This article has been
cited by other articles in ScienceCentral.
Abstract
Community-based health management policies are needed considering societal aging. We aimed to develop a transitional care model (TCM) program for patients with pneumonia, asthma, and chronic obstructive pulmonary disease. First, we conducted in-depth interviews with patients who were hospitalized, released, and readmitted for those three conditions to identify issues with the current hospitalization/discharge system and post-discharge processes. Next, we developed a new TCM program suited to the realities of the current medical environment. Interviews revealed problems including inadequate awareness of disease and health management; insufficient information exchange between patients, caregivers, and primary medical institutions; and absence/low usage of community-based care services. The investigation applying the new TCM program to patients and following up on readmission rates and life satisfaction after discharge is ongoing. Reviewing these results and conducting further studies in the future will allow improvements to the model.
Go to :

Graphical Abstract
Go to :

Keywords: Pneumonia, Asthma, Chronic Obstructive Pulmonary Disease, Hospital Readmission, Transitional Care
Recently, numerous countries, including Korea, are experiencing rapid population aging, which leads to increased numbers of chronic patients, repeated hospital readmissions associated with reduced quality of life, and elevated medical costs.
12 Accordingly, there has been an explosive growth in the demand for out-of-hospital health management and community-based care, which has become a universal issue.
13
The Korean government announced the “Comprehensive Plan for Community Care,” developing new care models to prepare for societal aging, preparing legal and institutional resources, and expanding infrastructure; it established the principle of autonomous implementation at the community level. Additionally, the “Comprehensive Plan for the Advancement of Public Healthcare” was published in October 2018, emphasizing reinforcing public healthcare; a core objective was “to strengthen local community-based health management systems.” In this context, in 2019, ten national university hospitals across the country were selected as regional public healthcare centers, and pilot projects were pursued to establish care programs for discharged patients. These projects aimed to improve support for patients' rapid return to society and enhance treatment quality for patients after discharge. For this, the hospitals established a care plan before discharge to link the patients with community-based services, thereby enabling continuous medical and care services in the local community after discharge.
Kangwon National University Hospital was a designated hospital for pilot projects in 2019, and the present project is targeted for patients with respiratory diseases. We used a transitional care model (TCM) as the main project model. It is an intervention method for elderly patients with multiple risk factors when facing a changing environment of medical institutions, medical personnel, or healthcare services.
456 According to previous studies, application of a TCM to patients with chronic obstructive pulmonary disease (COPD) or asthma after discharge reduced their rehospitalization rate, emergency room (ER) visits, and length of stay compared to a control group.
7891011 However, TCMs vary greatly depending on what elements are included in each model or how the elements are combined. As this variation can lead to differing results, it is important to construct a TCM to suit the medical environment and patients' specific circumstances.
812 Hence, we first conducted in-depth interviews with inpatients who were readmitted within the past six months to identify problems with their hospitalization/discharge and post-discharge processes; we then developed a new TCM program to address these problems.
In-depth Interviews
We conducted in-depth interviews with patients and their caregivers. The interviewees comprised patients hospitalized in the Kangwon National University Hospital's Department of Respiratory Medicine for pneumonia, asthma, or COPD and readmitted within six months of discharge. Two nurses conducted individual interviews with patients and caregivers who consented to participate. The interviews were semi-structured, using standard questions on the details of 1) previous hospitalization, 2) time between the previous hospitalization and the current readmission, 3) (current) readmission, and 4) everyday management of respiratory disease. The interviews proceeded until both the interviewer and the interviewee felt there was nothing further to be obtained; each interview lasted for 30 minutes–1 hour. Additional interviews were conducted in case of inadequate interview content or insufficient time with an interviewee. After completing the interviews, the preventive medicine physicians and the nurses who conducted the interviews identified the root causes of readmission using the 5-Whys technique.
13 Additionally, the actual readmission processes of patients were compared with a hypothetical ideal process.
13 The aims were to generate an improved plan for use with patients in the hospital.
The six interview participants, five males and one female, included three COPD patients, two pneumonia patients, and one asthma patient. Three of the interviews were conducted with patients, and the other three with caregivers (the patient's daughter, in all cases). All six patients were aged ≥ 65 years.
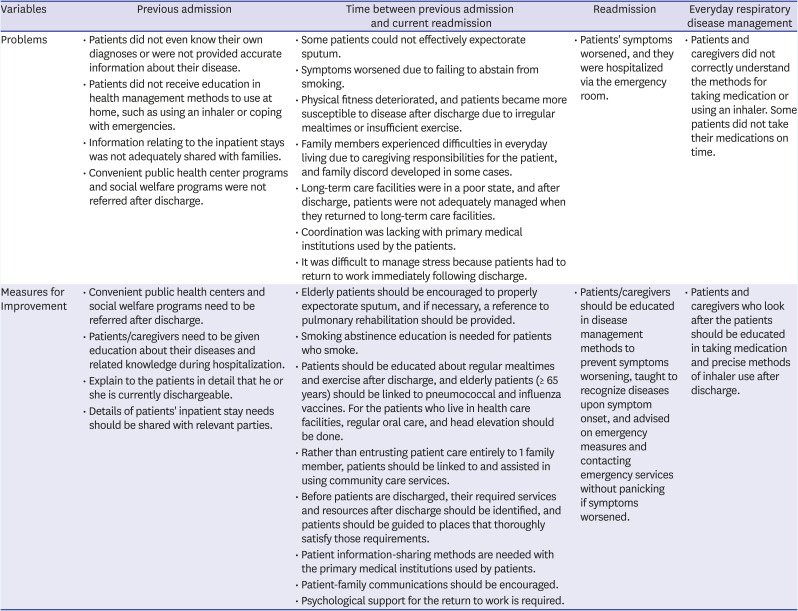
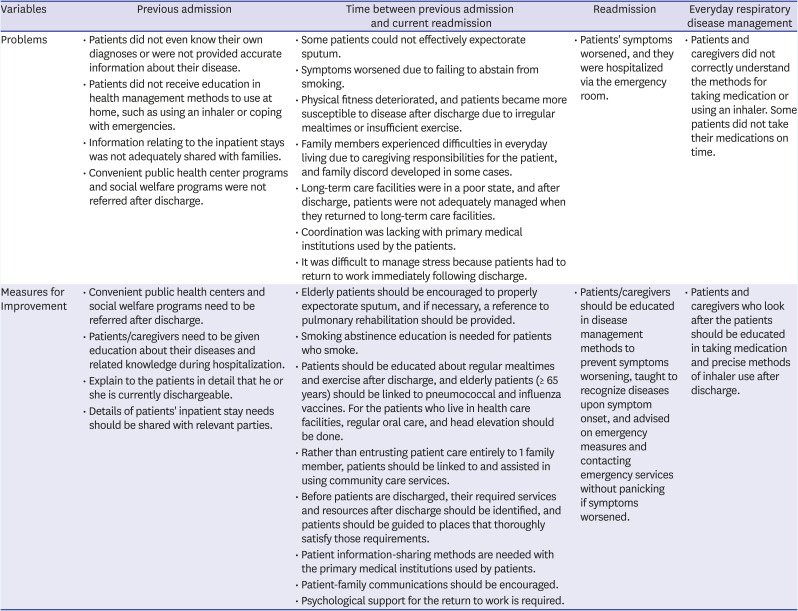
Table 1 shows the problems with the current admission/discharge system identified in the interviews and the elements of the improved plan.
Table 1
Problems with the readmission process for patients and ideas for improvement
|
Variables |
Previous admission |
Time between previous admission and current readmission |
Readmission |
Everyday respiratory disease management |
|
Problems |
• Patients did not even know their own diagnoses or were not provided accurate information about their disease. |
• Some patients could not effectively expectorate sputum. |
• Patients' symptoms worsened, and they were hospitalized via the emergency room. |
• Patients and caregivers did not correctly understand the methods for taking medication or using an inhaler. Some patients did not take their medications on time. |
|
• Patients did not receive education in health management methods to use at home, such as using an inhaler or coping with emergencies. |
• Symptoms worsened due to failing to abstain from smoking. |
|
• Information relating to the inpatient stays was not adequately shared with families. |
• Physical fitness deteriorated, and patients became more susceptible to disease after discharge due to irregular mealtimes or insufficient exercise. |
|
• Convenient public health center programs and social welfare programs were not referred after discharge. |
• Family members experienced difficulties in everyday living due to caregiving responsibilities for the patient, and family discord developed in some cases. |
|
• Long-term care facilities were in a poor state, and after discharge, patients were not adequately managed when they returned to long-term care facilities. |
|
• Coordination was lacking with primary medical institutions used by the patients. |
|
• It was difficult to manage stress because patients had to return to work immediately following discharge. |
|
Measures for Improvement |
• Convenient public health centers and social welfare programs need to be referred after discharge. |
• Elderly patients should be encouraged to properly expectorate sputum, and if necessary, a reference to pulmonary rehabilitation should be provided. |
• Patients/caregivers should be educated in disease management methods to prevent symptoms worsening, taught to recognize diseases upon symptom onset, and advised on emergency measures and contacting emergency services without panicking if symptoms worsened. |
• Patients and caregivers who look after the patients should be educated in taking medication and precise methods of inhaler use after discharge. |
|
• Patients/caregivers need to be given education about their diseases and related knowledge during hospitalization. |
• Smoking abstinence education is needed for patients who smoke. |
|
• Explain to the patients in detail that he or she is currently dischargeable. |
• Patients should be educated about regular mealtimes and exercise after discharge, and elderly patients (≥ 65 years) should be linked to pneumococcal and influenza vaccines. For the patients who live in health care facilities, regular oral care, and head elevation should be done. |
|
• Details of patients' inpatient stay needs should be shared with relevant parties. |
• Rather than entrusting patient care entirely to 1 family member, patients should be linked to and assisted in using community care services. |
|
• Before patients are discharged, their required services and resources after discharge should be identified, and patients should be guided to places that thoroughly satisfy those requirements. |
|
• Patient information-sharing methods are needed with the primary medical institutions used by patients. |
|
• Patient-family communications should be encouraged. |
|
• Psychological support for the return to work is required. |

Previous admission
All patients who were interviewed directly reported that they did not know their diagnosis at the time of their previous admission. They also mentioned that at discharge, they had not received an explanation about methods of managing health at home, using an inhaler, or coping with emergencies. Moreover, treatment details and precautions were not properly shared with patients' families nor with the nursing aides caring for the patients after discharge. The comparisons with the hypothetical ideal process identified three to nine linkable social welfare services available to each patient at discharge, but these were not properly utilized.
Time between previous and current admission
There were cases in which symptoms worsened because the patient could not properly expectorate sputum or abstain from smoking. Some patients reported fitness declines due to irregular mealtimes or inadequate exercise post-discharge. Some also reported family discord, as caring for the patient caused hardships in family members' daily lives. Finally, information was not properly shared with the patients' local primary medical care institutions.
Current hospitalization (readmission)
Of the six patients who participated in interviews, four were admitted via the ER, 1 of whom experienced severe symptoms requiring ventilator care in the intensive care unit. Patients who had been prescribed an inhaler were not familiar with its use in emergencies.
Everyday management of respiratory disease
Patients did not have a good understanding of how to take their medicine or use their inhaler; some reported not taking their medicine according to the prescribed schedule.
The 5-Whys technique identified the following fundamental factors in the patient readmissions
• Patients lacked awareness of their disease and were incapable of proper disease management.
• There was insufficient information exchange between the caregiver during inpatient treatment and the nursing aide (carer) after discharge, resulting in poor adherence to the precautions advised by the hospital.
• It was difficult to manage stress because patients had to return to work immediately following discharge.
• The patients' overall physical fitness worsened due to insufficient nutritional intake or exercise.
• Proper care was not provided at long-term care facilities, and elderly patients living alone had difficulty in self-care.
Go to :

Development and Application of a TCM Program Based on the Observed Circumstances
We developed and applied a new TCM based on analyses of the in-depth interviews. Preventive medicine physicians, a respiratory medicine physician, and nurses participated in developing the new TCM with assistance from a social worker. In addition to in-depth interviews, we referred to previous case reports of international TCM projects.
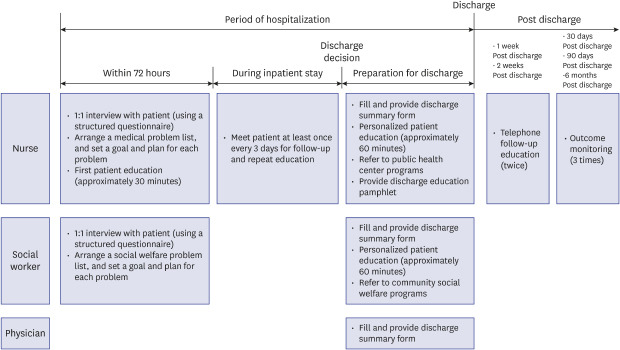
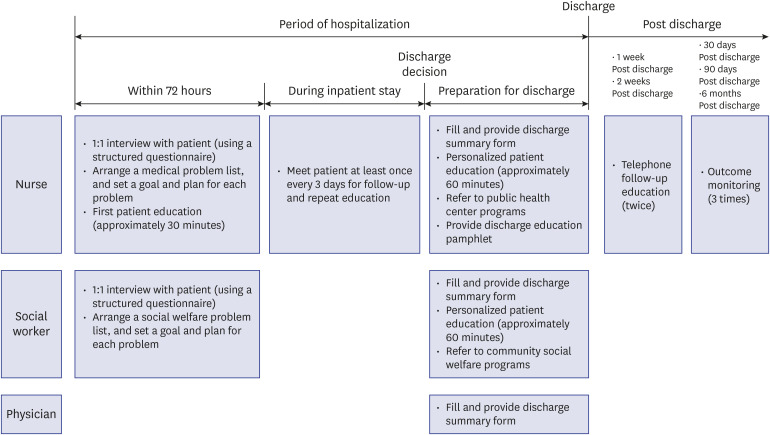
1415 The TCM was revised while administering the service to 19 patients during a pilot period from August 1 to 31, 2019, and a diagram of the final TCM is shown in
Fig. 1.
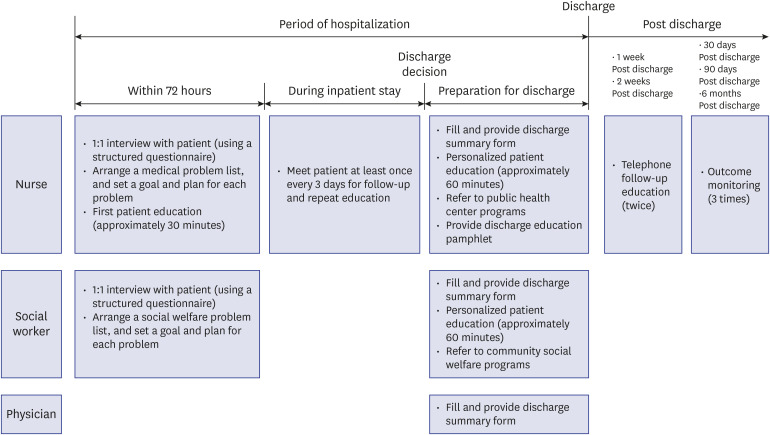 | Fig. 1 The new transitional care model developed for pneumonia, asthma, or chronic obstructive pulmonary disease patients.
|
The recipients of the new TCM were adults, ≥ 18 years, admitted to Kangwon National University Hospital with a diagnosis of pneumonia, COPD, or asthma; a nurse and social worker were assigned to each patient upon admission. Within 72 hours of patient admission, a nurse and social worker conducted a 1:1 interview to identify problems and establish a goal and plan for each problem. The nurse provided at least 30 minutes of basic education relating to the patient's disease and continually observed the patient during their hospital stay, meeting the patients at least once every three days, and reminding them of the contents of prior education sessions. Once the patient was scheduled for discharge, the nurse referred them to a convenient local public health center program, and the social worker referred them to a convenient local welfare program. The nurse, social worker, and a board-certified internist compiled a discharge summary form. The discharge summary form includes inpatient treatment details at the current hospital, test results, drug prescriptions, details of self-management education, and details of the referred public health center and local welfare programs. The nurse provided customized patient education before discharge, including a pamphlet with the contents of this education. The nurse contacted the patient at 1- and 2-weeks after discharge to discuss the patient's use of the linked programs and adherence to advice and medication regimen. To assess program effectiveness, patients were called 30 days, 90 days, and six months after discharge to check survival, current life satisfaction, and any readmission to hospitals or the ER.
TCM implementation and outcome monitoring began earnestly on September 1, 2019. However, in actual practice, a social worker could not be hired during the trial period, so the role of the social worker in the final selected model was not fulfilled. As of February 6, 2020, the service was provided to 69 patients: 50 pneumonia, nine asthma, and 10 COPD patients. The program is ongoing and will be further developed for use with more patients by examining and monitoring outcomes, conducting further studies, and applying improvements.
Go to :

Ethics Statement
The present study protocol was reviewed and approved by the Institutional Review Board of Kangwon National University Hospital (approval No. 2019-07-009). Informed consent was submitted by all subjects when they were enrolled.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download