This article has been
cited by other articles in ScienceCentral.
Abstract
Although some comorbidities, such as diabetes mellitus, lung disease, and chronic kidney disease, are known as risk factors for poor clinical outcome in patients with coronavirus disease 2019 (COVID-19), it is unknown if human immunodeficiency virus (HIV) patients with COVID-19 would have poor prognosis than others. Rare cases of HIV patients with COVID-19 have been reported. As of May 25th, 2020, over 11,000 patients have been diagnosed with COVID-19 and over 13,000 are living with HIV in Korea. Here, we present the first HIV patient with COVID-19 in Korea. The 29-year-old Korean man had been taking Genvoya® regularly for seven years and HIV was well suppressed with CD4 counts of 555/mm3. He had mild symptoms of sore throat, dry cough, loss of taste and smell. He received hydroxychloroquine while Genvoya® was continued. Pneumonia diagnosed in chest computed tomography improved without oxygen supplementation. He was discharged on hospital day 31. HIV patients are considered as immunocompromised, but this case suggests that well controlled HIV patients have satisfactory prognosis following proper medical care.
Go to :

Graphical Abstract
Go to :

Keywords: COVID-19, SARS-CoV-2, HIV
INTRODUCTION
As of May 25, 2020, the novel coronavirus disease (COVID-19) pandemic has affected 5,300,000 patients over the world. Patients with comorbidities such as diabetes mellitus, cardiovascular disease, lung disease, malignancies, and chronic kidney disease are considered to have poor outcome. Rare cases of human immunodeficiency virus (HIV) patients with COVID-19 have been reported
1234 and it is unknown if they would have poor prognosis than other patients with COVID-19. Despite the numbers of newly confirmed cases are decreasing, over 10,700 patients have been diagnosed with COVID-19 as of May 4th, 2020 in Korea. The population of Korea is 51 million and there are over 13,000 of HIV patients in Korea. Here, we present the clinical characteristics and good outcome of the first HIV patient with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in Korea.
Go to :

CASE DESCRIPTION
A 29-year-old Korean man who had lived in London, UK, arrived at the Incheon International Airport in Korea on March 29, 2020. He had mild cough, sputum, chilling, myalgia and rhinorrhea seven days before arrival. In addition, he lost his taste and smell since March 26, 2020. Although he wanted to get SARS-CoV-2 polymerase chain reaction (PCR) test, it was rejected in London. During the quarantine inspection process at the airport, he reported sore throat and mild cough. His body temperature was 37.6oC at that time. He was isolated in the airport quarantine space and the PCR using throat and nasopharyngeal (NP) swab samples showed positive for SARS-CoV-2.
On admission (March 30, 2020), the physical examination revealed a body temperature of 36.8°C, a respiratory rate of 16 per minute, a pulse of 72 per minute, and a blood pressure of 117/77 mmHg. His body mass index (BMI) was 24.21 (height 178 cm, weight 76.7 kg). There were no pharyngeal injections, skin rash, and lymphadenopathy. The laboratory test showed almost normal findings, except elevated ESR as 25 mm/hr. Platelet counts were 188,000/mm
3 and LD was 208 IU/L. His CD4 count was 555/mm
3, CD4/CD8 ratio was 0.4 and HIV RNA was lower than 20 copies/mL. The initial chest radiography showed no infiltrates (
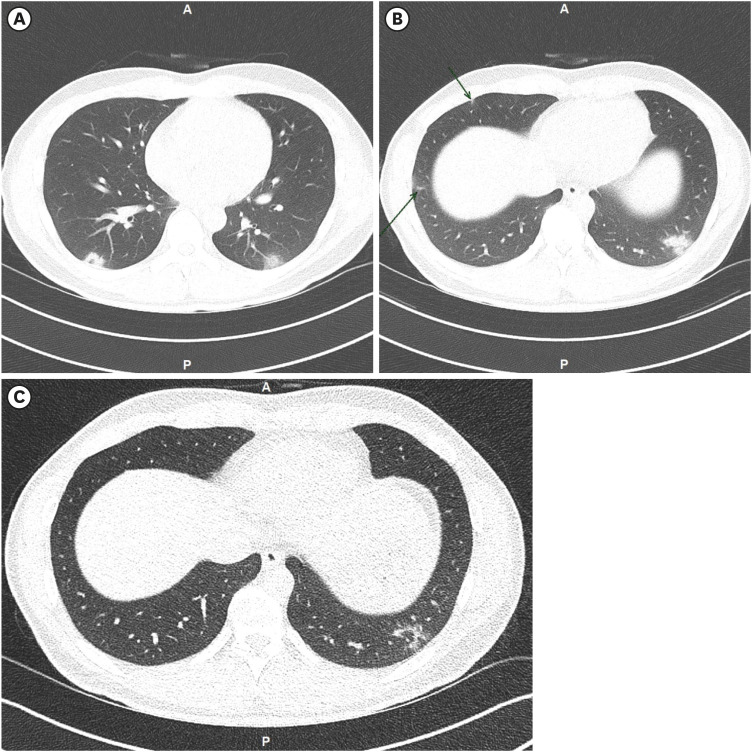
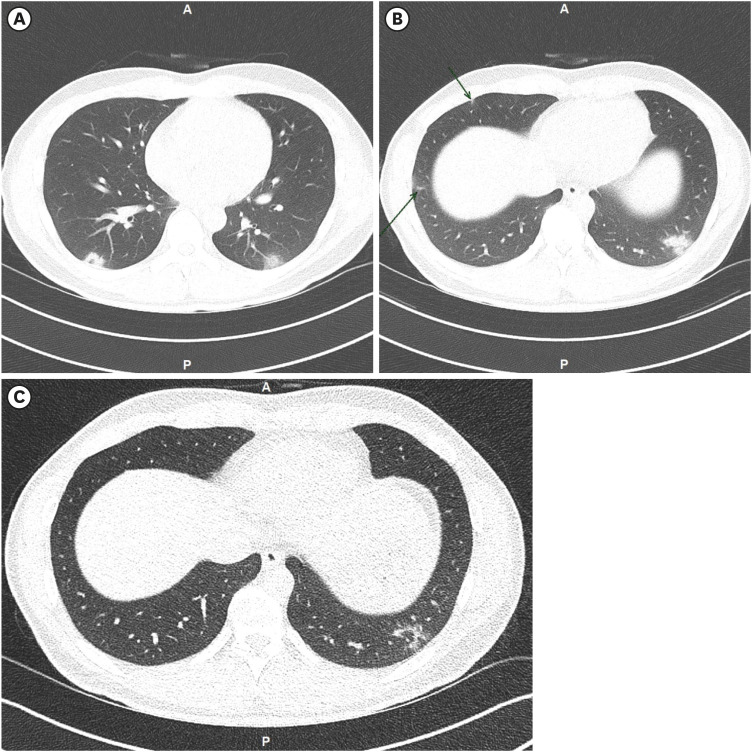
Fig. 1), but low dose chest computed tomography (LDCT) on hospital day (HD) 2 (day 9 of illness) showed multifocal consolidation with air-bronchogram surrounded by halo of ground-glass opacities (GGO) in both lower lungs (
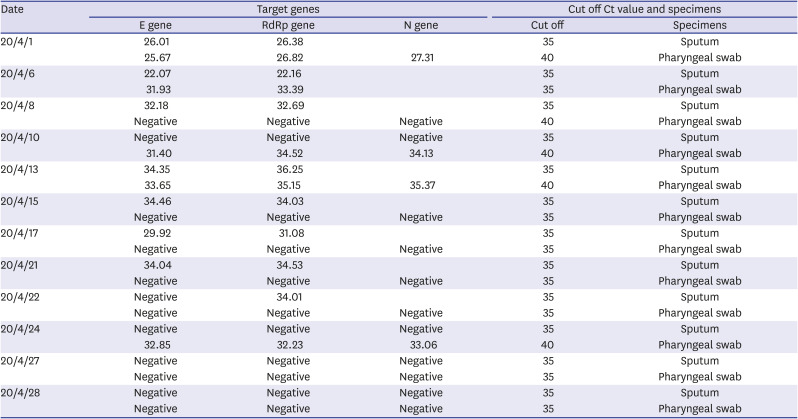
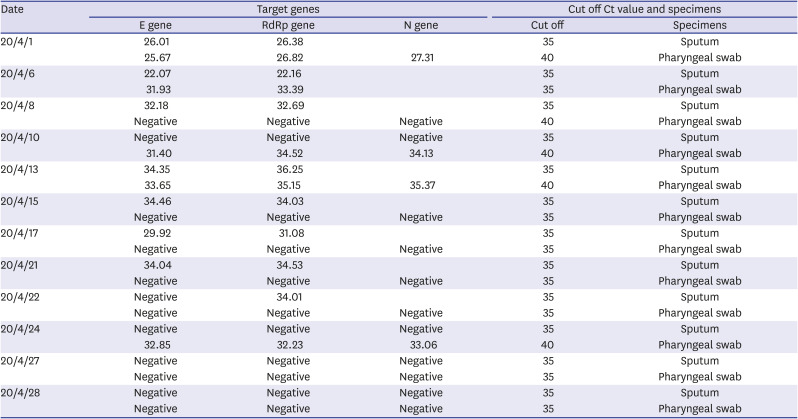
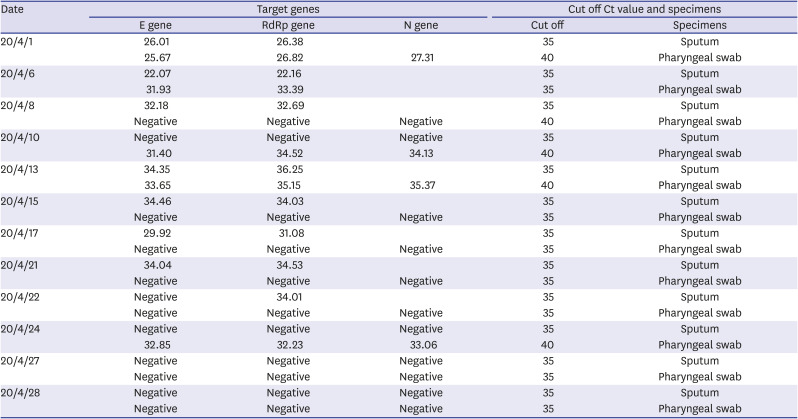
Fig. 2A and B). The Ct value was 26.82 in nasopharyngeal swab and 26.38 in sputum sample at admission (
Table 1). We used the betacoronavirus
E gene and the SARS-CoV-2 specific
RdRp gene for PCR diagnosis (Allplex™ of Seegene and PowerChek™ of Kogene).
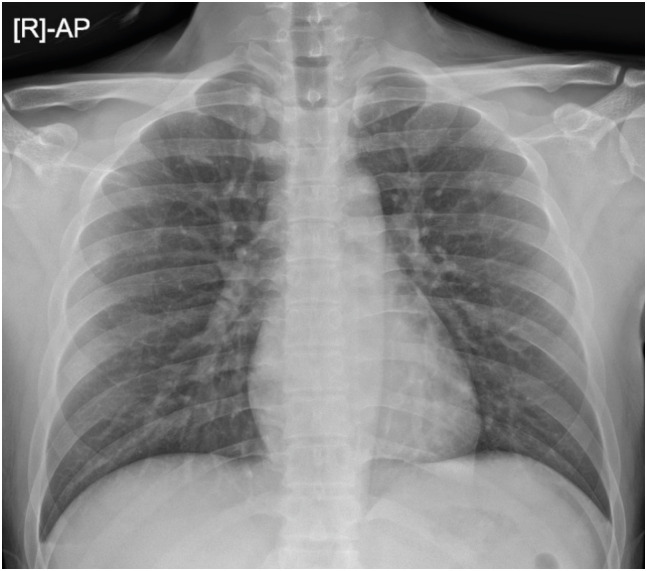 | Fig. 1 Chest X-ray on hospital day 1 (day 8 of illness).
|
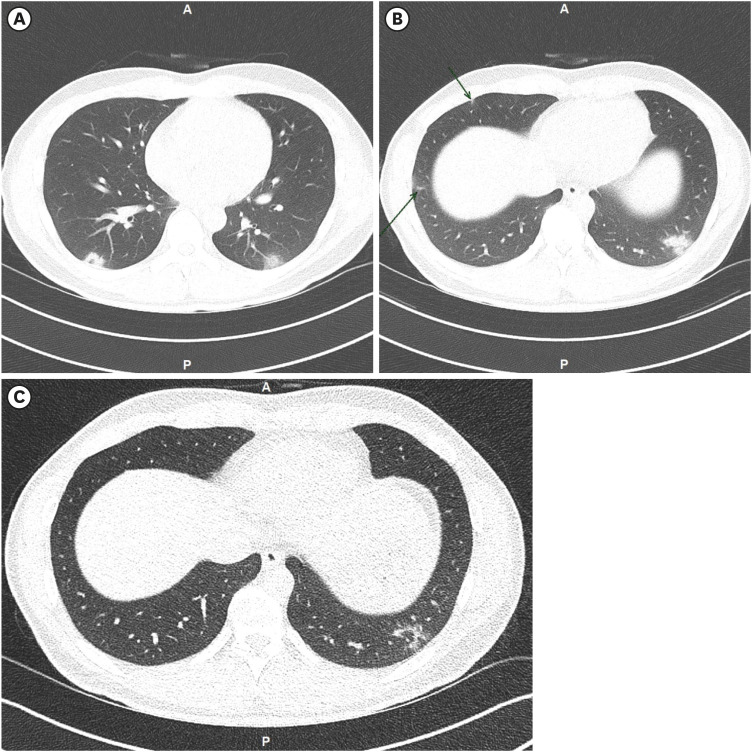 | Fig. 2
Low dose chest computed tomography of the patient.
(A, B) On HD 2 (day 9 of illness). (C) On HD 9 (day 16 of illness).
HD = hospital day.

|
Table 1
Ct values of PCR test of the patient
|
Date |
Target genes |
Cut off Ct value and specimens |
|
E gene |
RdRp gene |
N gene |
Cut off |
Specimens |
|
20/4/1 |
26.01 |
26.38 |
|
35 |
Sputum |
|
25.67 |
26.82 |
27.31 |
40 |
Pharyngeal swab |
|
20/4/6 |
22.07 |
22.16 |
|
35 |
Sputum |
|
31.93 |
33.39 |
|
35 |
Pharyngeal swab |
|
20/4/8 |
32.18 |
32.69 |
|
35 |
Sputum |
|
Negative |
Negative |
Negative |
40 |
Pharyngeal swab |
|
20/4/10 |
Negative |
Negative |
Negative |
35 |
Sputum |
|
31.40 |
34.52 |
34.13 |
40 |
Pharyngeal swab |
|
20/4/13 |
34.35 |
36.25 |
|
35 |
Sputum |
|
33.65 |
35.15 |
35.37 |
40 |
Pharyngeal swab |
|
20/4/15 |
34.46 |
34.03 |
|
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |
|
20/4/17 |
29.92 |
31.08 |
|
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |
|
20/4/21 |
34.04 |
34.53 |
|
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |
|
20/4/22 |
Negative |
34.01 |
|
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |
|
20/4/24 |
Negative |
Negative |
Negative |
35 |
Sputum |
|
32.85 |
32.23 |
33.06 |
40 |
Pharyngeal swab |
|
20/4/27 |
Negative |
Negative |
Negative |
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |
|
20/4/28 |
Negative |
Negative |
Negative |
35 |
Sputum |
|
Negative |
Negative |
Negative |
35 |
Pharyngeal swab |

During admission, he reported dry cough, loss of taste and smell. Loss of taste persisted for about two weeks. Loss of smell was improving, but persisted till discharge (HD 31). He did not complain of other symptoms such as sore throat, rhinorrhea, sputum, chilling and myalgia which he had before admission. He did not need oxygen supplementation, his oxygen saturation was 100% in room air. The regimen of anti-retroviral treatment (ART) (Genvoya
®: elvitegravir/cobicistat/emtricitabine/tenofovir), which he had been taking for 5 years, was not changed. Hydroxychloroquine 200 mg twice a day were started on the second day of admission and given for five days. No adverse events developed related to hydroxychloroquine. Pneumonia improved in follow up chest computed tomography (CT) (HD 11) (
Fig. 2B). He was discharged on HD 30 due to persistently PCR positive for SARS-CoV-2 in sputum.
Fig. 3 shows the trend of Ct values of NP swabs and sputum.
 | Fig. 3 Viral load kinetics of HIV with SARS-CoV2 patient.
|
Ethics statement
The patient submitted informed consent for this publication.
Go to :

DISCUSSION
This HIV patient who had been taking ART regularly for seven years showed mild clinical course without oxygen demand although he had bilateral pneumonia in chest CT. This course was similar with other COVID-19 patients without concomitant HIV infection. A Spanish study presented 5 HIV patients out of 543 COVID-19 patients.
1 Among them, two patients received intensive care: one with CD4 counts of 13/mL (patient A) was cured and the other with CD4 of 445/mL was still on ECMO till HD 21. Although people living with advanced HIV disease, those with low CD4 count and elevated viral load, are considered as immunocompromised patients, the first patent in the Spanish study and another late presenter in a literature survived after management in hospitals.
12 HIV patients are likely to have similar clinical features and outcomes compared to those of general population, especially when HIV RNA are suppressed under 20 copies/mL and CD4 counts are not low.
For the treatment, since boosted protease inhibitors including lopinavir/ritonavir showed antiviral activity against SARS-CoV-2 in vitro, those drugs have been commonly used for COVID-19 treatment. However, the clinical efficacy was not promising.
5 We did not change ART to boosted protease inhibitor in the patient. In contrast, all 5 patients were given boosted protease inhibitors in the Spanish study.
1 Further studies are needed to evaluate the clinical features and appropriate ART and management for HIV patients with COVID-19.
Our case highlights some issues. Although we only experienced one HIV patient with COVID-19, if HIV is well suppressed, the clinical feature is similar to that of general people with COVID-19.
The published case series
1 presented that HIV patients with COVID-19 had similar clinical features and outcomes compared to those of general population, when HIV RNA is suppressed under 20 copies/mL and CD4 counts are not low.
We maintained ART regimen and did not start any antiviral agent but hydroxychloroquine.
More observational studies are needed not changing ART regimen and giving steroids.
Go to :