INTRODUCTION
Antiretroviral therapy (ART) has reduced the rates of morbidity and mortality among patients with human immunodeficiency virus (HIV) infection.
12 In many regions, HIV infection is now widely considered as a manageable chronic disease, with the life expectancy of HIV patients receiving ART approaching that of the general population in some settings.
34 Survival after the diagnosis of HIV has also continued to improve over time since highly active antiretroviral therapy (HAART) was introduced in Korea in 1991.
5 Along with increased survival, the causes of death among HIV-infected patients have also changed gradually. As a result of the dramatic reduction in mortality resulting from acquired immunodeficiency syndrome (AIDS) defining illness, the proportion of non-AIDS-related death has increased in the HAART era.
6 A recently published Canadian population-based cohort study showed that non-AIDS-defining cancers are currently the leading non-AIDS-related cause of death among HIV-infected patients. A previous study conducted in Korea showed that the proportion of AIDS-related death remained higher than non-AIDS-related death between 1990 and 2011. Since then, although an increase in survival has been documented, there have not been any recently published data regarding the specific causes of death among people diagnosed with HIV in Korea. According to a study forecasting cause-specific mortality in Korea, causes of death regarding HIV and AIDS are estimated to increase from 2002 to 2030.
7 However, until now, little data has been available on the causes of death in HIV patients in Korea, which could be useful information to help focus on appropriate interventions to improve the rates of morbidity and mortality of HIV patients. In addition, with the ongoing national Korean multicenter cohort research data, there is a limitation to investigate the changes in the cause of death because 73.8% of the data on causes of death are missing.
8
This study aimed to evaluate the changes in the causes of death among HIV-infected patients in Korea in the era of ART according to the HIV diagnosis and death period. In addition, we aimed to elucidate the prognosis of low CD4 counts at the time of HIV diagnosis.
DISCUSSION
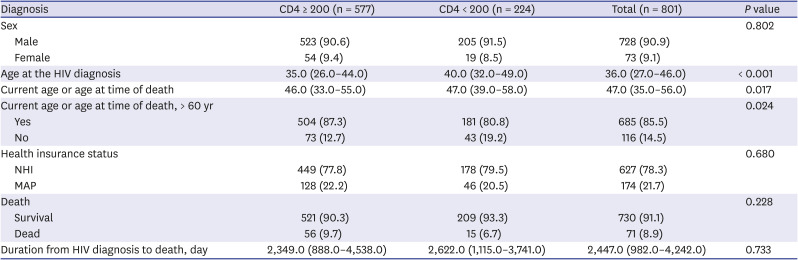
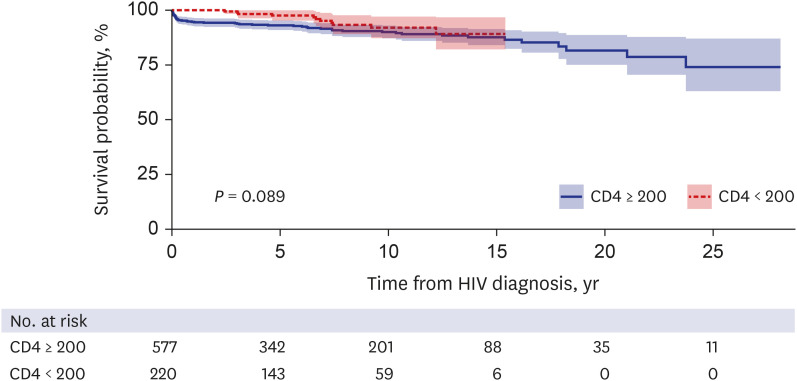
In this study, we had a follow-up period of more than 20 years to monitor the changes in causes of death and the impact of low CD4 counts at the time of HIV diagnosis on death among HIV-infected patients in Korea. We elucidated that HIV patients diagnosed with CD4 < 200 cells/mm
3 were not at greater risk of death compared with the CD4 ≥ 200 cells/mm
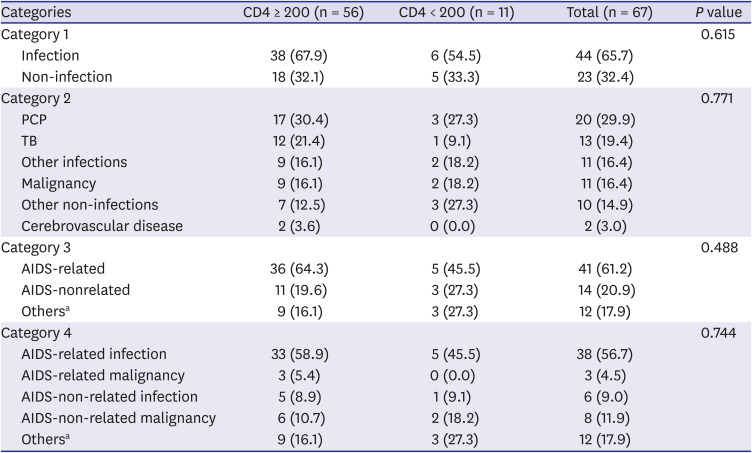
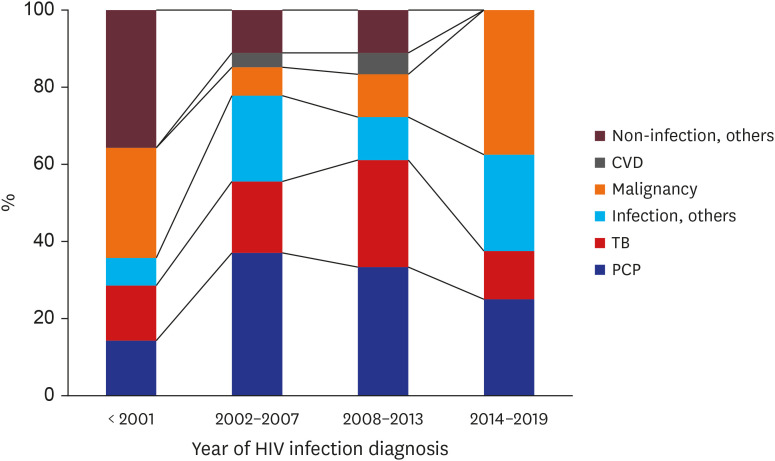
3 group. Our study showed that PCP was the single most common cause of death among HIV patients in both the past and present, and that TB was the second leading cause of death from infections. These are similar to results of a previous study conducted in Korea between 1990 and 2011,
6 but the frequency of these diseases has decreased in recent years. Malignant tumors have become an important cause of death in recent years, and an increasing tendency of AIDS-non-related malignancies was observed.
It is important to identify prognostic factors for survival among HIV-infected patients. Based on previous studies, CD4 cell count was suggested as the most important prognostic factor among the main risk factors for death.
1213 It has been reported that CD4 cell count at the time of HIV diagnosis is the predominant prognostic factor for survival,
14 and baseline CD4 counts are more relevant for AIDS-related causes of death. This observation has shown important implications for the clinical management of HIV patients.
15 CD4 count at the start of ART is strongly associated with short-term survival, but its association with longer-term survival is less well characterized. A recent study conducted in North America and Europe suggested that patients with low baseline CD4 cell count only carry the burden of increased risk of death up to 5 years after ART.
16 Another study conducted in China also showed that baseline CD4 count becomes a weak prognostic factor after 6 months of starting ART.
17
In our study, there was no significant difference observed regarding long-term survival coming from baseline low CD4 count in this study. Though, the short-term survival rate (HIV diagnosis to death within 3 months) showed a higher survival rate in groups with CD4 counts less than 200 at the time of diagnosis. Among CD4 count < 200 cells/mm3 group patients, those who died within three months were not identified, which could be interpreted as a study limitation of the distribution of patients. This result showed that it is difficult to identify the association between the CD4 counts at the time of HIV diagnosis and short-term mortality rate, and further studies are needed to evaluate the associations.
Although our study did not include the ART status near the time of HIV diagnosis, we showed that WHO HIV stages at the time of HIV diagnosis and death were not statistically different between the CD4 < 200 cells/mm3 and CD4 ≥ 200 cells/mm3 groups.
A recently published prospective cohort study in Japan reported that late diagnosis (CD4 < 200 cells/mm
3 at the first visit) was an independent risk factor for mortality among HIV patients.
18 According to a previous large HIV population-based cohort study, the mortality rate was higher in patients with CD4 counts of 200 cells/mm
3 or less, and a CD4 count of less than 200 is one of the factors associated with AIDS-related causes of death.
19 However, in our study, the mortality rate and AIDS-related causes of death between CD4 < 200 cells/mm
3 and CD4 ≥ 200 cells/mm
3 groups showed no significant differences. This difference might be attributed to the fact that the previous study did not find a specific cause of death in 18.7% of patients.
19
In addition, a previous study showed that socioeconomic disadvantage was strongly associated with poorer HIV treatment outcomes in settings with universal access to health care suggesting the importance of adherence to interventions and social support.
20 Therefore, considering the association between socioeconomic status and drug adherence followed by compliance, we investigated the association of socioeconomic status with long term survival. We have found that a patient’s socioeconomic status did not show a statistical difference on the survival between the national health care group and MAP group, implying that other factors including the national HIV and AIDS strategy, which aimed to increase access to care, improve health outcomes and address health inequities might be playing an important role on an HIV patient's survival, as reported in a previous study.
22122 Especially in Korea, there is no difference in access to hospitals based on income, as the government fully supports the cost of treating HIV patients. Even with late diagnosis, if the patients were on ART treatment, the clinical prognosis on survival could be similar, regardless of CD4 count at the time of HIV diagnosis and socioeconomic status.
HIV infection has become a chronic disease with the improvement of HIV treatment. Advances in ART, effectiveness in HIV suppression, decreased side effects, and increased ease of taking medications have contributed to these improvements.
23 The introduction of combination ART also marked an important achievement toward prolonging the lifespan of HIV patients, resulting in shifting patterns in both mortality rates and leading causes of death in high-income countries.
24
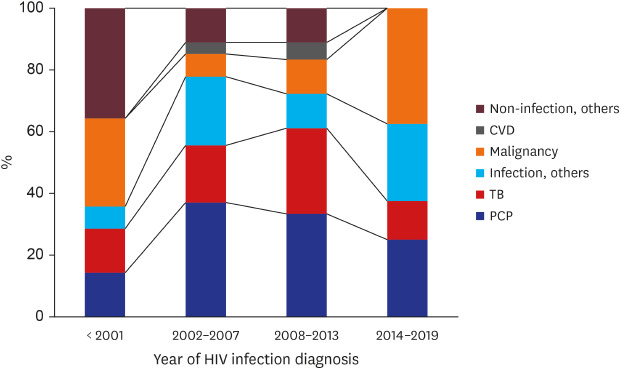
With more recent HIV diagnoses, HIV patients showed a tendency to die of non-infection-related causes. Among the non-infection death causes, malignancy accounted for approximately 40% of the deaths of patients diagnosed between 2014 and 2019, which is 2 times more than among cases diagnosed between 2008 and 2013.
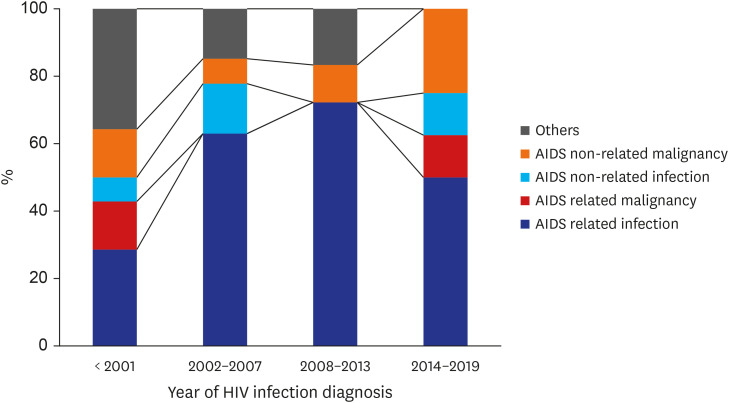
Among HIV-infected patients, as rates of death owing to AIDS-attributable causes decreased, rates owing to non-AIDS-attributable causes also decreased, but the percentages of deaths resulting from non-HIV-attributable causes, such as heart disease and non-AIDS cancers, increased.
25 It has been reported that AIDS-related deaths have decreased, whereas non-AIDS-related deaths, such as those because of non-AIDS malignancy or cardiovascular diseases, have increased among an aging cohort of HIV patients.
2627
Korea is among the high-income countries, and our study also showed that AIDS-related deaths decreased, whereas non-AIDS-related deaths increased between 2015 and 2019. In New York, the percentage of deaths owing to non-AIDS-related causes increased by 32.8% (from 19.8% to 26.3%;
P = 0.015) between 1999 and 2004. Among deaths owing to non-AIDS-related causes, 76% could be attributed to non-AIDS-defining types of cancer, cardiovascular disease, or substance abuse.
28 A recently published Canadian population-based cohort study showed that non-AIDS-defining cancers are currently the leading non-AIDS-related cause of death in HIV-infected patients.
29 Our study also showed that between the years of 2015 and 2019, AIDS-non-related disease has become an important cause of death and AIDS-non-related malignancy is currently the leading non-AIDS-related cause of death. It has been also confirmed that the incidence of malignant tumors increases with age, accounting for about 1% of those under 60 and about 4% of those over 60. The increasing number of HIV patients dying of diseases non-related to AIDS can be explained by the improvement of drugs and the improvement of patients' compliance through HIV counseling projects. Among non-AIDS-related deaths, the incidence of cerebrovascular disease was lower than expected and there was no death owing to cardiovascular disease or drug dependency in this study.
According to a study of specific causes of death in Japan between 2005 and 2016, AIDS-related malignancies accounted for 24%, non-AIDS-defining malignancies for 23%, and AIDS-defining infections accounted for 15%.
18 Although the study period was somewhat different from our study period, the most common cause of AIDS-defining infection was PCP, which was similar to our study. However, the second most common cause of infection was found to be progressive multifocal leukoencephalopathy in Japan compared with our finding of TB in Korea. Infection cause of death priorities appear to be different depending on high prevalence infectious diseases, such as TB. Toxoplasmosis was found in 2 patients (0.01%) in the Japanese study. However, there was no death from toxoplasma infection in this study. Among the AIDS-defining malignancies, lymphoma was the most common cause in the Japanese study. Death from AIDS-associated malignancies was also caused mainly by lymphomas in this study. Death from the Kaposi’s sarcoma was found in 2 patients (0.015%) in the Japanese study, but there was no death from Kaposi's sarcoma in our study. Suicide as the cause of death accounted for 8.5% of deaths in Japan, whereas this accounted for 4.5% in our study.
This study has several limitations. First, our study was conducted at a single center in Korea. Therefore, our findings may not be generalized to other regions of the country. Nevertheless, this was the first study in Korea to elucidate the trends of causes of death in HIV patients in the past 20 years. Second, it was not possible to identify the survival of follow-up loss patients and, in cases of death outside of the hospital there was a restriction on the cause of death analysis. Therefore, we had to exclude 4 patients who died outside of the hospital with unidentified causes of death. However, these numbers did not seem significant compared with the total number of deaths among HIV patients included in the death cause analysis, accounting for approximately 5%. Third, our database did not include data regarding ART adherence. We could not identify whether the patients continued to receive ART near their deaths or not; nor could we identify ART start time after HIV diagnosis. This may result in bias in the interpretation of the survival results according to the baseline CD4 count difference. Nevertheless, we believe that this study is worthy of sustained attention because our study demonstrated that there was no statistical difference regarding ever ART history and long-term survival analysis of overall causes of death, including AIDS-related death between the CD4 < 200 cells/mm3 group and the CD4 ≥ 200 cells/mm3 group.
In conclusion, our results showed that patients diagnosed with CD4 < 200 cells/mm3 are not at greater risk of death than those with CD4 ≥ 200 cells/mm3, and those diagnosed with HIV in more recent years show a tendency to die from non-AIDS-related diseases, suggesting that the effectiveness of ART and improved and solid medical care cascade systems greatly contribute to this. Ongoing monitoring of mortality trends by causes of death will continue to be important and will provide the necessary data to enable appropriate targeting of interventions to improve the quality of patient care and reduce avoidable mortality.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download