Discussion
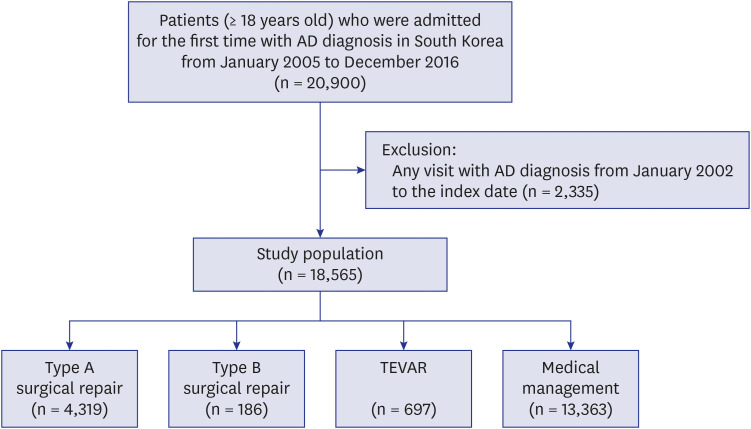
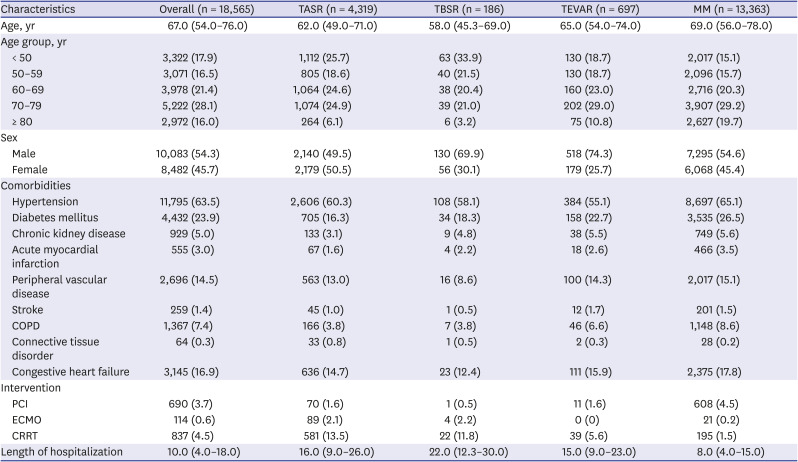
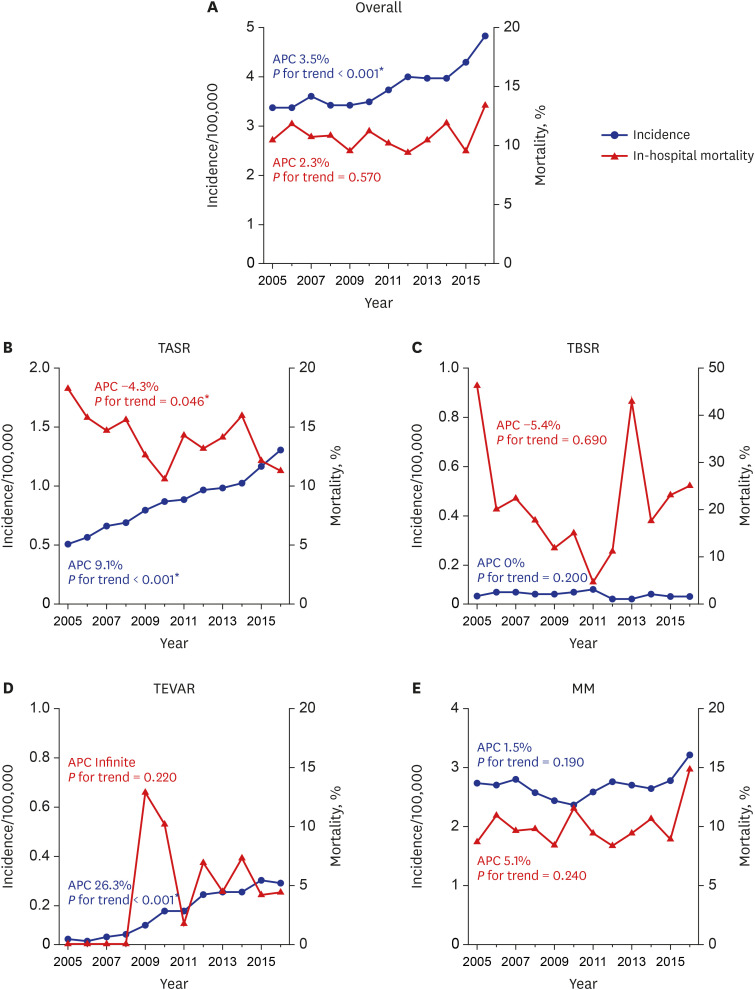
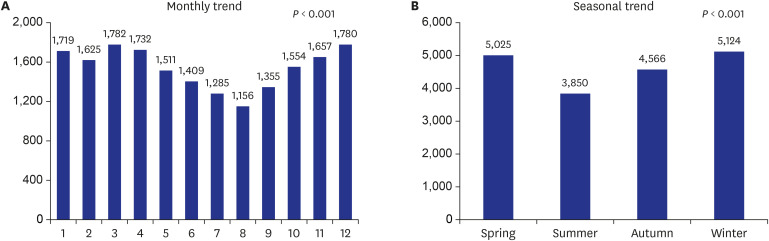
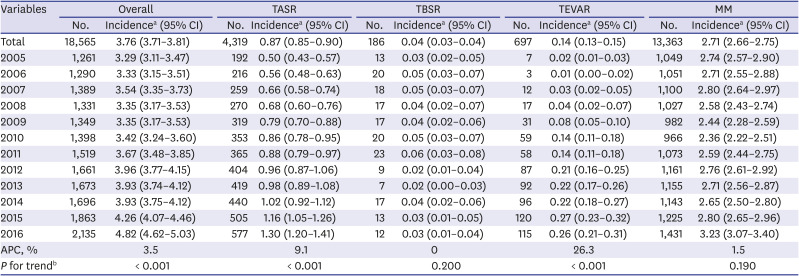
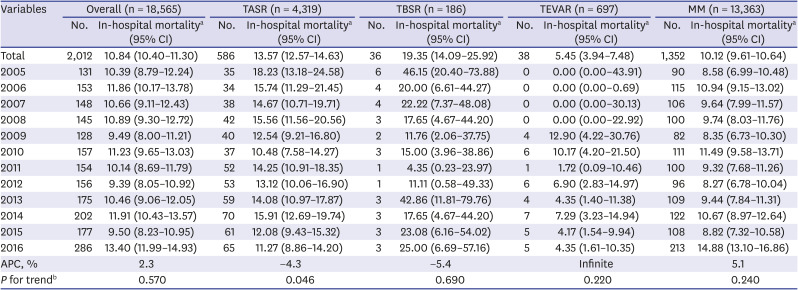
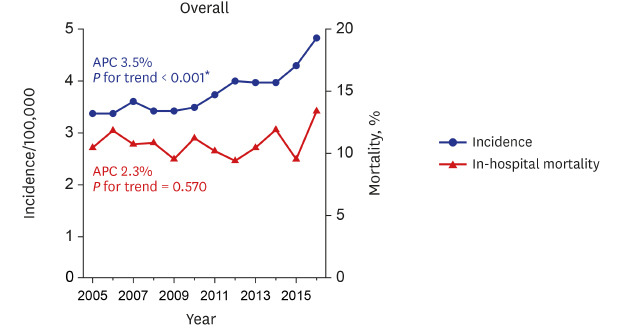
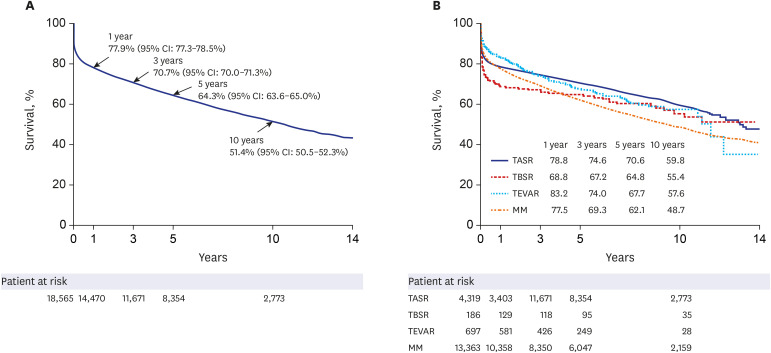
AD is an acute condition with an extremely high morbidity rate, and quantifying its true incidence remains difficult. This study defined and classified the true incidence of thoracic AD using nationwide data from Korea. Among 18,565 patients who were newly diagnosed with AD from January 2005 to December 2016, the incidence rate of AD was 3.76 per 100,000 person-years. The annual incidence rate gradually increased during the study period. The overall in-hospital mortality rate was 10.84% and remained consistent during the study period, whereas the TASR in-hospital mortality rate significantly decreased. An older age, the female sex, hypertension, and chronic kidney disease were independent risk factors for in-hospital mortality.
This study, which involved a large retrospective population-based analysis of AD, is comparable to other previous contemporary studies.
1245 In a rare previous Asian nationwide population-based study, Yeh et al.
12 demonstrated that the annual incidence rate of AD was 5.6 per 100,000 person-years, and that the average annual incidence of patients treated surgically for type A AD was 1.44 per 100,000 person-years in Taiwan. Additionally, in a recent German multi-institutional retrospective study, Wundram et al.
15 demonstrated that the emergency department incidence of acute type A AD was 5.24 per 100,000 person-years. However, this group only investigated the prevalence rate and did not address the treatment outcomes. Additionally, since the prevalence rate was calculated using the emergency department incidence rate as the denominator rather than the population-based incidence rate,
15 it is believed that the number could be higher. In a recent study investigating the surgical outcomes of type A acute AD based on the Japan Cardiovascular Surgery Database, Abe and colleagues demonstrated that the annual incidence rate of surgery for acute type A AD was approximately 1.16 per 100,000 person-years.
16 The incidence rates of overall AD and TASR in our study were 3.76 and 0.87 per 100,000 person-years, and these results revealed the lower incidence compared with that in studies in other countries.
121516 In our study, all hospitalizations through the emergency room were included. However, we did not include patients who died in the emergency room or during transport to a different hospital because the date of the first admission with an AD diagnosis was defined as the index date. In total, 619 people were excluded during the study period, which could represent a limitation leading to an underestimation of the incidence rate. If included, the incidence rate was slightly higher at 3.89/100,000/year. However, since most patients with AD are hospitalized, we significantly confirmed the outcome by epidemiology and the treatment method by focusing on AD patients who were hospitalized.
In our results, the incidence rate of AD exhibited an increasing trend, and the APC was 3.5%. In particular, the incidence rates of TASR and TEVAR significantly increased over time in our study, which may be due to the development of the emergency transport system because living AD patients can be transferred to a hospital more rapidly.
17 Additionally, the increase in the TEVAR group may be ascribed to the increasing trend in endovascular interventions.
21819
In this study, the patients with thoracic AD were predominantly in their 60s and 70s. This distribution is similar to that reported in previous publications.
124 In previous studies, the male-to-female ratio was approximately 2:1,
124 however, the sex ratio in the current study was 54.3:45.7. This male-to-female ratio is comparable to that reported in a previously published study based on the Korean multi-center registry of acute aortic syndrome.
20
Due to the limitations of the diagnostic coding system regarding the classification of types A and B, in this study, AD was classified into TASR, TBSR, TEVAR, and MM as described in a previously published study.
2 McClure and colleagues stated that if a patient was alive at the time of discharge after medical treatment, the patient was classified as having type B AD. If a patient died during hospital admission, they assessed the records of the Office of the Registrar General – Death Database to identify the primary cause of death and classify the patient as having type A or B AD.
1 However, in some cases, if a patient was diagnosed with acute retrograde type A AD with retrograde extension from an intimal tear in the descending aorta into the ascending aorta, he (or she) could survive and be alive at discharge with a favorable prognosis,
21 and it is thought that there is a risk of misclassification.
According to our results, the in-hospital mortality rates of all patients and those in the TASR, TBSR, TEVAR and MM subgroups were 10.84%, 13.57%, 19.35%, 5.45% and 10.12%, respectively. These findings are comparable to the results reported in a previous study in which Zimmerman and colleagues demonstrated mortality trends in hospitalized AD patients in the general United States population (2003–2012).
2
Despite the observed increasing trend in AD, the mortality rate did not increase, which is comparable to the findings of previous studies.
2713 Our findings demonstrate that the in-hospital mortality rate in the TASR subgroup significantly decreased over time. This result is comparable to a recent study investigating the surgical outcomes of type A acute AD based on the Japan Cardiovascular Surgery Database. In this previous study, the overall operative mortality rate was 9.5% and showed a decreasing trend.
16
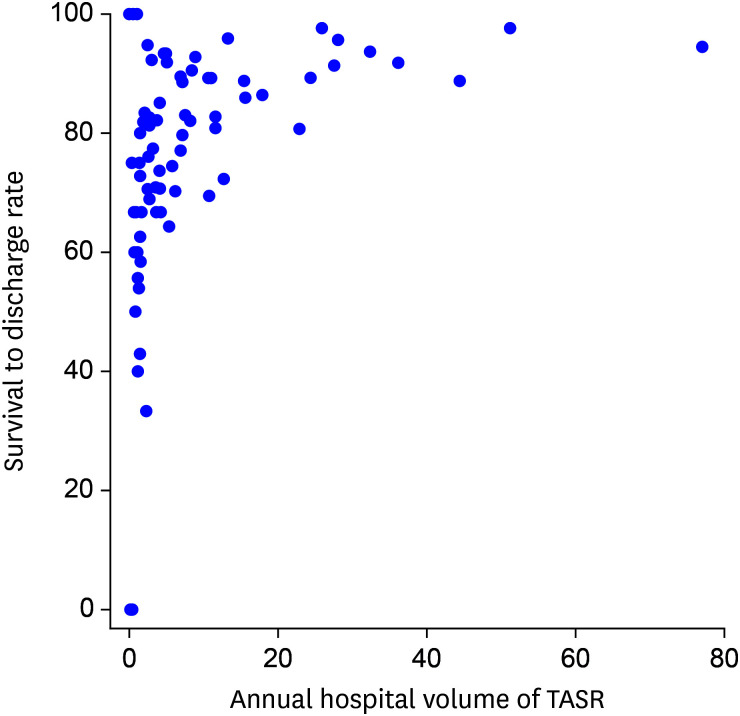
We investigated the treatment outcome of TASR according to the hospital volume (
Fig. 4), and nine of 10 centers with an average of 20 surgeries or more per year had a survival rate to hospital discharge exceeding 88%. This finding does not imply that the hospital volume and the outcome of TASR are directly proportional but rather suggests that a center with a volume of an average of 20 surgeries or more per year has acceptable outcomes.
Although the 30-day and 1-year mortality rates of the TASR subgroup did not significantly decrease, the overall trend was decreasing. Our findings suggest that advances in surgical skills, including standardized cannulation methods, neuroprotective techniques, a formalized series of main procedures, pre- and postoperative management and the establishment of a multidisciplinary team, may be major factors contributing to the improved outcomes.
22
According to our results, the 30-day mortality rates of all patients and those in the TASR, TBSR, TEVAR and MM subgroups were 13.02%, 15.07%, 20.43%, 8.18% and 12.51%, respectively. In this study, the median length of hospitalization of all patients was 10.0 days, and the 30-day mortality rates of all patients and those in the TASR subgroup were higher than the in-hospital mortality rates. The median hospital stay in our study was longer than the hospitalization of 16 days in the International Registry of Acute Aortic Dissection study.
3 Close observation of AD patients may be necessary after hospital discharge to improve early outcomes. In a recent study based on the nationwide Japanese Registry of All Cardiac and Vascular Disease database, Yamaguchi and colleagues demonstrated that the median hospital stay among patients who survived was 28 days in type A AD and 22 days in type B AD due to rehabilitation and nursing care during the same hospitalization period.
2324
The 1-year survival rates of the TBSR and TEVAR subgroups were 68.8% and 83.2%, respectively. After a certain period, the survival rates of the TBSR and TEVAR subgroups became similar. The Kaplan-Meier curve of TEVAR is steeper than that of TBSR after the first year. Patients with type B AD undergoing surgical repair are at a high risk of morbidity and mortality during the acute phase because of catastrophic conditions, such as aortic rupture or impending rupture. Additionally, TEVAR carries a risk of the need for reintervention during long-term follow-up.
1819
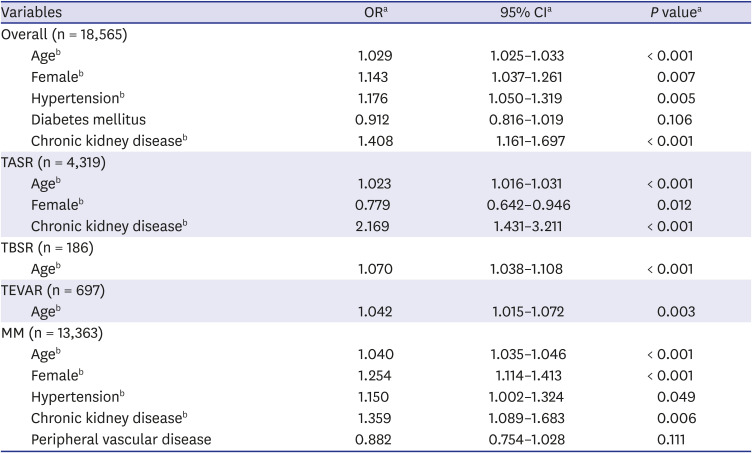
An older age was the most important factor predicting in-hospital mortality in all treatment groups, including the whole population. Obviously, age can affect treatment due to the patient’s general condition or underlying diseases. The female sex, hypertension and chronic kidney disease were other risk factors for in-hospital mortality.
Our study has several limitations. First, as mentioned above, it was impossible to stratify the study cohort into type A or B AD due to the limitations of the coding system. Therefore, the patients were classified into the TASR, TBSR, TEVAR and MM subgroups as previously described.
2 Second, our database reflects the incidence of AD in hospitalized patients, and accurately defining the incidence of AD is difficult because of its high early mortality rate and the common problem of missed diagnoses due to death outside of the hospital or before arrival at the hospital.
456 These limitations might lead to the underestimation of the incidence of AD. Autopsies of deceased patients suspected of having died from AD could help determine a more accurate incidence rate, but practical and ethical difficulties exist. Third, it is impossible to determine the exact date of surgical or endovascular intervention. If we know the date of the surgical or endovascular intervention, it may be possible to determine whether an emergency occurred; however, this analysis is impossible due to the nature of the nationwide health insurance claims from the NHIS.
In conclusion, the incidence rate of AD was 3.76 per 100,000 person-years, with an increasing tendency in Korea. The incidence rates of TASR and TEVAR significantly increased over time. The patients with thoracic AD were predominantly in their 60s and 70s. The male-to-female ratio was 54.3:45.7, which slightly differs from the sex ratios reported in previous studies. The in-hospital mortality rates of all patients and the TASR subgroup were 10.84% and 13.57%, respectively, which are noninferior to the outcomes reported in previous studies from other countries, and the in-hospital mortality rate in the TASR subgroup decreased over the course of the decade. An older age, the female sex, hypertension, and chronic kidney disease were significant predictive factors for in-hospital mortality.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download