI as surrogate index of high exposure. Even within the affected family members, the exposure level may be different, however, quantitative assessment of exposure level cannot be ensured because exposure level depended on memory long after exposure, and compensation issues might compound exposure assessment. Thus, family clustering of HDLI as surrogate index of high exposure seems reasonable although the strength of the exposure could be different even within the family members. Finally, initial imaging was not available in some patients.
In conclusion, we identified several radiologic findings in children and adults with familial clustering of HDLI based on chest CT imaging results from several years after cessation of exposure to HD. Some of these findings differ from the established diagnostic radiologic criteria for HDLI. In particular, the radiologic findings at several years after cessation of exposure to HD were different for children and adults. Our results may serve a basis for an improved understanding of the pathogenesis of HDLI and help to better characterize the natural course of this disease in adults and children.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download