INTRODUCTION
Congenital bleeding disorders are rare diseases caused by deficiencies of protein cofactors and enzymes involved in blood coagulation.
12 The most common coagulopathies are von Willebrand disease (vWD), an autosomal inherited bleeding disorder caused by a deficiency or abnormality of von Willebrand factor; hemophilia A (HA); and hemophilia B (HB). HA and HB are X-linked inherited disorders caused by deficiencies of factors VIII and IX, respectively.
1
The Korea Hemophilia Foundation (KHF) publishes an annual report on its patient registry, including patient demographics and data on the utilization of health services.
3 However, patients who are not enrolled in the KHF are not properly identified. Some patients are reluctant to register in the KHF for various reasons. Others may not be diagnosed properly. Therefore, it is difficult to accurately ascertain the number of people with congenital bleeding disorders in Korea. According to the 2018 KHF Annual Report, there were 2,458 registered patients, including 1,889 (77%) with HA, 450 (18%) with HB, and only 136 (5%) with vWD.
3 According to the 2018 annual global survey of the World Federation of Hemophilia (WFH), there are 2,423 hemophilia patients in Korea.
4 Australia (n = 2,653) and South Africa (n = 2,332), which have similar numbers of hemophilia cases, have 2,146 and 647 vWD patients, respectively. Therefore, some congenital bleeding disorders in Korea might be underestimated.
The epidemiology of congenital bleeding disorders in Korea has not been examined using nationwide population-based data. Therefore, we examined the nationwide incidence of congenital bleeding disorders using the Korean Health Insurance Review and Assessment Service (HIRA) databases.
RESULTS
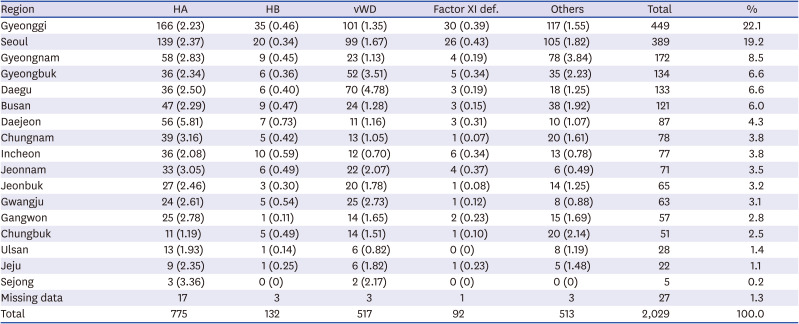
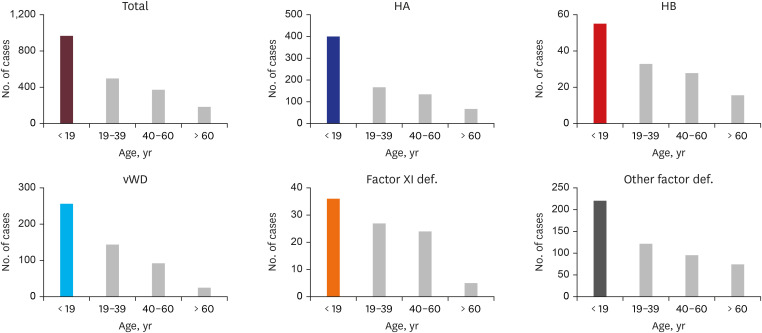
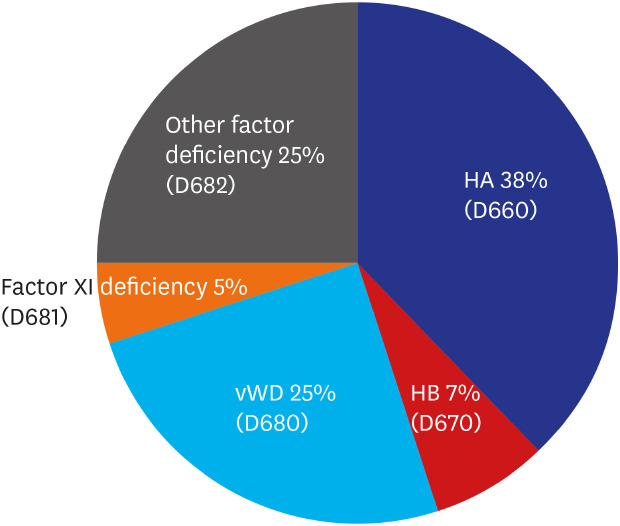
We identified 2,029 patients with congenital bleeding disorders during the 6-year period. The overall incidence of congenital bleeding disorders was 0.78/100,000 person-years. HA was the most frequent disorder with 775 patients identified, accounting for 38% of all patients included between January 2010 and December 2015 (
Fig. 1). Although vWD has been widely known as the most common congenital bleeding disorder, only 517 patients with vWD were identified, accounting for 25% of the total number of patients in the 6 years. Patients with HB made up 7% (n = 132) of the total. Patients with factor XI deficiency accounted for 5% (n = 92) of the total. Other rare congenital bleeding disorders were deficiencies of factors I, II, V, VII, X, XII, and XIII, which affected 25% (n = 513).
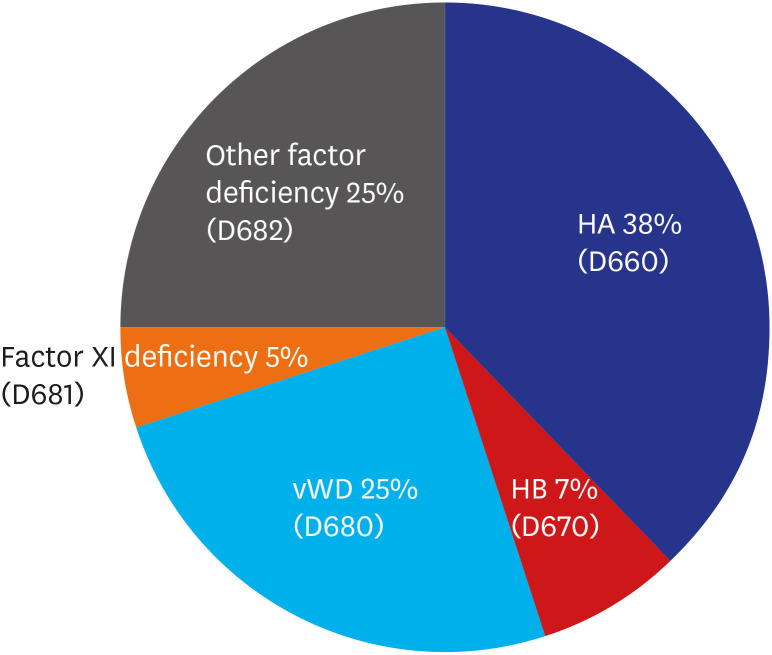
Fig. 2 shows the trend in the numbers of patients registered with congenital bleeding disorders in the last 6 years. These data do not represent a gradual increase or decrease on simple number each year. However, HA had a gradual increase of the estimated ASR in HA from 2010 (1.78/100,000) to 2014 (3.15/100,000) (
Table 1).
Fig. 1
Patients with congenital bleeding disorders reported in the Korean HIRA database from 2010 to 2015.
HIRA = Health Insurance Review and Assessment Service, HA = hemophilia A, HB = hemophilia B, vWD = von Willebrand disease.
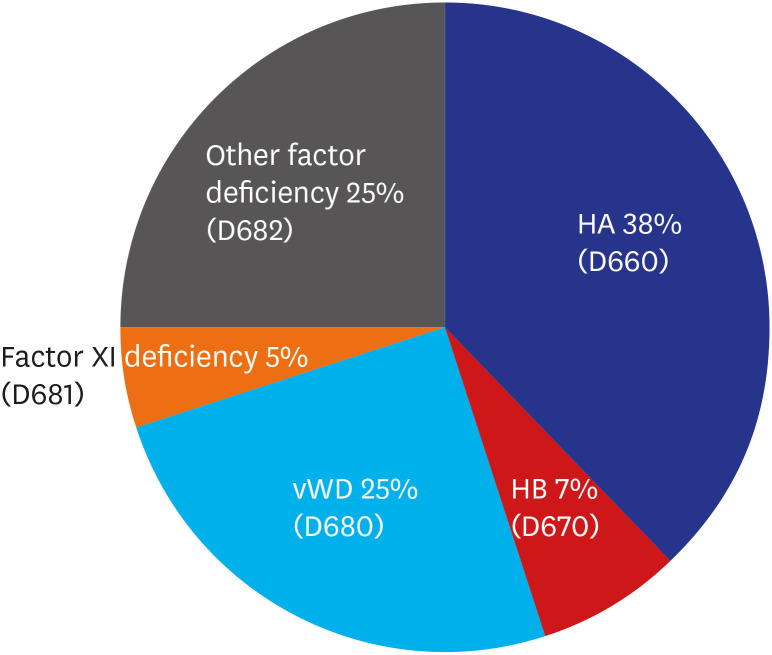
Fig. 2
Trends in the total numbers of patients with bleeding disorders registered in the Korean HIRA database from 2010 to 2015.
HIRA = Health Insurance Review and Assessment Service, HA = hemophilia A, HB = hemophilia B, vWD = von Willebrand disease.
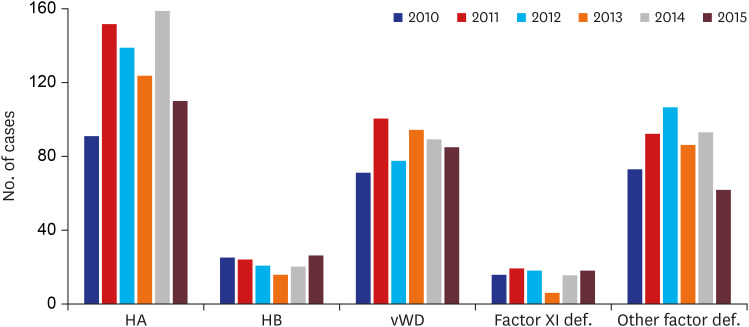
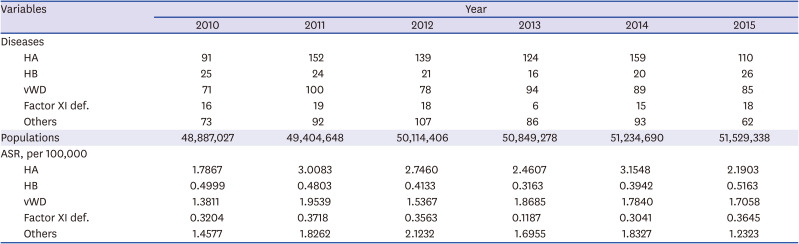
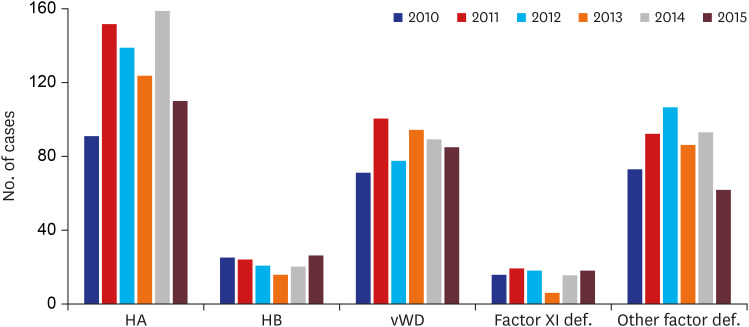
Table 1
Age standardized incidence rate of each congenital bleeding disorder by year
|
Variables |
Year |
|
2010 |
2011 |
2012 |
2013 |
2014 |
2015 |
|
Diseases |
|
|
|
|
|
|
|
HA |
91 |
152 |
139 |
124 |
159 |
110 |
|
HB |
25 |
24 |
21 |
16 |
20 |
26 |
|
vWD |
71 |
100 |
78 |
94 |
89 |
85 |
|
Factor XI def. |
16 |
19 |
18 |
6 |
15 |
18 |
|
Others |
73 |
92 |
107 |
86 |
93 |
62 |
|
Populations |
48,887,027 |
49,404,648 |
50,114,406 |
50,849,278 |
51,234,690 |
51,529,338 |
|
ASR, per 100,000 |
|
|
|
|
|
|
|
HA |
1.7867 |
3.0083 |
2.7460 |
2.4607 |
3.1548 |
2.1903 |
|
HB |
0.4999 |
0.4803 |
0.4133 |
0.3163 |
0.3942 |
0.5163 |
|
vWD |
1.3811 |
1.9539 |
1.5367 |
1.8685 |
1.7840 |
1.7058 |
|
Factor XI def. |
0.3204 |
0.3718 |
0.3563 |
0.1187 |
0.3041 |
0.3645 |
|
Others |
1.4577 |
1.8262 |
2.1232 |
1.6955 |
1.8327 |
1.2323 |
The estimated ASR of HA is 1.78–3.15/100,000 people per year. That for vWD was 1.38–1.95/100,000 people per year between 2010 and 2015 (
Table 1). Highest proportion (47.8%) of patients with congenital bleeding disorders was diagnosed at age under 19 years old. For all disorders except factor XI deficiency, more than half of patients were diagnosed at < 19 years of age (
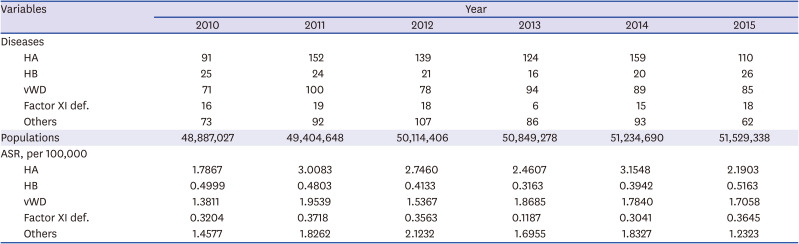
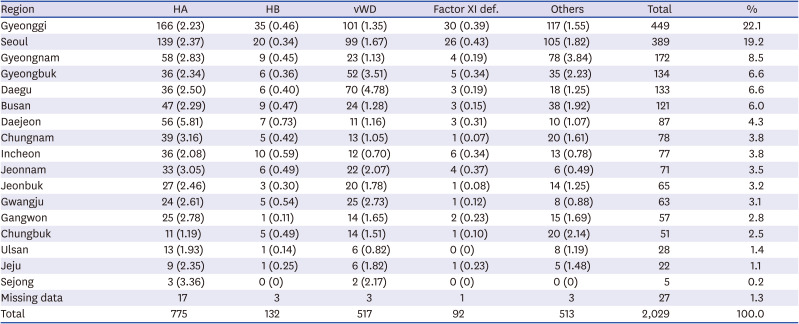
Fig. 3). The geographic distribution of the patients with congenital bleeding disorders in Korea most in Gyeonggi (22.1%) and Seoul (19.2%) (
Table 2). However, the estimated ASR of HA was the highest in Daejeon (5.81/100,000) and that for vWD was the highest in Daegu and Gyeongbuk, respectively (4.78/100,000 and 3.51/100,000).
Fig. 3
Distributions of patients with congenital coagulation disorders according to age during 6 years.
HA = hemophilia A, HB = hemophilia B, vWD = von Willebrand disease.
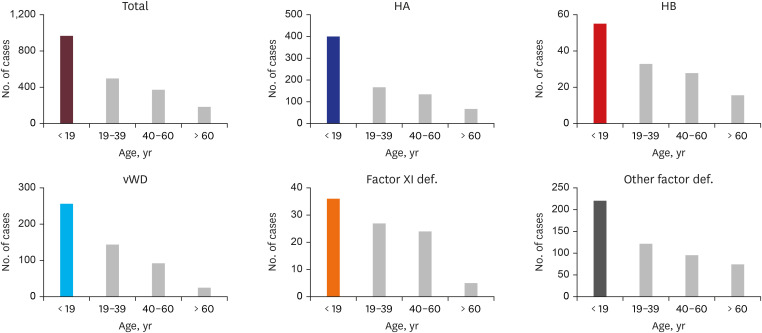
Table 2
Distributions of patients with congenital coagulation disorders according to region for 6 years
|
Region |
HA |
HB |
vWD |
Factor XI def. |
Others |
Total |
% |
|
Gyeonggi |
166 (2.23) |
35 (0.46) |
101 (1.35) |
30 (0.39) |
117 (1.55) |
449 |
22.1 |
|
Seoul |
139 (2.37) |
20 (0.34) |
99 (1.67) |
26 (0.43) |
105 (1.82) |
389 |
19.2 |
|
Gyeongnam |
58 (2.83) |
9 (0.45) |
23 (1.13) |
4 (0.19) |
78 (3.84) |
172 |
8.5 |
|
Gyeongbuk |
36 (2.34) |
6 (0.36) |
52 (3.51) |
5 (0.34) |
35 (2.23) |
134 |
6.6 |
|
Daegu |
36 (2.50) |
6 (0.40) |
70 (4.78) |
3 (0.19) |
18 (1.25) |
133 |
6.6 |
|
Busan |
47 (2.29) |
9 (0.47) |
24 (1.28) |
3 (0.15) |
38 (1.92) |
121 |
6.0 |
|
Daejeon |
56 (5.81) |
7 (0.73) |
11 (1.16) |
3 (0.31) |
10 (1.07) |
87 |
4.3 |
|
Chungnam |
39 (3.16) |
5 (0.42) |
13 (1.05) |
1 (0.07) |
20 (1.61) |
78 |
3.8 |
|
Incheon |
36 (2.08) |
10 (0.59) |
12 (0.70) |
6 (0.34) |
13 (0.78) |
77 |
3.8 |
|
Jeonnam |
33 (3.05) |
6 (0.49) |
22 (2.07) |
4 (0.37) |
6 (0.49) |
71 |
3.5 |
|
Jeonbuk |
27 (2.46) |
3 (0.30) |
20 (1.78) |
1 (0.08) |
14 (1.25) |
65 |
3.2 |
|
Gwangju |
24 (2.61) |
5 (0.54) |
25 (2.73) |
1 (0.12) |
8 (0.88) |
63 |
3.1 |
|
Gangwon |
25 (2.78) |
1 (0.11) |
14 (1.65) |
2 (0.23) |
15 (1.69) |
57 |
2.8 |
|
Chungbuk |
11 (1.19) |
5 (0.49) |
14 (1.51) |
1 (0.10) |
20 (2.14) |
51 |
2.5 |
|
Ulsan |
13 (1.93) |
1 (0.14) |
6 (0.82) |
0 (0) |
8 (1.19) |
28 |
1.4 |
|
Jeju |
9 (2.35) |
1 (0.25) |
6 (1.82) |
1 (0.23) |
5 (1.48) |
22 |
1.1 |
|
Sejong |
3 (3.36) |
0 (0) |
2 (2.17) |
0 (0) |
0 (0) |
5 |
0.2 |
|
Missing data |
17 |
3 |
3 |
1 |
3 |
27 |
1.3 |
|
Total |
775 |
132 |
517 |
92 |
513 |
2,029 |
100.0 |
DISCUSSION
A few epidemiology studies have evaluated the incidence of congenital bleeding disorders in Korea. Most have been reported by the KHF.
34910 To the best of our knowledge, this is the first nationwide study of the entire population to analyze the incidence of congenital bleeding disorders in Korea using HIRA databases.
The most frequent bleeding disorder found in this study was HA (38%), followed by vWD (25%) and HB (7%). This result is very similar to the WFH 2018 Annual Global Survey, in which HA accounted for 51% (173,711), followed by vWD (23%; 78,547) and HB (10%; 34,289).
4 However, only 5% (135) of those in the KHF are vWD patients, contrasting studies showing that vWD is known to be one of the most common congenital bleeding disorders.
3111213 Given the high prevalence of vWD across ethnic groups, there were very few reported patients.
14 In Korea, 2,423 hemophilia patients were reported in 2018. South Africa and Australia, which have similar numbers of hemophilia patients, reported significantly more vWD patients, with 2,146 and 647, respectively.
4 When patients are diagnosed with congenital bleeding disorders in Korea, registration in the KHF is usually recommended. However, some patients may be reluctant for their disease to be known. Moreover, patients with mild hemophilia or vWD do not feel the need to register with the KHF for treatment because they do not need regular therapy. We found that vWD is likely to be underestimated despite the marked increase in hemophilia patients in Korea determined using nationwide data.
Patients classified as other factor deficiency accounted for a large portion (25%) in our study. Unfortunately, further detailed disease classification was not available due to many limitations in HIRA and NHIS data. A comprehensive study is necessary in order to identify the details of rare congenital bleeding disorders in Korea. Patients with factor XI deficiency accounted for 5% of the total number of patients (92/2,029) recorded for 6 years in this study. According to KHF, registered patients with factor XI deficiency was 0.9% (23/2,458) by 2018 in Korea.
3 Italian Registry of congenital bleeding disorders also reported similar proportion (0.7%, 82/11,000) in factor XI deficiency by 2015.
15
In some countries, the annual prevalence of congenital bleeding disorders has increased in recent decades.
4151617181920 The KHF also reported that the number of registered patients had tripled. While the total Korean population increased by 12%, the KHF data showed a 200% increase in hemophilia from 997 patients in 1991 to 2,148 in 2012.
9 We also found a moderate increase of the estimated ASR in HA from 2010 (1.78/100,000) to 2014 (3.15/100,000) though significant change in the simple number of patients with HA did not show from 2010 to 2015.
After stratifying by age group, the greatest proportion of patients in the WFH 2018 Annual Report was younger than 19 years compared to other age groups.
4 According to the 2018 KHF, 645 (26.3%) of 2,458 registered patients were < 19 years.
3 In our study, the age group with the highest proportion of patients was < 19 years (47.8%), followed by ages 19–39 (24.3%) and 40–59 (18.4%) years. There may be some variation in the age distributions of patients with congenital bleeding disorders across countries. Because they are inherited disorders, they are often diagnosed at an early age. However, some are diagnosed in older patients. The life expectancies of these patients are increasing with active factor therapy, and patients with mild symptoms who are diagnosed at old age are also increasing with advances in diagnostic technology.
The most patients were registered in Gyeonggi (22.1%) and Seoul (19.2%) because these provinces have the largest populations. However, the estimated ASR of HA was the highest in Daejeon (5.81/100,000) and that for vWD was the highest in Daegu and Gyeongbuk, respectively (4.78/100,000 and 3.51/100,000). We guess that it may be affected by the institution according to region. The geographic distribution in other regions was heterogeneous.
There are some limitations to using the HIRA databases. First, the diagnoses of congenital bleeding disorders were based on codes, without laboratory results. Second, other rare congenital bleeding disorders accounting for 25% of the cases in this study, such as deficiencies in factors I, II, V, VII, X, XII, and XIII, were not analyzed separately in this study. It would be better to study these diseases separately in the future. Third, we did not analyze details about congenital bleeding disorders including the prevalence, mortality rate, viral infection due to treatment, classification according to disease severity, trends in the use of factor concentrates, or the cost of congenital bleeding disorders.
Nevertheless, our study is meaningful as it is the first nationwide population-based study of congenital bleeding disorders in Korea. This retrospective study permitted the calculation of more accurate incidences of these diseases in Korea. We also accurately assessed the number of patients with vWD, who have been poorly identified to date. Our data on the incidence of congenital bleeding disorders may give some useful systematic information. A system for collecting more detailed data on congenital bleeding disorders is needed.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download