INTRODUCTION
Spinal surgery tends to be more aggressive and has higher risk than other orthopedic surgeries because it is sensitively related to the neurologic entity and tends to require a longer operation time. Therefore, unpredicted postoperative medical complications often lead to problems, which requires keen awareness. Common gastrointestinal complications after spinal surgery are postoperative ileus, constipation, and fecal impaction with rare complications of acute appendicitis, ascites, colitis, gastrointestinal bleeding, and bowel perforation. Several studies have analyzed the risk factors leading to diverse medical complications after spinal surgery, but most of them looked into incidences of each complication qualitatively, reporting the incidence of gastrointestinal complications ranging from 0.1% to 8.6%.
12345 Among them, reports regarding symptomatic postoperative ileus were relatively frequent, with 2.6%–13.4% incidence after undergoing all spinal procedures, which represented the smallest value in posterior approaches.
678
On the other hand, risk factors or incidences of hepatobiliary complications have yet to be investigated. Serum liver enzymes and total bilirubin levels are checked routinely in postoperative care, as they are often temporarily elevated, though they may be associated with the development of hepatitis, pancreatitis, or acute cholecystitis.
910 Case reports of acute cholecystitis and hepatitis after spinal surgery have previously been reported, but qualitative analysis of associated laboratory testing is yet to be conducted.
1112 Gastrointestinal complications are generally detected and diagnosed through patients' symptoms, whereas elevated serum markers of hepatobiliary complications are often asymptomatic and thought to be temporary, and therefore easily overlooked.
In reviewing our institute's data, presentations of postoperative ileus were frequently observed after spinal fusion surgeries; the results were as expected, but there were also two startling cases of periappendiceal abscess and acute cholecystitis leading to subsequent urgent surgical intervention. The aim of this study is to examine the incidence of gastrointestinal complications after spinal surgery, quantitatively analyze the risk factors of frequent complications, and determine cues requiring early approaches.
METHODS
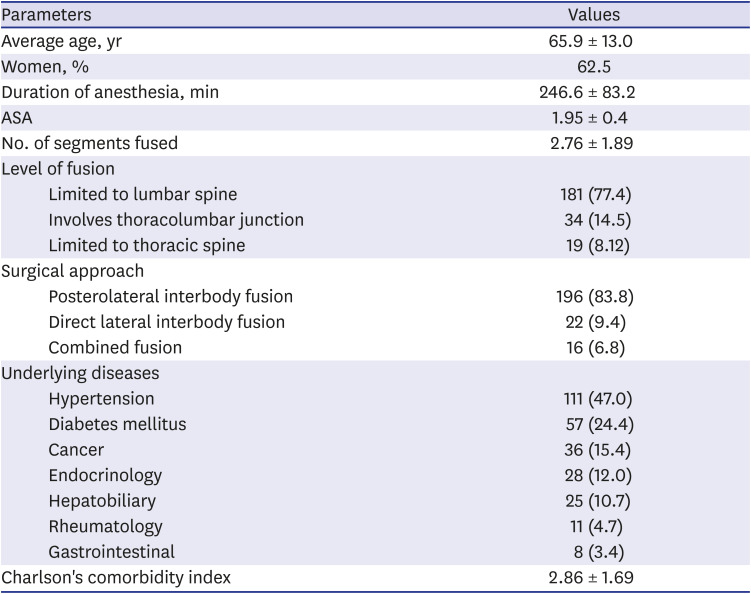
In total, 234 consecutive patients who underwent spine surgery performed by one senior doctor at our institute from January 1st, 2017 to December 31th, 2017 were retrospectively enrolled in the registry with institutional review board approval from the Institutional Review Board. Posterior and direct lateral spinal fusion surgeries on the thoracolumbar and the lumbar spines were included. All operations were performed in prone position under general endotracheal anesthesia. However, lateral decubitus position was performed for direct lateral lumbar interbody fusion (DLIF), followed by consecutive posterolateral interbody fusion (PLIF) in prone position. Eventually, all surgeries were performed in prone position.
The enrolled indications in this study were: 1) posterior instrumentation with or without DLIF and 2) thoracolumbar or lumbar spinal fusion. The excluded indications were: 1) cervical and thoracic fusion only, 2) anterior interbody fusion through a trans-peritoneal approach, 3) spine surgery without posterior instrumented fusion such as diskectomy and laminectomy, and 4) fractures and tumors with neurological complications.
The patients' data were reviewed on the medical charts by a spine fellow and a resident. The following demographic and surgical data were analyzed: age, gender, levels of fused segments, location of fusion (lumbar spine limited, thoracolumbar junction involving, or thoracic spine limited), surgical approaches (posterior, direct lateral, or both), ASA (American Society of Anesthesiologists) physical status classification, and duration of general anesthesia (in hours).
The primary outcomes were presence of paralytic ileus, elevated serum alanine transaminase (ALT) and aspartate transaminase (AST) levels, and elevated total bilirubin levels. The diagnosis of paralytic ileus was confirmed by gastroenterologists under consultation and radiologist's formal reading for plain abdomen radiographs. Liver function tests and total bilirubin levels were investigated. Laboratory results were routinely checked on postoperative day as well as the following day, and these were compared with preoperative data. Serum levels of > 40 unit per liter for ALT, > 45 unit per liter for AST, and > 1.58 mg/dL for total bilirubin levels were considered as elevation according to our institute's diagnostic reference. More than > X2 upper limit of normal levels of ALTs or ASTs were considered to be significant, indicating that further diagnostic evaluation including imaging studies is necessary,
13 whereas > X1 upper limit of normal level was considered to be significant for the total bilirubin.
The underlying diseases of patients were identified by reviewing the anesthesiologist's preoperative assessment charts: the categories were subdivided into hypertension, diabetes mellitus, gastrointestinal, hepatobiliary, endocrinology, rheumatology, and cancer. In addition, diseases were quantified according to the updated Charlson's comorbidity index scoring system.
141516
Univariate logistic regression analyses of all variables were performed for all 234 patients who met the criteria. In turn, significant results were reanalyzed by multivariate logistic regression. The variables used were adjusted with age and gender. P values lower than 0.05 were considered as significant, and all statistical analyses were conducted using R version 3.5.1.
Ethics statement
This study was approved by the Institutional Review Board of the Catholic Medical Center (approval No. KC19RESI0394). Informed consent was waived by the board.
DISCUSSION
Among medical complications, gastrointestinal and hepatobiliary complications are considered to be relatively less common, but they can still lead to life-threatening conditions.
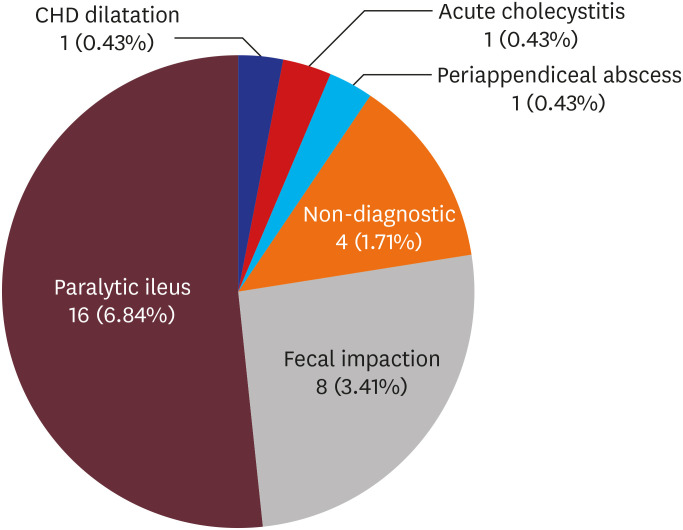
1 In this study, among apparent gastrointestinal and hepatobiliary complications after spinal fusion (13.2%), paralytic ileus (6.8%) and fecal impaction (3.4%) were the most frequently observed for gastrointestinal complications, with no cases of gastrointestinal bleeding, emphasizing its significance in managing paralytic ileus. Regarding hepatobiliary complications, overt liver enzyme elevation was present in roughly one-fourth (26.9%) of total cases, and in about one-eighth (12.4%) for total bilirubin elevation (
Tables 1 and
2). The complications were not significantly different according to age, gender, approaches, surgical approaches, location of fusion, or Charlson's comorbidity index. Several studies have reported the incidences of paralytic ileus after spinal fusion surgery. A cohort study of 220,522 lumbar fusions revealed 3.5% total incidence of postoperative paralytic ileus,
17 with 2.6% after posterior lumbar fusions (PLFs) and 7.5% after anterior lumbar fusions (ALFs). Earlier studies reported a higher incidence of 14.8% in 121 ALFs.
18
The mechanism of postoperative ileus is mainly functional (paralytic), which is a reversible disturbance manifesting from the third to fifth day after surgery that frequently presents as abdominal pain, nausea, vomiting, abdominal distension, or constipation (fecal impaction).
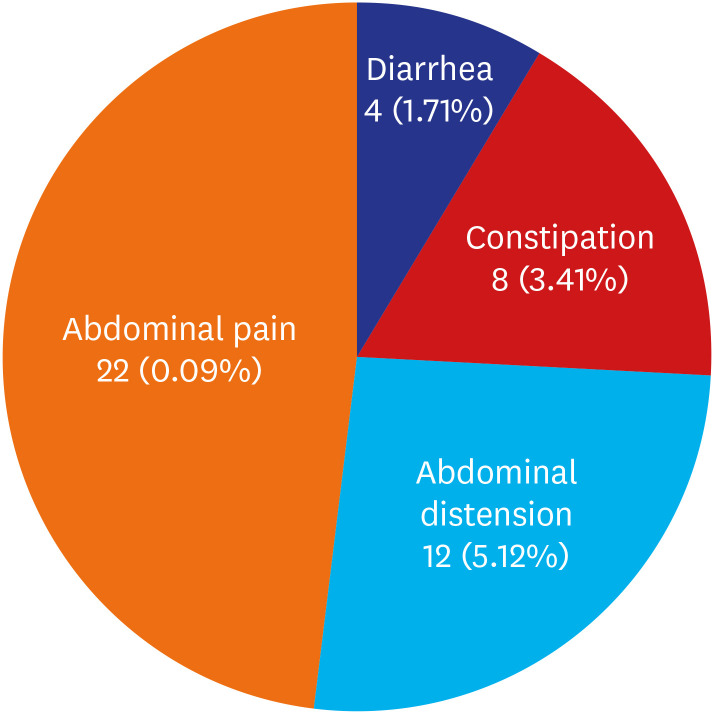
19 In our study, 22 patients out of 31 diagnosed complications (71%) complained of abdominal pain (
Table 1). Gastrointestinal tract motility may be reduced, leading to paralytic ileus partly by surgery, partly by the residual effects of anesthetic agents, and particularly by opioids administered for postoperative pain relief.
20 An additionally suggested mechanism is that spinal manipulations including mid to lower thoracic levels or upper lumbar levels might provoke and damage splanchnic nerves, resulting in decreased gastrointestinal motility and reactive ileus.
2 On the other hand, avoiding early oral intake after surgery is known to be a simple prevention strategy for the postoperative ileus.
3 Treatments for postoperative ileus include nothing per os (NPO), application of nasogastric tubes, early enteral nutrition, early mobilization, administration of metoclopramide, cisapride, opiate antagonist, laxatives, and even nonsteroidal anti-inflammatory drugs.
21
Older age, men, and circumferential fusion compared to discrete anterior or posterior approaches for fusion have been reported to be risk factors for ileus.
17 Moreover, total estimated blood loss and total opiate dosage have also been reported as risk factors.
22 Postoperative pain control in our study was mostly achieved by patient controlled analgesia (PCA) composed of fentanyl and ramosetron, with additional per re nata tramadol or pethidine injections for postoperative pain control. Opioids are well known to induce bowel dysfunction by the activation of mu-opioid receptors in the gastrointestinal tract.
23
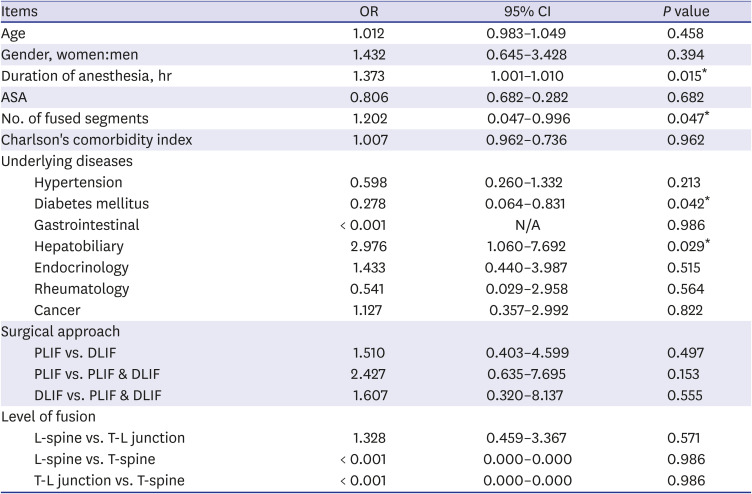
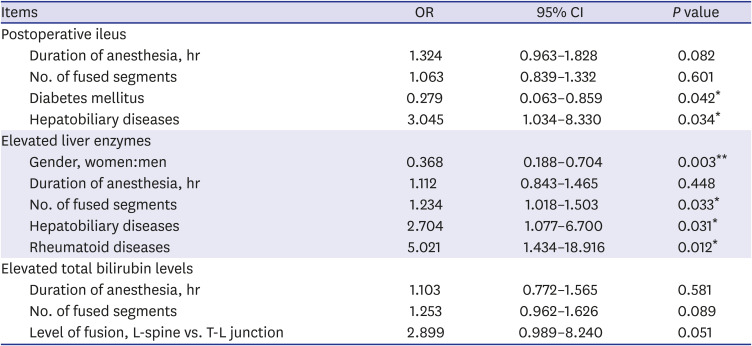
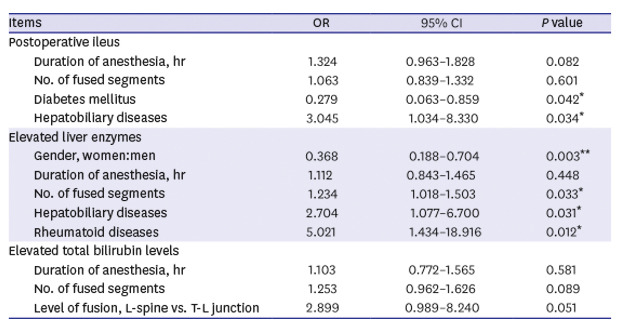
Univariate logistic regression analyses revealed that duration of anesthesia, number of segments fused, and hepatobiliary complications are risk factors of postoperative paralytic ileus, while age, gender, and circumferential approaches are not. A doubtful result of reduced risks in underlying diabetes mellitus (OR, 0.278;
P = 0.042) was also confirmed by multivariate logistic regression analysis (
Table 5), contradicting our previously held knowledge regarding increased oxidative stress in diabetic patients which leads to decreased bowel motility.
17242526 The result might suggest a false negative, indicating the need for further analysis with a larger sized study. However, the associated contingency table shows that only three of 57 diabetic patients developed postoperative ileus, while 28 were present among 177 non-diabetic patients. Considering that the sample size is not too small, the possibility of an unexplained mechanism still exists.
Table 5
Multiple logistic regression for risk factors with significant result from univariate logistic regression analysis for each outcomes
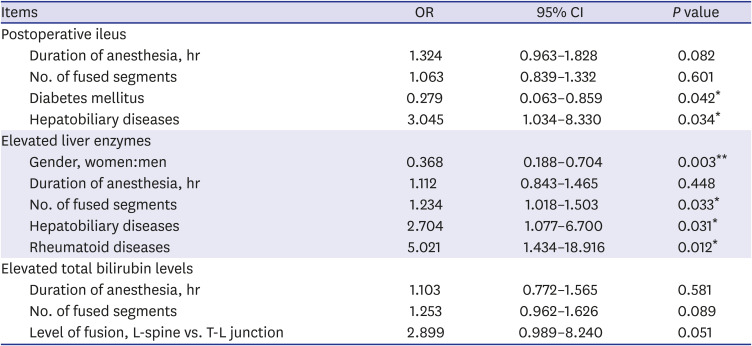
|
Items |
OR |
95% CI |
P value |
|
Postoperative ileus |
|
|
|
|
Duration of anesthesia, hr |
1.324 |
0.963–1.828 |
0.082 |
|
No. of fused segments |
1.063 |
0.839–1.332 |
0.601 |
|
Diabetes mellitus |
0.279 |
0.063–0.859 |
0.042*
|
|
Hepatobiliary diseases |
3.045 |
1.034–8.330 |
0.034*
|
|
Elevated liver enzymes |
|
|
|
|
Gender, women:men |
0.368 |
0.188–0.704 |
0.003**
|
|
Duration of anesthesia, hr |
1.112 |
0.843–1.465 |
0.448 |
|
No. of fused segments |
1.234 |
1.018–1.503 |
0.033*
|
|
Hepatobiliary diseases |
2.704 |
1.077–6.700 |
0.031*
|
|
Rheumatoid diseases |
5.021 |
1.434–18.916 |
0.012*
|
|
Elevated total bilirubin levels |
|
|
|
|
Duration of anesthesia, hr |
1.103 |
0.772–1.565 |
0.581 |
|
No. of fused segments |
1.253 |
0.962–1.626 |
0.089 |
|
Level of fusion, L-spine vs. T-L junction |
2.899 |
0.989–8.240 |
0.051 |
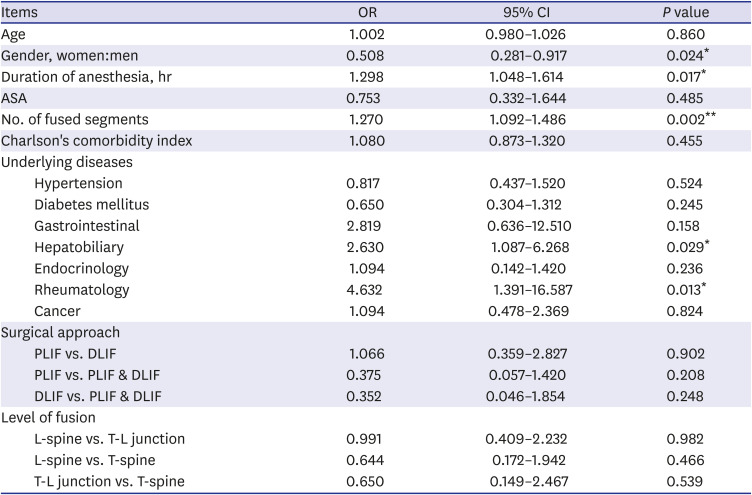
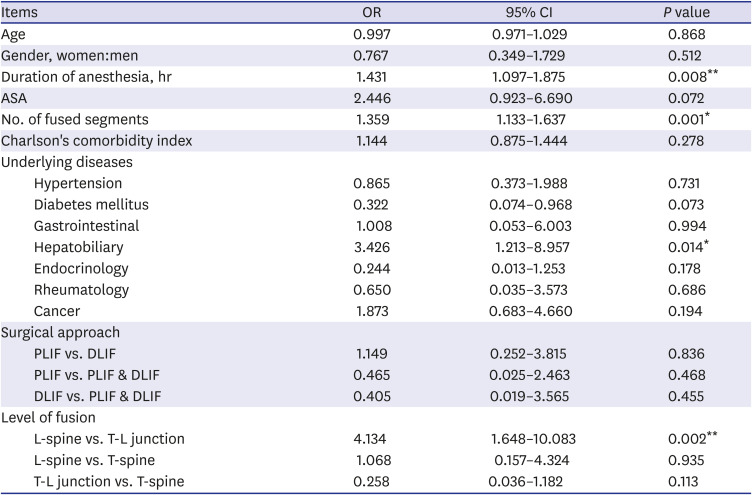
For postoperatively elevated liver enzymes, multivariate logistic regression revealed that men, number of fused segments, underlying hepatobiliary diseases, and rheumatoid diseases were risk factors (
Table 5). Hepatobiliary diseases would certainly accelerate the rise, but a notable result of rheumatoid diseases is accounted for by the relatively excess load of hepatotoxic medications used for the treatment. The only risk factor identified of postoperatively elevated serum total bilirubin levels after multiple logistic regression was fusions involving thoracolumbar junctions (
Table 5). A mechanism that may be suggested for the latter is manipulation of splanchnic nerves from celiac plexus arising from lower thoracic levels affecting the metabolism of hepatobiliary functions.
Abdominal pain after spinal surgery is a popular subject demanding doctor's attention for patients on postoperative care. In majority of cases, the symptoms can be easily relieved by simple prescriptions or conservative management, or they are spontaneously regressed by an unknown mechanism. However, the indifference and ignorance of the doctor in charge might lead to a crisis, as they could have had various chances to prevent issues.
Gastrointestinal and hepatobiliary complications can be prevented in number of ways, but it cannot be fully prevented, since surgical interventions under general anesthesia have inevitable consequences themselves. Disease entities which will later develop into a condition requiring immediate interventions are hidden in between the majority of naturally or easily subsiding symptoms. Hence, even a simple abdominal pain must not be neglected. Basic approaches of careful physical examinations, plain abdominal radiograph, follow-up blood tests, and early CT scans in doubtful conditions accompanied by inter-department consultations will lead to providential cut off devastating consequences. Thus, the most predisposing factor of developing comorbidities might be the carefulness and keen awareness of the treating physician.
This study was limited to patients who complained of abdominal pain that developed during one year after spine surgery. However, the findings of this study suggest a new level of importance in scrutinizing the methods involved in evaluating patients who complain of abdominal pain and avoiding the dismissal of pain that may initially seem trivial. The reason for such limitation was that the preliminary results have clearly shown the possibility of developing pain in this short time frame, and the results between this study and those with longer time frames were statistically insignificant. In addition, the two patients that described the development of serious pain in a short time frame further undermined the need for a larger sample size, even though these occurrences were very rare.
In conclusion, patients on postoperative care after spinal surgery should receive direct attention as soon as possible after manifesting abdominal symptoms. Laboratory and radiologic results must be carefully reviewed, and early consultation to gastroenterologists or general surgeons is recommended to avoid preventable complications.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download