This article has been
cited by other articles in ScienceCentral.
Abstract
Background
The coronavirus disease 2019 (COVID-19) has escalated to be a global threat to public health. Analysis of the use of radiology resources may render us insight regarding the public health behavior during pandemic. We measured the influence COVID-19 had on the use of radiology resources in terms of the number of examinations performed, and turnaround time for portable radiography.
Methods
This study was conducted at a tertiary hospital located in area where the prevalence of COVID-19 infection was low (0.01%). We compared the number of radiology examinations 1) before pandemic (in 2019) vs. during peak of pandemic (January to March 2020), and 2) before pandemic vs. after the peak of pandemic (April to June 2020) via t-tests. We repeated similar analyses for subgroups as follows: gender, age, department (outpatient, inpatient, emergency, screening), body parts, and modality. We also performed a survey of radiologic technologists regarding the turnaround time and rate-limiting step of portable radiography for patients with and without suspicion or confirmation of COVID-19.
Results
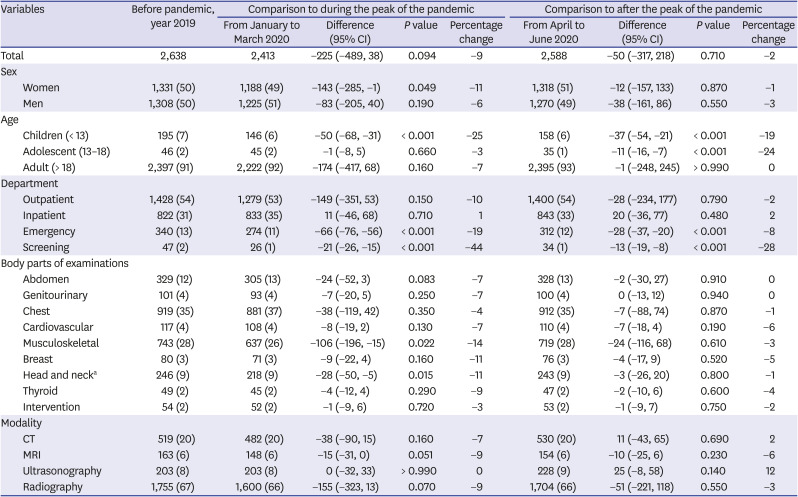
Although not statistically significant, the daily number of examinations during the peak of pandemic decreased by 9 percentage points (2,638 vs. 2,413; difference [95% CI], −225 [−489, 38]; P = 0.094). The percentage change was especially notable for children, emergency, and screening department (25, 19, and 44 percentage points, respectively). After the peak of the pandemic, the number of examinations increased back to near the pre-pandemic level (2,638 vs. 2,588; −50 [−317, 218]; P = 0.71). The turnaround time for portable radiography tended to be longer for patients with suspicion or confirmation of COVID-19, with donning personal protective equipment being the major rate-limiting step.
Conclusion
The number of examinations decreased during the pandemic, reflecting the tendency of the public to refrain from seeking medical care even in a community of low infection risk. Nevertheless, burden of healthcare providers may not have decreased as much, considering longer turnaround time required for COVID-19 related examinations.
Keywords: Health Resources, Infections, COVID-19, Pandemics, Korea
INTRODUCTION
Ever since December 2019 when there was an initial outbreak in Wuhan, China, the coronavirus disease 2019 (COVID-19) has quickly spread and escalated to be a global threat to public health.
12 The number of patients confirmed to have the disease has surpassed 17 million, claiming the lives of more than 668,910 patients worldwide as of August 1st, 2020.
3
The pandemic is already having a profound impact on the medical community, although its long-term implications are yet difficult to anticipate. Some hospitals located in areas where outbreaks were clustered, such as Wuhan, China, or Daegu, Korea, have been stretched beyond their capacity, overwhelmed with demands for medical care related to COVID-19.
4 Burnout of involved healthcare providers has been and is still of grave concern.
5 Hospitals in other regions better-positioned in terms of outbreak size or hospital resources have also been affected financially by decreased revenue.
6 Fear of contracting the virus has daunted patients' healthcare-seeking behavior in general, leading to the postponement of hospital visits even for life-threatening emergencies such as stroke or heart attack.
78 Some hospitals had to shut down their outpatient or emergency departments,
6 either voluntarily to create additional staffing and inpatient capacity for the COVID-19, or mandatorily for quarantine.
Our goal amidst the pandemic would be to prevent any operational crisis by spreading out and keeping the demand for medical resources within the capacity of the system. It requires efforts of the medical community in liaison with the government in many aspects, such as in preparing contingency staffing schedules, protocols regarding medical resource allocation not only within a hospital but in-between hospitals,
9 or providing public guidance regarding hospital visits for both COVID-related and nonrelated illnesses. All these would be dependent on our ability to anticipate public health behavior and to accurately assess the buffer resources that could be mobilized in case of emergencies.
As an action for such ‘preparedness,’ we may quantitatively assess the impact COVID-19 had on the use of radiology resources. Radiology examinations are involved in almost all patients' workup regardless of the ordering department or presenting symptoms, serving diverse medical needs from annual screening to treatment response evaluation for malignancy. Turnaround time for radiologic examinations would probably be longer in pandemics due to measures taken for infection control,
10 such as donning and doffing personal protective equipment or room sterilization. Thus, analysis of the use of radiology resources may render us some insight regarding the use of overall medical resources and public health behavior during the pandemic.
1112
In this study, we analyzed the influence COVID-19 had on the use of radiology resources in a tertiary hospital in Korea, in terms of the change in the daily number of radiology examinations performed, and turnaround time for portable radiography.
METHODS
Hospital setting
The study was conducted at a tertiary hospital located in Korea. More than 2,660 healthcare providers including approximately 700 clinicians are working in this 1,324-bed hospital as of August 1
st, 2020. In the department of radiology, there are 62 radiologists including 48 attending, 128 radiologic technologists, and 32 nurses. Our main catchment area has a population of approximately 14 million people.
13 However, a considerable portion of our patients is from all over the nation.
COVID-19 nationwide and in the catchment area
The number of patients confirmed to have COVID-19 in Korea is 14,336, as of August 1st, 2020.
14 The first case of COVID-19 in Korea was confirmed on January 20th. The first wave of the outbreak came with a rapid upsurge, with more than 600 cases newly diagnosed daily until early March. Since then, the spread slowed down, with newly diagnosed cases kept mostly below 80 per day. In Gyeonggi-do where our hospital is located, there was no significant clustering of the cases, with about 1,553 cumulated cases in the region (0.01% out of a population of 14 million) as of August 1st, 2020. Except for a week (from March 9th to 15th) when our pain management division of the department of anesthesiology was shut down due to COVID-19 infection of one of the department's employees, our center did not close or reduce any of our services. Except for that one employee, none of the workers in our center has been confirmed with COVID-19, including those who were in close contact with the employee.
Examinations in the Department of Radiology
We searched our electronic database to identify the examinations performed in the Department of Radiology from January 1st, 2019 to June 30th, 2020. We used the examinations in the year 2019 as those performed ‘before the pandemic,’ from January to March 2020 as ‘during the peak of the pandemic,’ and from April to June 2020 as ‘after the peak of pandemic.’
In our center, the department of nuclear medicine operates independently from the Department of Radiology. Thus, we did not include nuclear medicine imaging such as positron emission tomography or bone scan. The majority of ultrasonography was performed in the Department of Radiology, except for transvaginal ultrasonography performed by the Department of Obstetrics and Gynecology, and a relatively minute number of abdominal and thyroid ultrasonography performed by physicians of other departments. All examinations using X-ray, except for coronary angiography and a small portion of other vascular angiographies, were performed in the department of radiology. All magnetic resonance imaging (MRI) was performed in the Department of Radiology.
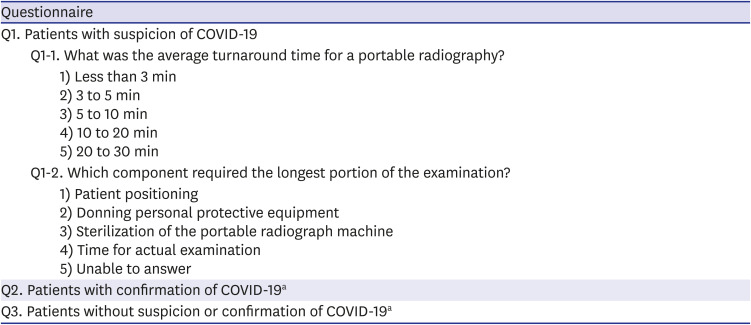
Online survey
We performed an online survey regarding the turnaround time of portable radiography for patients 1) with suspicion, 2) with confirmation, and 3) without suspicion or confirmation of COVID-19 infection. We defined the turnaround time as the interval from the completion of one patient's examination to the initiation of another patient's examination.
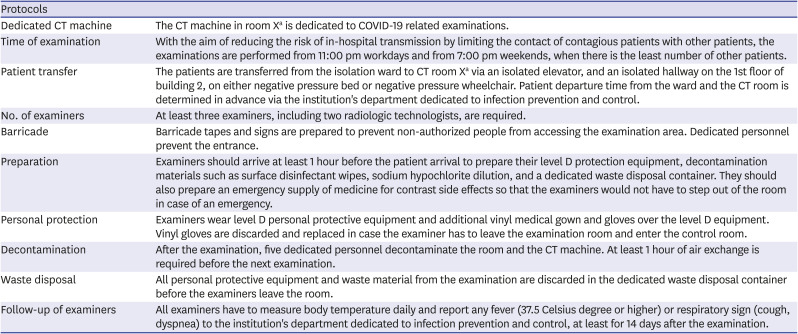
15 This would include the time used for patient positioning or donning personal protective equipment for infection prevention. After the COVID-19 pandemic, all members of our radiology department had to abide by the protocols entailing various measures for infection control, from controlling patient transfer route to minimize contact with other patients, to sterilizing the room and machine after each examination.
Table 1 shows our protocol for CT examination. Thus, we expected that the turnaround time for radiology examinations would have increased meaningfully after the COVID-19 pandemic. Via online survey, we invited all radiologic technologists who were assigned to shifts involving portable radiography examinations of patients with suspicion or confirmation of COVID-19. We asked questions regarding the average turnaround time of portable radiography, and a component requiring the longest portion of the examination (i.e., rate-limiting step) (
Table 2). The survey was anonymous, and only those who agreed to participate responded. There were no financial or other rewards for participation.
Table 1
Protocol for CT examination of patients with COVID-19
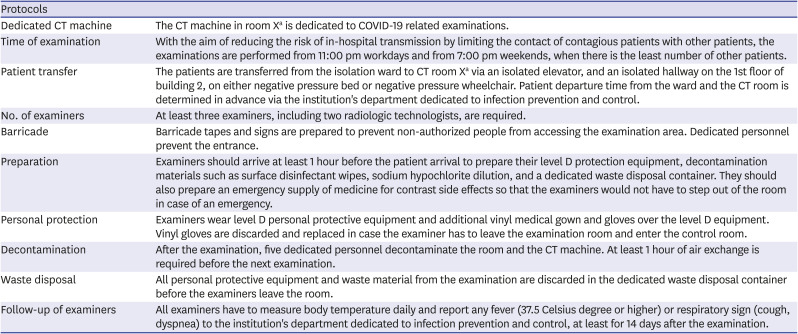
|
Protocols |
|
Dedicated CT machine |
The CT machine in room Xa is dedicated to COVID-19 related examinations. |
|
Time of examination |
With the aim of reducing the risk of in-hospital transmission by limiting the contact of contagious patients with other patients, the examinations are performed from 11:00 pm workdays and from 7:00 pm weekends, when there is the least number of other patients. |
|
Patient transfer |
The patients are transferred from the isolation ward to CT room Xa via an isolated elevator, and an isolated hallway on the 1st floor of building 2, on either negative pressure bed or negative pressure wheelchair. Patient departure time from the ward and the CT room is determined in advance via the institution's department dedicated to infection prevention and control. |
|
No. of examiners |
At least three examiners, including two radiologic technologists, are required. |
|
Barricade |
Barricade tapes and signs are prepared to prevent non-authorized people from accessing the examination area. Dedicated personnel prevent the entrance. |
|
Preparation |
Examiners should arrive at least 1 hour before the patient arrival to prepare their level D protection equipment, decontamination materials such as surface disinfectant wipes, sodium hypochlorite dilution, and a dedicated waste disposal container. They should also prepare an emergency supply of medicine for contrast side effects so that the examiners would not have to step out of the room in case of an emergency. |
|
Personal protection |
Examiners wear level D personal protective equipment and additional vinyl medical gown and gloves over the level D equipment. Vinyl gloves are discarded and replaced in case the examiner has to leave the examination room and enter the control room. |
|
Decontamination |
After the examination, five dedicated personnel decontaminate the room and the CT machine. At least 1 hour of air exchange is required before the next examination. |
|
Waste disposal |
All personal protective equipment and waste material from the examination are discarded in the dedicated waste disposal container before the examiners leave the room. |
|
Follow-up of examiners |
All examiners have to measure body temperature daily and report any fever (37.5 Celsius degree or higher) or respiratory sign (cough, dyspnea) to the institution's department dedicated to infection prevention and control, at least for 14 days after the examination. |
Table 2
Survey regarding turnaround time and rate-limiting step for portable radiography
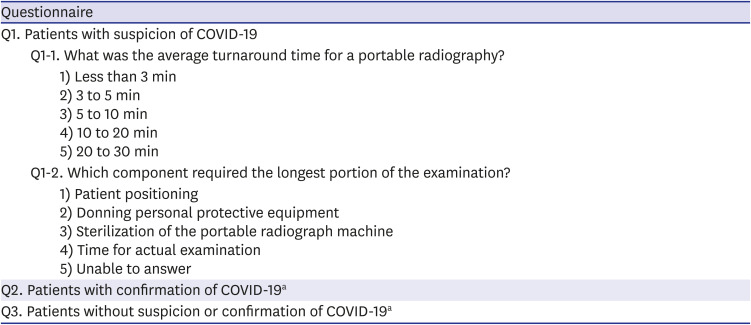
|
Questionnaire |
|
Q1. Patients with suspicion of COVID-19 |
|
Q1-1. What was the average turnaround time for a portable radiography? |
|
|
1) Less than 3 min |
|
|
2) 3 to 5 min |
|
|
3) 5 to 10 min |
|
|
4) 10 to 20 min |
|
|
5) 20 to 30 min |
|
Q1-2. Which component required the longest portion of the examination? |
|
|
1) Patient positioning |
|
|
2) Donning personal protective equipment |
|
|
3) Sterilization of the portable radiograph machine |
|
|
4) Time for actual examination |
|
|
5) Unable to answer |
|
Q2. Patients with confirmation of COVID-19a
|
|
Q3. Patients without suspicion or confirmation of COVID-19a
|
Statistical analysis
Two radiologists (H.Y.K., and J.C. with five and four years of research experience, respectively) planned all analyses before data collection. A statistician (S.L., with three years of experience) performed all the analyses.
We compared the average daily number of radiology examinations 1) before the pandemic (in 2019) vs. during the peak of the pandemic (January to March 2020), and 2) before the pandemic (in 2019) vs. after the peak of the pandemic (April to June 2020). We used the
t-tests for the comparisons and calculated the differences with their 95% confidence intervals (CIs). We additionally calculated the percentage change in the average daily number of radiology examinations, which we defined as the change in the average daily number (the number during the peak or after the peak of pandemic subtracted by that before the pandemic), divided by the average daily number of radiology examinations before the pandemic. We repeated similar analyses for each subgroup as follows: gender; age (children [below 13], adolescents [between 13 and 18 years old], and adults [above 18 years old]); department (outpatient, inpatient, emergency, screening); body parts (i.e., subspecialty) of examinations (abdomen, genitourinary, chest, cardiovascular, musculoskeletal, breast, head and neck, thyroid, and intervention); and modality (computed tomography [CT], MRI, ultrasonography, radiography). We opted not to adjust for multiple comparisons,
16 as we deemed that overall results showing 95% CIs were more important than mere
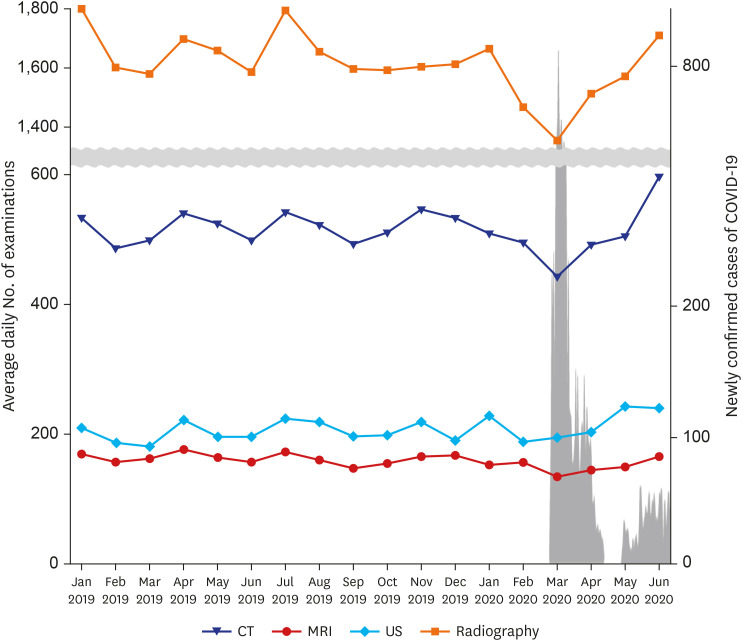
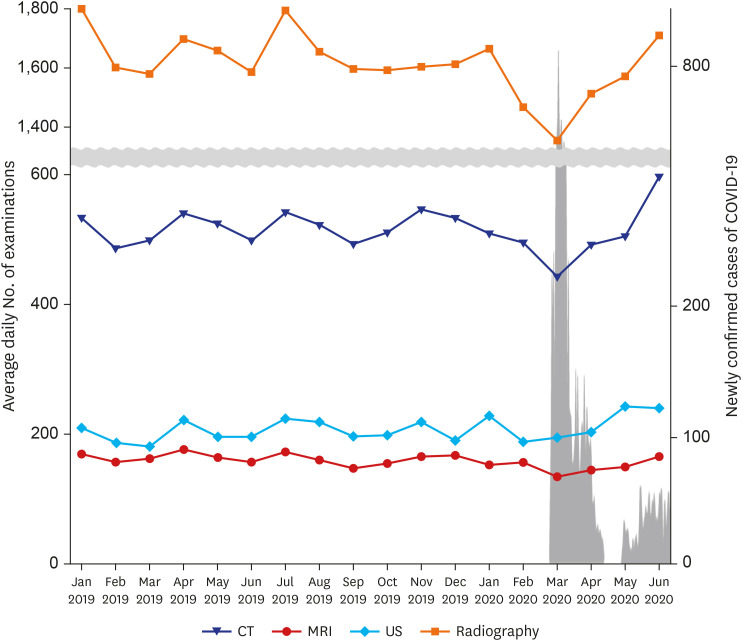
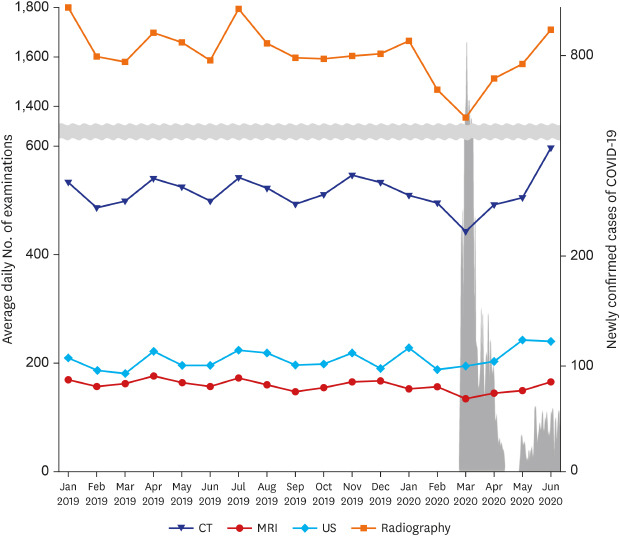
P values. Finally, we drew a line graph to visually represent the change in the number of radiology examinations, along with the change in the nationwide number of newly confirmed cases across the timeline from January 2019 to June 2020.
We did not perform any statistical comparison for the turnaround time of portable radiography, as we deemed that our sample size was too small to render any meaningful result. Instead, we analyzed the results qualitatively via stacked bar charts.
We used R software (version 3.6.3). We considered a two-sided P value less than 0.05 as statistically significant.
Ethics statement
The Institutional Review Board of Seoul National University Bundang Hospital waived patient informed consent for the use of the patient data, and approved the study including an online survey (approval No. B-2006-616-007 and B-2007-625-301).
RESULTS
Patients
A total of 512,322 patients underwent 1,360,182 radiology examinations from the year 2019 to June 2020. They were 241,602 men (mean age ± standard deviation, 54.1 ± 22.0 years) and 270,720 women (54.8 ± 20.3 years). There were 36,146 children of age under 13 (5.6 ± 4.0 years), and 8,276 adolescents of age between 13 and 18 years old (15.5 ± 1.5 years). A total of 171 patients who were confirmed as having COVID-19 underwent radiology examination(s).
Comparison of radiology examinations
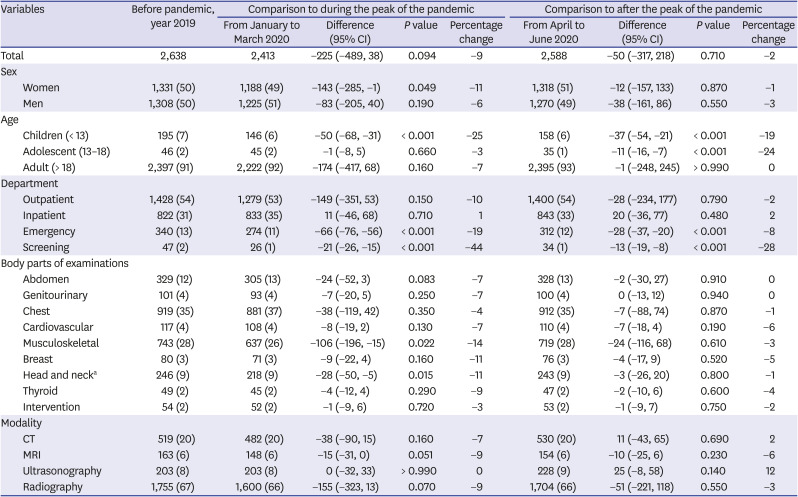
Although not statistically significant, the daily number of examinations during the peak of the pandemic decreased by nine percentage points (2,638 vs. 2,413; difference [95% CI], −225 [−489, 38];
P = 0.094) (
Table 3 and
Fig. 1). The difference was statistically significant for children (−25 percentage points; 195 vs. 146; −50 [−68, −31];
P < 0.001), emergency department (−19 percentage points; 340 vs. 274; −66 [−76, −56];
P < 0.001), and screening department (−44 percentage points; 47 vs. 26; −21 [−26, −15];
P < 0.001). Among body parts, the difference was notable in musculoskeletal, breast, and head and neck examinations (decreased by 14, 11, and 11 percentage points, respectively). In comparison, chest examinations decreased by 4 percentage points. After the peak of the pandemic, the number of examinations increased back to near the pre-pandemic level (2,638 vs. 2,588; −50 [−317, 218];
P = 0.71) (
Table 3 and
Fig. 1).
Table 3
Comparison of the average daily number of radiology examinations before and after the COVID-19 pandemic
|
Variables |
Before pandemic, year 2019 |
Comparison to during the peak of the pandemic |
Comparison to after the peak of the pandemic |
|
From January to March 2020 |
Difference (95% CI) |
P value |
Percentage change |
From April to June 2020 |
Difference (95% CI) |
P value |
Percentage change |
|
Total |
2,638 |
2,413 |
−225 (−489, 38) |
0.094 |
−9 |
2,588 |
−50 (−317, 218) |
0.710 |
−2 |
|
Sex |
|
|
|
|
|
|
|
|
|
|
Women |
1,331 (50) |
1,188 (49) |
−143 (−285, −1) |
0.049 |
−11 |
1,318 (51) |
−12 (−157, 133) |
0.870 |
−1 |
|
Men |
1,308 (50) |
1,225 (51) |
−83 (−205, 40) |
0.190 |
−6 |
1,270 (49) |
−38 (−161, 86) |
0.550 |
−3 |
|
Age |
|
|
|
|
|
|
|
|
|
|
Children (< 13) |
195 (7) |
146 (6) |
−50 (−68, −31) |
< 0.001 |
−25 |
158 (6) |
−37 (−54, −21) |
< 0.001 |
−19 |
|
Adolescent (13–18) |
46 (2) |
45 (2) |
−1 (−8, 5) |
0.660 |
−3 |
35 (1) |
−11 (−16, −7) |
< 0.001 |
−24 |
|
Adult (> 18) |
2,397 (91) |
2,222 (92) |
−174 (−417, 68) |
0.160 |
−7 |
2,395 (93) |
−1 (−248, 245) |
> 0.990 |
0 |
|
Department |
|
|
|
|
|
|
|
|
|
|
Outpatient |
1,428 (54) |
1,279 (53) |
−149 (−351, 53) |
0.150 |
−10 |
1,400 (54) |
−28 (−234, 177) |
0.790 |
−2 |
|
Inpatient |
822 (31) |
833 (35) |
11 (−46, 68) |
0.710 |
1 |
843 (33) |
20 (−36, 77) |
0.480 |
2 |
|
Emergency |
340 (13) |
274 (11) |
−66 (−76, −56) |
< 0.001 |
−19 |
312 (12) |
−28 (−37, −20) |
< 0.001 |
−8 |
|
Screening |
47 (2) |
26 (1) |
−21 (−26, −15) |
< 0.001 |
−44 |
34 (1) |
−13 (−19, −8) |
< 0.001 |
−28 |
|
Body parts of examinations |
|
|
|
|
|
|
|
|
|
|
Abdomen |
329 (12) |
305 (13) |
−24 (−52, 3) |
0.083 |
−7 |
328 (13) |
−2 (−30, 27) |
0.910 |
0 |
|
Genitourinary |
101 (4) |
93 (4) |
−7 (−20, 5) |
0.250 |
−7 |
100 (4) |
0 (−13, 12) |
0.940 |
0 |
|
Chest |
919 (35) |
881 (37) |
−38 (−119, 42) |
0.350 |
−4 |
912 (35) |
−7 (−88, 74) |
0.870 |
−1 |
|
Cardiovascular |
117 (4) |
108 (4) |
−8 (−19, 2) |
0.130 |
−7 |
110 (4) |
−7 (−18, 4) |
0.190 |
−6 |
|
Musculoskeletal |
743 (28) |
637 (26) |
−106 (−196, −15) |
0.022 |
−14 |
719 (28) |
−24 (−116, 68) |
0.610 |
−3 |
|
Breast |
80 (3) |
71 (3) |
−9 (−22, 4) |
0.160 |
−11 |
76 (3) |
−4 (−17, 9) |
0.520 |
−5 |
|
Head and necka
|
246 (9) |
218 (9) |
−28 (−50, −5) |
0.015 |
−11 |
243 (9) |
−3 (−26, 20) |
0.800 |
−1 |
|
Thyroid |
49 (2) |
45 (2) |
−4 (−12, 4) |
0.290 |
−9 |
47 (2) |
−2 (−10, 6) |
0.600 |
−4 |
|
Intervention |
54 (2) |
52 (2) |
−1 (−9, 6) |
0.720 |
−3 |
53 (2) |
−1 (−9, 7) |
0.750 |
−2 |
|
Modality |
|
|
|
|
|
|
|
|
|
|
CT |
519 (20) |
482 (20) |
−38 (−90, 15) |
0.160 |
−7 |
530 (20) |
11 (−43, 65) |
0.690 |
2 |
|
MRI |
163 (6) |
148 (6) |
−15 (−31, 0) |
0.051 |
−9 |
154 (6) |
−10 (−25, 6) |
0.230 |
−6 |
|
Ultrasonography |
203 (8) |
203 (8) |
0 (−32, 33) |
> 0.990 |
0 |
228 (9) |
25 (−8, 58) |
0.140 |
12 |
|
Radiography |
1,755 (67) |
1,600 (66) |
−155 (−323, 13) |
0.070 |
−9 |
1,704 (66) |
−51 (−221, 118) |
0.550 |
−3 |
Fig. 1
Line graphs showing the change in the average daily number of radiology examinations from January 2019 to June 2020. The line graph with gray shading shows change in the daily nationwide number of newly-confirmed COVID-19 cases, with a peak in March 2020.
COVID-19 = coronavirus disease 2019, CT = computed tomography, MRI = magnetic resonance imaging.
Online survey
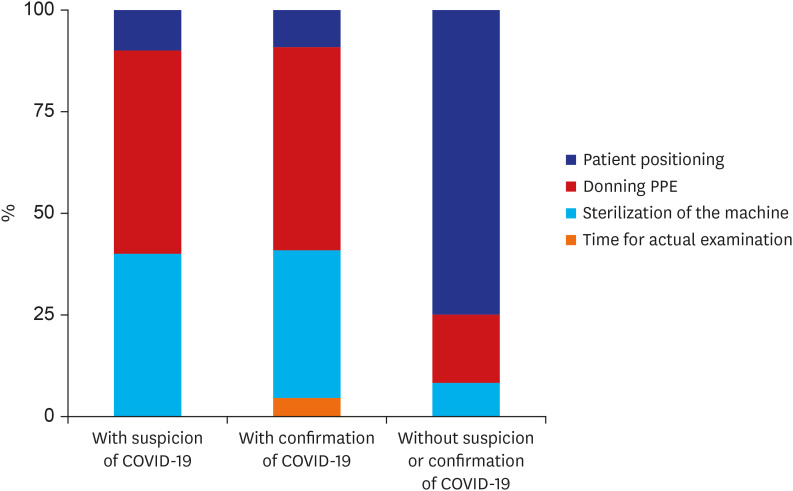
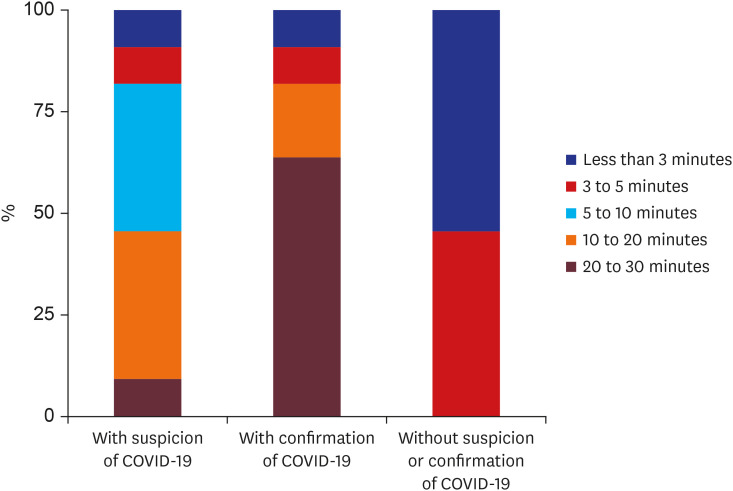
11 radiologic technologists (39% [11/28]) returned their responses. The turnaround time for portable radiography tended to be longer for patients with suspicion or confirmation of COVID-19, compared to those without COVID-19 (
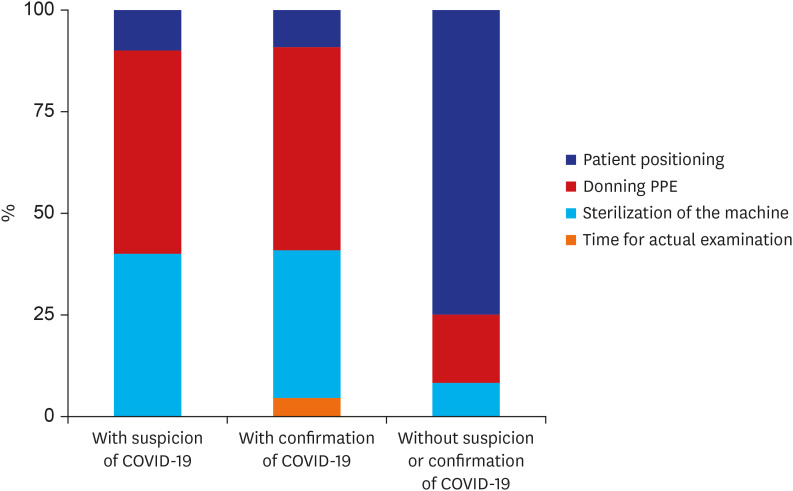
Fig. 2). More than 50% of the responders answered that the turnaround time for portable radiography in patients with confirmation of COVID-19 was 20 to 30 minutes. In comparison, more than 50% responded that the turnaround time for patients without suspicion or confirmation of COVID-19 was less than 3 minutes. ‘Donning personal protective equipment’ was most frequently selected as the rate-limiting step in the examinations of patients with suspicion or confirmation of COVID-19, followed by ‘sterilization of portable radiograph machines’ (
Fig. 3).
Fig. 2
Stacked bar charts showing the responses of radiologic technologists regarding the turnaround time of portable radiography examination for patients with suspicion, confirmation of COVID-19, and without suspicion or confirmation of COVID-19.
COVID-19 = coronavirus disease 2019.
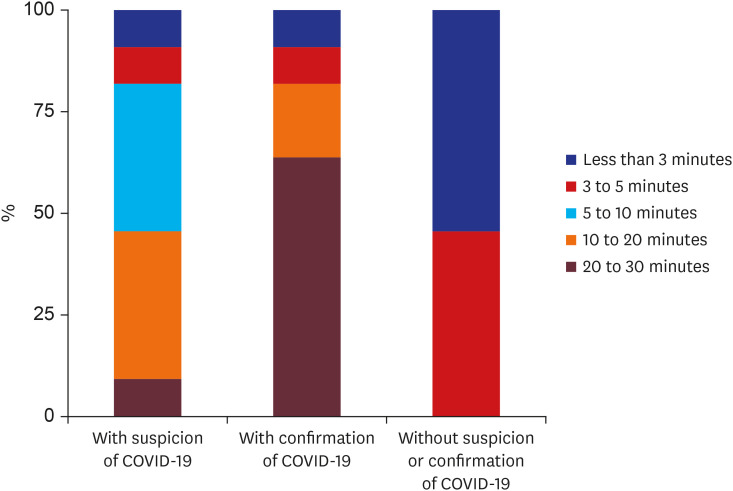
Fig. 3
Stacked bar charts showing responses of radiologic technologists regarding the rate-limiting step of portable radiography examination for patients with suspicion, confirmation of COVID-19, and without suspicion or confirmation of COVID-19.
PPE = personal protective equipment, COVID-19 = coronavirus disease 2019.
DISCUSSION
We showed that the COVID-19 pandemic caused a notable decrease in the number of radiology examinations enacted in a tertiary hospital, located in a geographic region where the infection occurred only sporadically. As radiology examinations are involved in almost all patients' workup, the use of the radiology resources may indirectly reflect the use of overall medical resources.
Our results have important implications as follows. First, a notable reduction in the number of radiology examinations during the peak of the pandemic (9 percentage points) showed the public behavior of avoiding hospital visits, potentially delaying necessary and urgent medical care.
17 The reduction in radiology examinations was noted not only for patients presenting to the emergency department (19 percentage points), but also for patients undergoing routine screening (44 percentage points). A significant reduction was also noted for children (25 percentage points). This trend is consistent with a troubling report from Hong Kong that the time from symptom onset to first medical contact in patients with acute myocardial infarction was significantly increased after the pandemic.
8 Relatively lower reduction of chest examinations (4 percentage points) would be attributable to increased clinical demand for examinations such as chest X-ray used for screening or follow-up of COVID-19 infection. National health authorities will need to formulate and implement guidelines regarding hospital visits in times of pandemic, ideally stratified according to patient risk factors. Patients for whom the risk of delayed workup is higher than the risk of contracting COVID-19 should be encouraged to seek medical care. Whether patients will adhere to such guidance will depend on their trust for the government and medical community to control the infection while delivering objective and neutral information regarding the infection risk. Our result showing the recovery of radiology examinations back to almost the pre-pandemic level is a promising sign of the public trust in the national health system and our center. Second, the reduction in the number of radiology examinations during the peak of the pandemic may have created some buffer resources to be mobilized for infection control, while it also meant decreased revenue for the hospital.
18 We set an example of how the medical community should assess past events to prepare for future outbreaks that will probably ensue. Quantitative assessment of the impact of the pandemic on medical resources such as radiology examinations allows us to gauge the extent to which a medical center may mobilize its medical resources in case of an emergency. This mobilization is not just for within a hospital but also potentially for other centers at risk of operational crisis.
19 Third, the pandemic may also affect resident training. Our center recovered from the reduction quickly, but there may be centers worldwide where the impact of the COVID-19 is prolonged enough to affect the resident training.
20 This may be due to the reduction in the number of cases the residents encounter, or because the residents are so overwhelmed by the medical care related to COVID-19 that they cannot receive a well-rounded education.
Although there was a notable reduction in the number of radiology examinations enacted in our center, this does not mean that the workload of the healthcare providers had decreased during the period. A few clinicians and radiologic technologists had to be quarantined due to their traveling history or close contact with confirmed patients. The on-call schedule had to be modified accordingly, increasing the burden for the remaining people. We had to assign additional nurses at the reception area to screen patients for symptoms or travel history to regions of widespread transmission. Our survey shows that the turnaround time for portable radiography was increased due to downtime during which the room or machine was disinfected, and the time used for donning and doffing personal protective equipment. This applied not only to patients with confirmation but also to those with suspicion of COVID-19. We also had to spend non-negligible time on online conferences to discuss hospital policies regarding the management of patients with suspicion or confirmation of COVID-19. Now that the number of radiology examinations has returned to almost the pre-pandemic level, extra resources devoted to infection control have probably increased the overall burden on our healthcare providers compared to that before the pandemic.
Our study had important weaknesses. First, it was a single-center study from a geographic region where the prevalence of COVID-19 infection was low, thus raising concern for generalizability of the results. Moreover, the study was conducted during short time period at the beginning of the pandemic, not able to reflect long-term consequences. We would need future studies using nationwide data from a longer time period, especially from geographic regions where large outbreaks were clustered. Second, the survey of our radiologic technologists may have been biased as it was based on their recall of memory. Moreover, only those who responded were included, which may have caused selection bias. Third, we did not analyze the actual clinical outcome (e.g., the number of adverse outcomes caused by delayed cancer diagnosis or treatment for acute myocardial infarction) associated with the reduction in the number of radiology examinations.
The number of radiology examinations decreased during the pandemic, reflecting the tendency of the public to refrain from seeking medical care even in a community of low infection risk. Nevertheless, overall burden of healthcare providers may not have decreased as much, considering longer turnaround time required for COVID-19 related examinations. Our results, although acquired from a specific locale, could be used as the foundation for further efforts on formulating guidelines and protocols for future outbreaks.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download