INTRODUCTION
According to World Health Organization data, the number of cases of coronavirus disease 2019 (COVID-19) reached six million worldwide in May 2020, with the related number of deaths standing at 367,166 in the same month.
1 In the context of Korea, there was a surge in the number of COVID-19 cases in March, with Daegu becoming the epicenter in terms of both the number of confirmed cases and screening tests. By the end of April, there were 10,765 confirmed cases in the country, of which 63.7% (6,852) were in Daegu; this translates to 281.22 confirmed cases per 100,000 people.
2
Healthcare workers are at the frontline of this unprecedented crisis, treating patients with COVID-19 and attempting to prevent new infections. Pandemics, in general, expose healthcare workers to heavy workloads and work-related stresses. Specifically, they are at high risk of infection, fears related to which can pose a psychological burden.
3 Moreover, they can be stigmatized because of their proximity to patients, and feelings of rejection and isolation further contribute to their psychological stress.
4
Prior to COVID-19, there were outbreaks of severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome in several countries. In this context, research has assessed healthcare workers' anxiety,
567 depression,
8 anger,
7 and posttraumatic stress.
59 A significant finding across studies has been healthcare workers' fear of infecting their families and friends because of the nature of their work.
810 The current outbreak of COVID-19 is no different, with reports of healthcare workers, especially nurses in Wuhan, China, experiencing psychological burden.
3 The factors associated with aggravated emotional stress include an uncontrolled number of new cases, insufficient personal protective equipment, and risk of infections. Thus, in this crisis, healthcare workers are in need of adequate mental healthcare. However, to determine the psychological support measures required, it is necessary to identify who is most vulnerable, which factors are most closely related to stress, and how severe the situation is.
In this context, we aimed to describe and assess immediate emotional stress in the healthcare workers of a university hospital. Depression and anxiety are examined in relation to the nature of the job, department, exposure routes, and other related factors. We report here the immediate psychological responses of healthcare workers during the COVID-19 outbreak.
Go to :

METHODS
Design and setting
This cross-sectional study was conducted at a university hospital in Daegu from April 2 to 10, 2020. In March, when it was designated as a COVID-19 care center, 4,998 screening tests were performed at the institute's drive-through test booth. The hospital also has a designated COVID-19 ward that can accommodate up to 100 beds. We sent Google survey requests to 2,650 employees.
Variables
The respondents were asked to mention their age, gender, education, and marital status. In addition, they were questioned about their position, duration of employment, and department during the COVID-19 outbreak. Their underlying diseases were reported, if any, and following questions were followed: 1) What is your level of exposure to COVID-19 while working?, 2) Have you ever been in contact with a patient with COVID-19?, 3) Have you ever undergone COVID-19 screening?, 4) Are there any confirmed or suspected COVID-19 cases in your family?, 5) Have you ever experienced social rejection or other negative experiences because of your job?, and 6) Are you satisfied with the personal protective equipment provided to you?
Depression was assessed with the Korean version of nine-item Patient Health Questionnaire (PHQ-9). Each item is scored on a four-point Likert scale from 0 (not at all) to 3 (nearly every day). The total score ranges from 0 to 27, with higher scores indicating greater depressive symptoms. A score of 10 represents the cutoff for moderate to severe depression. The validity and reliability were reported in previous studies.
111213 The Cronbach's alpha coefficient from the PHQ-9 was reported as 0.81.
14
Anxiety was assessed with the Korean version of seven-item Generalized Anxiety Disorder (GAD-7) scale (range, 0–21). The GAD-7 has an accepted cutoff value of 10.
15 Its total score is interpreted as follows: no clinically significant anxiety, score of 0–4; mild anxiety, score of 5–9; moderate anxiety, score of 10–14; and severe anxiety, score of 15–21. The Cronbach's alpha coefficient from the GAD was 0.85. The sensitivity and specificity of the Korean version of GAD-7 were 81.8% and 89.9%, respectively.
16
The subjective risk score was calculated using a visual analog scale (VAS) from 0 to 10. The 0 score represent the respondent felt no risk at all, and 10 represent highest risk they recognize. For example, if a respondent felt no risk of COVID-19 at all while working, then he or she would check ‘0’, or the other way around; if a respondent felt the highest risks about COVID-19, he or she would check ‘10’.
Statistical analysis
Respondents' characteristics and answers were presented using descriptive statistics, and geometric mean scores and standard deviations were calculated for the PHQ-9, GAD-7, and VAS. To assess the risks according to position, department, and exposure route, we performed multiple logistic regression analysis. Lastly, the crude odds ratios (ORs) were described and adjusted for age, gender, education, marital status, and duration of employment. All statistical analyses were conducted using SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics statements
Respondents were assured of anonymity and confidentiality and written informed consent was obtained prior to the survey. This study was approved by the Institutional Review Board of Yeungnam University Hospital (YUMC 2020-03-105-002).
Go to :

RESULTS
Overall, of the 1,010 employees who responded to the survey, seven were excluded: six because they did not provide informed consent and one because of a self-reported history of psychological problems. The general characteristics of the 1,003 participants whose data were analyzed are presented in
Table 1. Of the participants, 352 (35.1%) were in their 20s, 776 (77.4%) were aged between 20 and 50, and the majority (n = 773; 77.1%) were women. Further, 710 (70.8%) had a bachelor's degree and most (n = 648; 64.6%) were nurses. Their duration of employment ranged from under five years to over 25 years, but 50.8% had worked for less than five years. One hundred and forty-three (14.2%) participants were working in the ward for confirmed COVID-19 cases, and 86 (8.6%) were involved in the drive-through COVID-19 screening booth. One hundred and fifty-three (15.2%) participants had had direct contact with patients with COVID-19, 47 (4.7%) had been exposed to test samples, 270 (26.9%) had been in contact with random or unspecified visitors, and 229 (22.9%) replied their contact with COVID-19 were very rare. In addition, 131 (13.1%) participants replied that their exposure route was unknown or uncertain.
Table 1
General characteristics of the study population (n = 1,003)

|
Variables/questionnaire |
Categories/answer |
Values |
|
Age, yr |
20s |
352 (35.1) |
|
30s |
228 (22.7) |
|
40s |
196 (19.5) |
|
50s |
207 (20.6) |
|
60s |
20 (2.0) |
|
Gender |
Men |
230 (22.9) |
|
Women |
773 (77.1) |
|
Education |
Bachelor's |
710 (70.8) |
|
Master's |
154 (15.3) |
|
PhD |
33 (3.3) |
|
Others |
106 (10.6) |
|
Marital status |
Married |
491 (49.0) |
|
Single |
494 (49.2) |
|
Separated/divorced |
19 (1.9) |
|
Position |
Doctor, staff and fellow |
37 (3.7) |
|
Doctor, intern and resident |
34 (3.4) |
|
Nurse, senior or supervisor |
37 (3.7) |
|
Nurse, junior or charge duty |
611 (60.9) |
|
Medical technician |
98 (9.8) |
|
Administrative and secretary officers |
74 (7.4) |
|
Pharmacy staff |
12 (1.2) |
|
Cafeteria workers |
18 (1.8) |
|
Others |
82 (8.2) |
|
Duration of employment |
Less than 5 years |
510 (50.8) |
|
More than 5, less than 10 years |
94 (9.4) |
|
More than 10, less than 15 years |
42 (4.2) |
|
More than 15, less than 20 years |
51 (5.1) |
|
More than 20, less than 25 years |
118 (11.8) |
|
More than 25 years |
188 (18.7) |
|
Departmenta
|
Drive-through COVID-19 screening |
86 (8.6) |
|
Gate/entrance visitor screening |
126 (12.6) |
|
Ward for confirmed COVID-19 cases |
143 (14.2) |
|
Ward for suspected COVID-19 cases |
35 (3.5) |
|
General ward (non-COVID-19) |
373 (37.2) |
|
Outpatient |
155 (15.5) |
|
Operating room |
92 (9.2) |
|
Laboratory |
19 (1.9) |
|
Cafeteria |
17 (1.7) |
|
Others |
270 (26.9) |
|
Medical statusa
|
None |
918 (91.5) |
|
Chronic diseases (hypertension, diabetes, etc.) |
43 (4.3) |
|
Respiratory diseases |
44 (4.4) |
|
What is your level of exposure to COVID-19 while working? |
Directly treat or care for patients |
153 (15.2) |
|
Close proximity within 2 meters |
22 (2.2) |
|
Within the same indoor space |
35 (3.5) |
|
Treat or deal with test samples (e.g., swab or sputum) |
47 (4.7) |
|
Contact with suspected patients |
116 (11.6) |
|
Contact with random or unspecified patients |
270 (26.9) |
|
Rare contact |
229 (22.8) |
|
Unknown or uncertain |
131 (13.1) |
|
Have you ever been in contact with a patient with COVID-19? |
Yes |
273 (27.2) |
|
No |
582 (58.0) |
|
Unknown |
148 (14.8) |
|
Have you ever undergone COVID-19 screening? |
Yes |
186 (18.5) |
|
No |
817 (81.5) |
|
Have you ever been under self-quarantine? |
Yes |
57 (5.7) |
|
No |
946 (94.3) |
|
Are there any confirmed or suspected COVID-19 cases in your family? |
Yes |
69 (6.9) |
|
No |
934 (93.1) |
|
Have you ever experienced social rejection or other negative experiences because of your job? |
Yes |
381 (38.0) |
|
No |
622 (62.0) |
|
Are you satisfied with the personal protective equipment provided to you? |
Yes |
445 (44.4) |
|
No |
558 (55.6) |

Regarding the experience of contact with patients with COVID-19 and undergoing screening, 273 (27.2%) participants fell in the former category while 186 (18.5%) belonged to the latter. As a result of contact with patients, 57 (5.7%) participants had been forced to undergo self-quarantine. More than one-third of the sample (n = 381; 38.0%) had experienced social rejection or had other negative experiences because of their jobs. Overall, 445 (44.4%) were satisfied with their personal protective equipment.
The PHQ-9, GAD-7, and VAS scores were analyzed according to position, department, and exposure route (
Table 2). The mean scores of the PHQ-9, GAD-7, and VAS for the total sample were 7.98, 4.40, and 5.69, respectively. By position, senior or supervisor nurses had the highest mean scores on the PHQ-9 (mean = 9.51) and GAD-7 (mean = 6.08). The highest percentages of depression and anxiety—45.9% and 21.6%, respectively—were also observed in these positions. Administrative and secretary officers had the second highest means on the PHQ-9 and GAD-7, followed by junior or acting duty nurses. By department, participants who worked in the ward for confirmed COVID-19 cases had the highest mean scores on the PHQ-9, GAD-7, and VAS at 10.03, 5.78, and 8.11, respectively. Moreover, at 46.9% and 20.3%, respectively, this department had the highest rates of depression and anxiety. Regarding exposure routes, healthcare workers who came in direct contact with patients with COVID-19 in the process of treatment had the highest mean scores on the PHQ-9, GAD-7, and VAS at 10.18, 5.58, and 8.31, respectively. The proportion with moderate to severe risk of depression and anxiety was the highest in these respondents.
Table 2
Depression, anxiety, and self-reported risks by position, department, and related factors

|
Categories |
Variables |
PHQ-9 |
Depression |
GAD-7 |
Anxiety |
VAS |
|
Position |
Doctor, staff and fellow |
6.97 ± 5.29 |
10 (27.0) |
4.11 ± 4.07 |
2 (5.4) |
4.57 ± 2.65 |
|
Doctor, intern and resident |
4.94 ± 5.53 |
5 (14.7) |
1.74 ± 3.32 |
2 (5.9) |
6.09 ± 1.88 |
|
Nurses, senior or supervisor |
9.51 ± 5.56 |
17 (45.9) |
6.08 ± 5.26 |
8 (21.6) |
6.00 ± 2.60 |
|
Nurse, junior or acting duty |
8.25 ± 5.46 |
214 (35.0) |
4.40 ± 4.73 |
76 (12.4) |
6.12 ± 2.48 |
|
Medical technician |
7.40 ± 5.05 |
29 (29.6) |
3.74 ± 4.34 |
8 (8.2) |
5.59 ± 2.41 |
|
Administrative, secretary officer |
8.95 ± 6.12 |
26 (35.1) |
5.54 ± 5.54 |
14 (18.9) |
4.62 ± 2.50 |
|
Pharmacy staff |
7.75 ± 6.86 |
5 (41.7) |
4.67 ± 5.45 |
1 (8.3) |
2.75 ± 2.01 |
|
Cafeteria worker |
7.00 ± 5.49 |
5 (27.8) |
4.28 ± 4.40 |
2 (11.1) |
3.39 ± 2.45 |
|
Others |
7.98 ± 5.61 |
23 (28.0) |
4.40 ± 4.79 |
13 (15.9) |
5.69 ± 2.58 |
|
Department |
Drive-through COVID-19 screening |
8.15 ± 6.34 |
30 (34.9) |
5.05 ± 5.80 |
15 (17.4) |
5.94 ± 2.54 |
|
Gate/entrance visitor screening |
8.11 ± 5.15 |
44 (34.9) |
4.58 ± 4.48 |
14 (11.1) |
5.15 ± 2.48 |
|
Ward for confirmed COVID-19 cases |
10.03 ± 6.26 |
67 (46.9) |
5.78 ± 5.63 |
29 (20.3) |
8.11 ± 2.05 |
|
Ward for suspected COVID-19 cases |
5.06 ± 4.67 |
4 (11.4) |
2.83 ± 4.24 |
2 (5.7) |
6.71 ± 1.90 |
|
General ward (non-COVID-19) |
7.60 ± 5.60 |
113 (30.3) |
4.12 ± 4.72 |
44 (11.8) |
5.59 ± 2.18 |
|
Outpatient |
7.74 ± 5.61 |
45 (29.0) |
4.45 ± 4.96 |
17 (11.0) |
5.65 ± 2.20 |
|
Operating room |
6.23 ± 5.38 |
20 (21.7) |
3.47 ± 4.25 |
8 (8.7) |
5.53 ± 1.99 |
|
Laboratory |
7.58 ± 5.44 |
9 (47.4) |
4.40 ± 4.79 |
1 (5.3) |
7.47 ± 1.58 |
|
Cafeteria |
7.41 ± 5.43 |
5 (29.4) |
4.35 ± 4.36 |
2 (11.8) |
3.65 ± 2.57 |
|
Others |
7.61 ± 5.60 |
85 (31.5) |
4.32 ± 4.92 |
37 (13.7) |
4.51 ± 2.48 |
|
Exposure route |
Directly treat or care for patients |
10.18 ± 6.03 |
71 (46.4) |
5.58 ± 5.50 |
31 (20.3) |
8.38 ± 1.83 |
|
In the close places within 2 meters |
8.45 ± 5.12 |
7 (31.8) |
4.05 ± 4.46 |
2 (9.1) |
7.27 ± 1.49 |
|
Within the same indoor space |
7.86 ± 4.64 |
10 (28.6) |
3.69 ± 3.23 |
2 (5.7) |
6.74 ± 1.93 |
|
Treat or deal with test samples (e.g., swab or sputum) |
9.70 ± 5.38 |
26 (55.3) |
5.04 ± 4.37 |
6 (12.8) |
7.34 ± 1.99 |
|
Contact with suspected patients |
7.55 ± 4.67 |
36 (31.0) |
3.98 ± 4.12 |
11 (9.5) |
6.09 ± 1.86 |
|
Contact with random or unspecified patients |
7.96 ± 5.36 |
89 (33.0) |
4.64 ± 4.76 |
35 (13.0) |
5.86 ± 2.06 |
|
Rare contact |
6.59 ± 5.89 |
54 (23.6) |
3.67 ± 4.96 |
25 (10.9) |
3.30 ± 2.06 |
|
Unknown or uncertain |
7.56 ± 5.44 |
41 (31.3) |
4.40 ± 4.79 |
14 (10.7) |
4.87 ± 2.01 |
|
Total |
7.98 ± 5.61 |
334 (33.3) |
4.40 ± 4.79 |
126 (12.5) |
5.69 ± 2.58 |

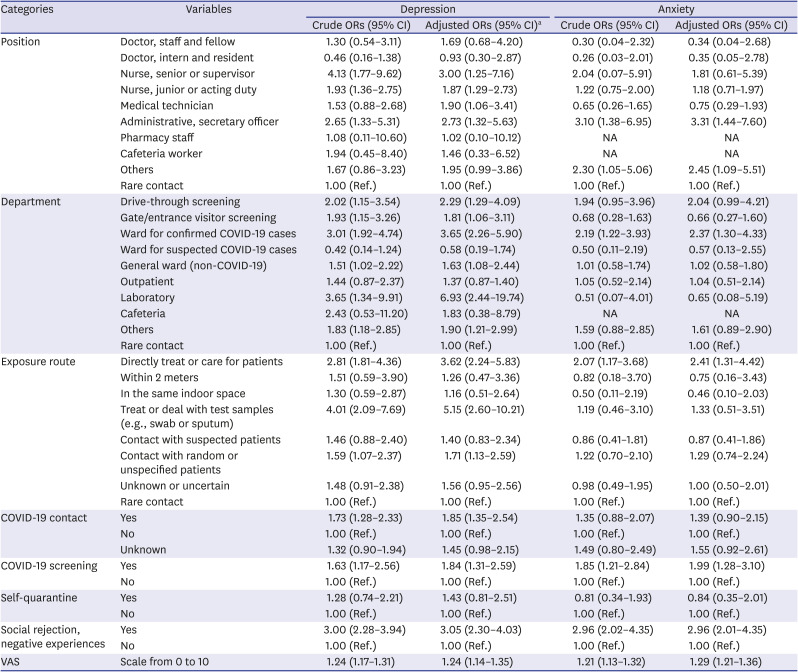
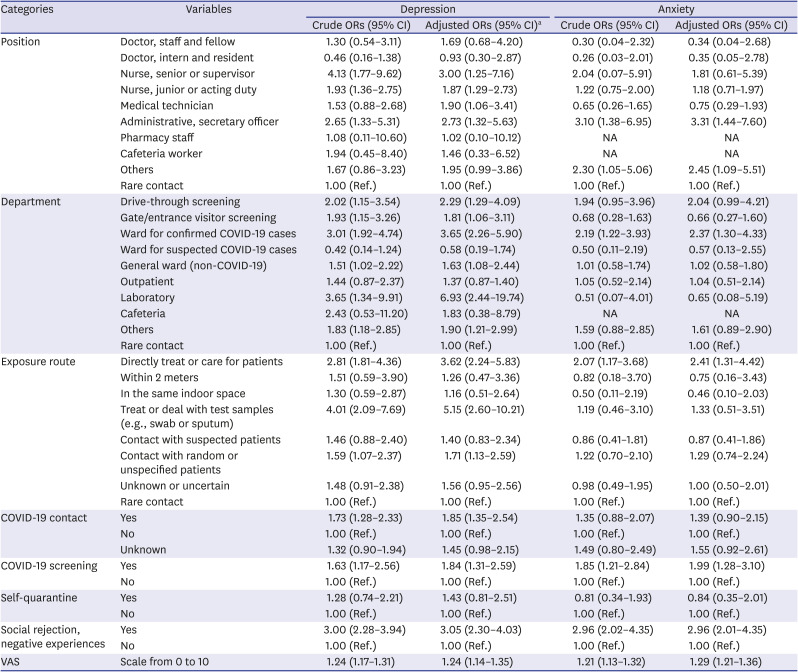
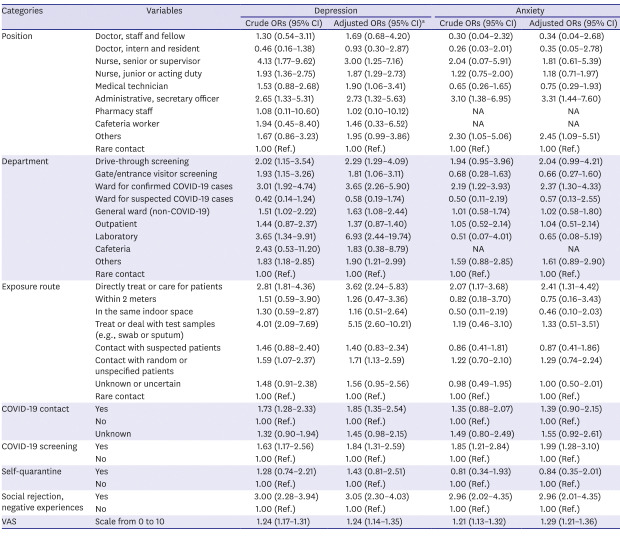
The ORs for depression and anxiety were analyzed after adjusting for age, gender, education, marital status, and duration of employment (
Table 3). Comparing those who rarely had contact with patients with COVID-19, nurses (OR, 3.00; 95% confidence interval [CI], 1.25–7.16), medical technicians (OR, 1.90; 95% CI, 1.06–3.41), and administrative and secretary officers (OR, 2.73; 95% CI, 1.32–5.63) showed statistically significantly higher ORs for depression. Among them, senior or supervisor nurses had the highest ORs, followed by administrative and secretary officers. Administrative and secretary officers also had statistically significantly higher ORs for anxiety (OR, 3.31; 95% CI, 1.44–7.60).
Table 3
Logistic regression analysis and ORs for increased anxiety, depression
|
Categories |
Variables |
Depression |
Anxiety |
|
Crude ORs (95% CI) |
Adjusted ORs (95% CI)a
|
Crude ORs (95% CI) |
Adjusted ORs (95% CI) |
|
Position |
Doctor, staff and fellow |
1.30 (0.54–3.11) |
1.69 (0.68–4.20) |
0.30 (0.04–2.32) |
0.34 (0.04–2.68) |
|
Doctor, intern and resident |
0.46 (0.16–1.38) |
0.93 (0.30–2.87) |
0.26 (0.03–2.01) |
0.35 (0.05–2.78) |
|
Nurse, senior or supervisor |
4.13 (1.77–9.62) |
3.00 (1.25–7.16) |
2.04 (0.07–5.91) |
1.81 (0.61–5.39) |
|
Nurse, junior or acting duty |
1.93 (1.36–2.75) |
1.87 (1.29–2.73) |
1.22 (0.75–2.00) |
1.18 (0.71–1.97) |
|
Medical technician |
1.53 (0.88–2.68) |
1.90 (1.06–3.41) |
0.65 (0.26–1.65) |
0.75 (0.29–1.93) |
|
Administrative, secretary officer |
2.65 (1.33–5.31) |
2.73 (1.32–5.63) |
3.10 (1.38–6.95) |
3.31 (1.44–7.60) |
|
Pharmacy staff |
1.08 (0.11–10.60) |
1.02 (0.10–10.12) |
NA |
NA |
|
Cafeteria worker |
1.94 (0.45–8.40) |
1.46 (0.33–6.52) |
NA |
NA |
|
Others |
1.67 (0.86–3.23) |
1.95 (0.99–3.86) |
2.30 (1.05–5.06) |
2.45 (1.09–5.51) |
|
Rare contact |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
Department |
Drive-through screening |
2.02 (1.15–3.54) |
2.29 (1.29–4.09) |
1.94 (0.95–3.96) |
2.04 (0.99–4.21) |
|
Gate/entrance visitor screening |
1.93 (1.15–3.26) |
1.81 (1.06–3.11) |
0.68 (0.28–1.63) |
0.66 (0.27–1.60) |
|
Ward for confirmed COVID-19 cases |
3.01 (1.92–4.74) |
3.65 (2.26–5.90) |
2.19 (1.22–3.93) |
2.37 (1.30–4.33) |
|
Ward for suspected COVID-19 cases |
0.42 (0.14–1.24) |
0.58 (0.19–1.74) |
0.50 (0.11–2.19) |
0.57 (0.13–2.55) |
|
General ward (non-COVID-19) |
1.51 (1.02–2.22) |
1.63 (1.08–2.44) |
1.01 (0.58–1.74) |
1.02 (0.58–1.80) |
|
Outpatient |
1.44 (0.87–2.37) |
1.37 (0.87–1.40) |
1.05 (0.52–2.14) |
1.04 (0.51–2.14) |
|
Laboratory |
3.65 (1.34–9.91) |
6.93 (2.44–19.74) |
0.51 (0.07–4.01) |
0.65 (0.08–5.19) |
|
Cafeteria |
2.43 (0.53–11.20) |
1.83 (0.38–8.79) |
NA |
NA |
|
Others |
1.83 (1.18–2.85) |
1.90 (1.21–2.99) |
1.59 (0.88–2.85) |
1.61 (0.89–2.90) |
|
Rare contact |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
Exposure route |
Directly treat or care for patients |
2.81 (1.81–4.36) |
3.62 (2.24–5.83) |
2.07 (1.17–3.68) |
2.41 (1.31–4.42) |
|
Within 2 meters |
1.51 (0.59–3.90) |
1.26 (0.47–3.36) |
0.82 (0.18–3.70) |
0.75 (0.16–3.43) |
|
In the same indoor space |
1.30 (0.59–2.87) |
1.16 (0.51–2.64) |
0.50 (0.11–2.19) |
0.46 (0.10–2.03) |
|
Treat or deal with test samples (e.g., swab or sputum) |
4.01 (2.09–7.69) |
5.15 (2.60–10.21) |
1.19 (0.46–3.10) |
1.33 (0.51–3.51) |
|
Contact with suspected patients |
1.46 (0.88–2.40) |
1.40 (0.83–2.34) |
0.86 (0.41–1.81) |
0.87 (0.41–1.86) |
|
Contact with random or unspecified patients |
1.59 (1.07–2.37) |
1.71 (1.13–2.59) |
1.22 (0.70–2.10) |
1.29 (0.74–2.24) |
|
Unknown or uncertain |
1.48 (0.91–2.38) |
1.56 (0.95–2.56) |
0.98 (0.49–1.95) |
1.00 (0.50–2.01) |
|
Rare contact |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
COVID-19 contact |
Yes |
1.73 (1.28–2.33) |
1.85 (1.35–2.54) |
1.35 (0.88–2.07) |
1.39 (0.90–2.15) |
|
No |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
Unknown |
1.32 (0.90–1.94) |
1.45 (0.98–2.15) |
1.49 (0.80–2.49) |
1.55 (0.92–2.61) |
|
COVID-19 screening |
Yes |
1.63 (1.17–2.56) |
1.84 (1.31–2.59) |
1.85 (1.21–2.84) |
1.99 (1.28–3.10) |
|
No |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
Self-quarantine |
Yes |
1.28 (0.74–2.21) |
1.43 (0.81–2.51) |
0.81 (0.34–1.93) |
0.84 (0.35–2.01) |
|
No |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
Social rejection, negative experiences |
Yes |
3.00 (2.28–3.94) |
3.05 (2.30–4.03) |
2.96 (2.02–4.35) |
2.96 (2.01–4.35) |
|
No |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
1.00 (Ref.) |
|
VAS |
Scale from 0 to 10 |
1.24 (1.17–1.31) |
1.24 (1.14–1.35) |
1.21 (1.13–1.32) |
1.29 (1.21–1.36) |

By department, workers engaged in drive-through screening (OR, 2.29; 95% CI, 1.29–4.09) and gate/entrance visitor screening (OR, 1.81; 95% CI, 1.06–3.11), as well as those working in the ward for confirmed COVID-19 cases (OR, 3.65; 95% CI, 2.26–5.90), general ward (non-COVID-19) (OR, 1.68; 95% CI, 1.08–2.44), and laboratory (OR, 6.93; 95% CI, 2.44–19.74) had statistically significant ORs for depression. However, only workers in the ward for confirmed COVID-19 cases had statistically significant ORs for anxiety (OR, 2.37; 95% CI, 1.30–4.33).
Direct contact with patients with COVID-19 in the process of treatment was directly associated with depression and anxiety; the ORs for depression and anxiety were 3.62 (95% CI, 2.24–5.83) and 2.41 (95% CI, 1.31–4.42), respectively. Likewise, dealing with COVID-19 test samples (e.g., swab or sputum) was associated with depression (OR, 5.15; 95% CI, 2.60–10.21). Exposure to random or unspecified patients was also associated with depression (OR, 1.71; 95% CI, 1.13–2.59). Workers who had been in contact with patients with COVID-19 (OR, 1.85; 95% CI, 1.35–2.54) and who had undergone COVID-19 screening (OR, 1.84; 95% CI, 1.31–2.59) had statistically significantly higher ORs for depression than those who had not. Lastly, social rejection or other negative experiences were associated with depression (OR, 3.05; 95% CI, 2.30–4.03) and anxiety (OR, 2.96; 95% CI, 2.01–4.35).
Go to :

DISCUSSION
This study was conducted in April 2020, when cases of COVID-19 were vigorously increasing in Daegu, Korea. The reported rates of depression and anxiety in the general population are 6.7%
17 and 6.2%,
18 respectively. According to Korean community survey for socio-psychological health and perceived social safety research performed 2014, the rate of high risk of anxiety shown to be 4.3%.
19 Considering those rates in general population, the rates among healthcare workers observed in this study are significantly higher. At the university hospital in question, the overall rates of depression and anxiety stood at 33% (n = 334) and 12.5% (n = 126), respectively. These rates and their ORs varied by position, department, and exposure route. The results can be interpreted as indicating that the closer healthcare workers' contact with patients with COVID-19, the higher the rates and ORs for depression, anxiety, and subjective risk.
As per a WHO report, by April 8, 22,073 healthcare workers across 53 countries had been infected with COVID-19.
20 Regarding Daegu specifically, as of March 24, there were 121 confirmed COVID-19 cases among healthcare workers, which is 4.42 per 1,000 people, whereas the cases in the general population numbered 6,620, which is 2.72 per 1,000 people.
21 Thus, it is evident that healthcare workers have higher chances of getting infected; further, they are exposed to physical and psychological burden. Accordingly, a study from Wuhan, China showed that 14.8% of healthcare workers experienced moderate to severe depression, while 12.3% had moderate to severe anxiety.
3 In comparison, the rate of depression is higher in our study. The difference might be attributable to the fact that while the Chinese study investigated 34 hospitals, including those at the fringes of Wuhan, our study focused on a single institution.
Nurses were identified to be at the highest risk of depression and anxiety, similar to other studies.
322 As of March 24, in Daegu, there were 56 confirmed cases in nurses and 51 in nurse aides, which is equivalent to 4.85 per 1,000 people and 5.14 per 1,000 people, respectively. It is notable that there were no differences in infection rates between the general population and doctors: 2.73 per 1,000 people and 2.37 per 1,000 people, respectively.
21 A potential explanation is that nurses tend to interact most closely with patients, increasing their chances of infection as compared to other groups, which is also associated with their emotional stress, ultimately resulting in the highest ORs for depression and anxiety.
Regarding factors associated with psychological impact during SARS, studies have listed position, high-risk work environments, quarantine, and perceived risk.
582324 While several factors might aggravate emotional stress, uncertainty and stigmatization seem the most significant in this regard. In our study, for instance, even for “rare” and “unknown” exposure, 23.6% and 31.3%, respectively, were identified as being at risk of depression; for anxiety, these proportions were 10.9% and 10.7%, respectively. Moreover, administrative and secretary officers, who are likely to have less contact with patients with COVID-19 compared to other job positions, had relatively high PHQ-9 and GAD-7 scores. This is comparable with another study wherein the administrative group had high PHQ-9 and GAD-7 scores.
22 These results support that hospital employees have higher levels of depression and anxiety than the general population even if they are not directly engaged in COVID-19-related work.
It is evident that not only are healthcare workers at a higher risk of exposure to COVID-19 than the general population but they are also stressed by social stigma. In fact, 18.5% of the participants answered that they had undergone COVID-19 screening, which is quite high, considering that the test rate in the general population was about 1.76% (910,822 test cases) of the total population of Korea as of May 2020.
25 In addition, 38.0% (n = 381) of the participants reported having experienced social rejection or other negative incidents. Those groups showed statistically significantly high ORs for depression and anxiety: 3.05 (95% CI, 2.30–4.03) and 2.96 (95% CI, 2.01–4.35), respectively. While these findings can be attributed to many factors, social rejection and negative experiences certainly seem to be associated with emotional stress. Moreover, psychological distress including stigmatization can persist over the long term, necessitating timely management.
26
The major limitation of our study is the use of self-reports, which can lead to over or under-reporting. Another limitation is that the participants belonged to a single institution. In addition, we considered a limited number of positions, departments, and exposure routes, which limits the generalizability of the findings. Regarding the appropriate reference group and ‘normal population’, we had certain limitation to set. It can be comparable to general population—not the ‘rarely contact’, however, the epidemiological data from the general population is from the studies conducted under the usual situation, not epidemic one. This might be one of the limitations of this study. Since this study is survey study, the response rate was quite low (38.1%), and there could be selection bias, which the more tendency to report their symptom, the more willing to answer the survey. Lastly, the cross-sectional design did not permit the comparison of basal mental health status with current status. However, we included over 1,000 healthcare workers in our assessment of emotional stress at a university hospital located at the epicenter of Korea's COVID-19 response. Also, the study was initiated immediately after the COVID-19 outbreak, which helped evaluate healthcare workers' immediate emotional response.
In the current situation of the COVID-19 pandemic, we evaluated emotional stress in healthcare workers, which was evaluated to be particularly severe in nurses and those who were directly exposed to patients. Significant levels of anxiety and depression were also identified in hospital employees without direct exposure to COVID-19. There is a need for appropriate psychological intervention measures to ensure healthy work environments for healthcare workers, who are playing a pivotal role in COVID-19 management.
Go to :







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download