INTRODUCTION
Atelectasis develops in up to 90% of patients undergoing general anesthesia (GA) depending on the surgical procedure and patient characteristics. It plays an important role in ventilation–perfusion mismatch and in the development of intraoperative hypoxia and postoperative pulmonary complications (PPCs).
12 In recent decades, since the establishment of lung-protective mechanical ventilation using low tidal volume to reduce mortality in patients with acute respiratory distress syndrome (ARDS), there has been a trend toward decreasing tidal volumes during surgery.
3 While conventional ventilation (CV) with high tidal volume has traditionally been advocated to prevent intraoperative atelectasis,
4 low tidal volume ventilation can contribute to the development of atelectasis.
56 Numerous studies investigating intraoperative low tidal volume ventilation combined with various levels of positive end-expiratory pressure (PEEP) and/or recruitment maneuvers (RMs) to reduce the incidence of PPCs have yielded conflicting results.
789 An imaging study that assesses whether intraoperative ventilation strategies actually influence the occurrence of atelectasis could support the interpretation of these inconsistent results.
10
Lung ultrasonography has been suggested as an accurate bedside point-of-care method for diagnosing anesthesia-induced atelectasis and tracking respiratory complications compared to gold standards, such as computed tomography (CT) and magnetic resonance imaging (MRI).
211 It was reported that lung ultrasonography can reliably detect anesthesia-induced atelectasis with a sensitivity, specificity, and diagnostic accuracy of about 90% in comparative studies with CT
12 or MRI.
11 Anesthesia-induced atelectasis is typically minor and is not seen in conventional chest radiographs unless it becomes severe.
1 Compared to the current standard diagnostic imaging method, i.e., chest radiography, lung ultrasonography exhibits superior detection of clinically relevant PPCs requiring treatment after cardiothoracic surgery.
13 This suggests that this method can be used as the primary imaging technique for diagnosing PPCs and enhancing bedside decision making.
To the best of our knowledge, the effects of protective ventilation (PV) using low tidal volume on the occurrence of atelectasis in adult patients without lung injury have not been evaluated using bedside lung sonography. We hypothesized that ventilation using low tidal volume may be associated with more atelectasis during open abdominal surgery. In this study, we assessed the effects of PV techniques on anesthesia-induced atelectasis identified via lung ultrasonography in patients undergoing abdominal surgery.
Go to :

METHODS
Study design and participants
This prospective randomized controlled study was conducted between October 2018 and August 2019. Patients aged ≥ 19 years with American Society of Anesthesiologists physical status I to III, who were scheduled for open abdominal surgery with an expected duration > 2 hours, were enrolled. Exclusion criteria included patient refusal, body mass index > 40 kg/m2, history of thoracic surgery, severe obstructive pulmonary disease, difficulty cooperating, nervous system disease, diaphragmatic paralysis, and a history of mechanical ventilation within 1 month preceding surgery.
Randomization
Patients were randomly assigned by computer to receive either CV or PV. A researcher not associated with the study performed a random allocation sequence using a computer random number generator with an allocation ratio of 1:1 and sealed opaque envelopes for allocation concealment. The anesthesiologist who performed lung ultrasonography, the patients, and their guardians were blinded to the group allocation.
Lung ultrasonography
Lung ultrasonography was performed at four time points: before the induction of GA (time point A; room air); 5 minutes after the induction of GA (time point B; fraction of inspired oxygen: FiO
2 0.5); at the end of surgery before emergence from anesthesia (time point C; FiO
2 0.5); and 1 hour after emergence from anesthesia in the recovery room (time point D; mask 6 L/min). It was performed by a single anesthesiologist who had performed more than 100 lung ultrasound (LUS) scan procedures using the X-Porte instrument (Sonosite, Bothell, WA, USA) and a high-frequency linear array probe (6–13 MHz). The classic lung sonographic approach was used to reveal the pleura and lung tissue between the acoustic shadows of two adjacent ribs (the bat sign). An oblique scan along the intercostal space was also used to examine the region hidden in the acoustic shadows of adjacent ribs. For the posterobasal region of the lung, the probe was placed within the intercostal space above the corresponding hemidiaphragm and immediately below the posterior axillary line to better assess posterior paradiaphragmatic atelectasis.
11
The presence of B-line and juxtapleural consolidation are the most commonly used findings to examine anesthesia-induced atelectasis. We used a modified LUS scoring system with these two findings as described previously.
14 The default scan depth was initially set to 4.8 cm and was adjusted to a suitable level for each patient. If B-lines were suspected, the depth of the scan was adjusted appropriately and checked to determine whether it erased A-lines and moved in synchrony with respiratory movements to exclude artifacts.
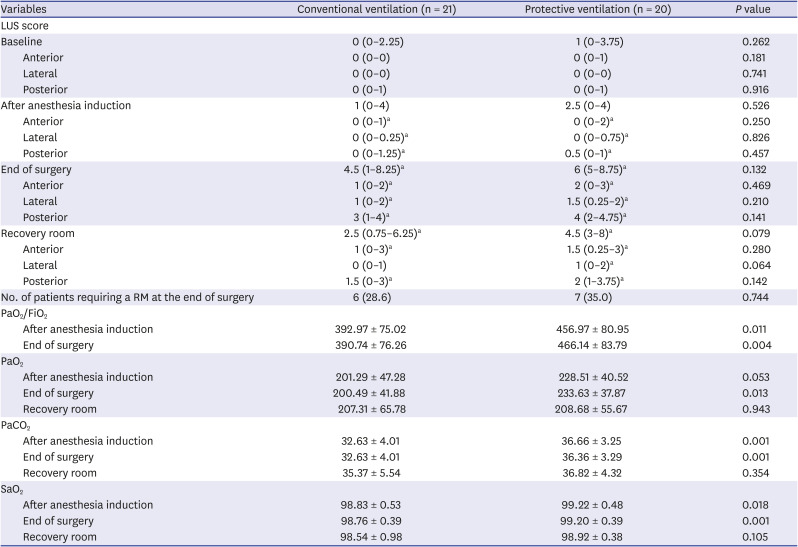
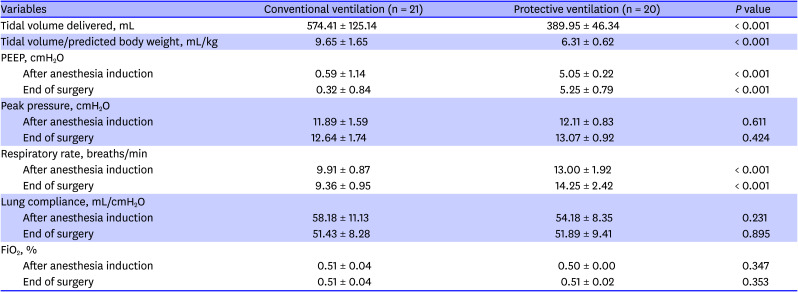
15 Each hemithorax was divided into six quadrants using two longitudinal lines (anterior and posterior axillary) and one axial line at the level of the nipples: the anterior, lateral, and posterior parts were separately divided into the upper and lower parts of the right and left lungs. Each of 12 quadrants was assigned a score of 0 to 3 as follows (
Fig. 1): 0, normal aeration (0–2 B lines); 1, small loss of aeration (≥ 3 B lines or small juxtapleural consolidations separated by a normal pleural line); 2, moderate loss of aeration (coalescent B lines or multiple small juxtapleural consolidations separated by a thickened or irregular pleural line); 3, severe loss of aeration (consolidation). All intercostal spaces in each region were checked, and the area of poorest aeration was recorded. Individual LUS scores from each quadrant were summed to calculate a total LUS score, which ranged from 0 to 36. If the LUS score at the end of surgery before emergence from anesthesia was ≥ 2 points in any region, we considered RMs to be required to re-expand atelectasis. For these patients, RMs involved applying airway pressure 30 cmH
2O for 30 seconds without changing FiO
2.
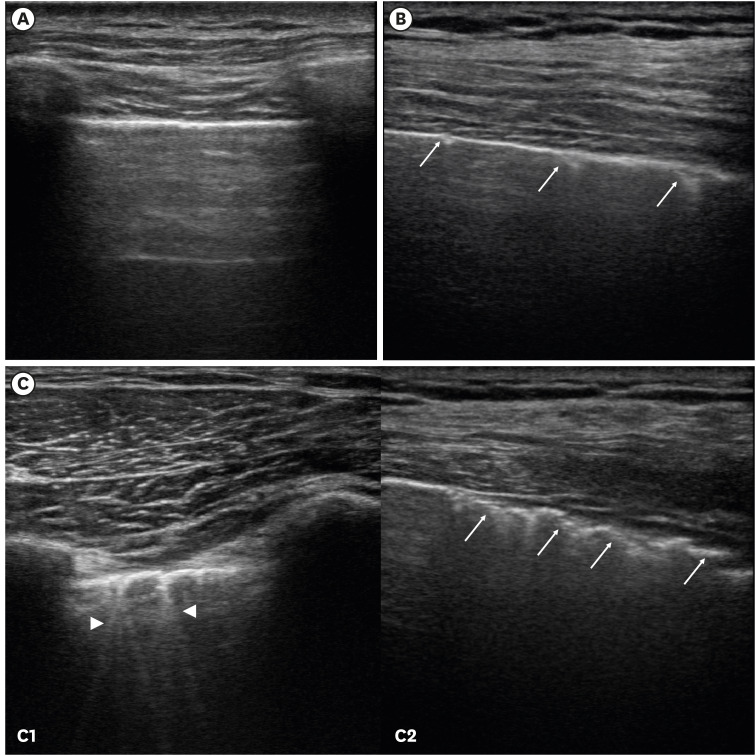 | Fig. 1
LUS score. The degree of aeration loss was graded depending on juxtapleural consolidation (arrow) and B lines (arrow head). (A) 0, normal aeration (0–2 B lines); (B) 1, small loss of aeration (≥ 3 B lines or multiple small juxtapleural consolidations separated by a normal pleural line); (C) 2, moderate loss of aeration (C1: coalescent B lines or C2: multiple small juxtapleural consolidations separated by a thickened or irregular pleural line); No patients exhibited severe loss of aeration corresponding to a LUS score of 3 points.
LUS = lung ultrasound.

|
Anesthesia
After intravenous injection of glycopyrrolate 0.2 mg and midazolam 3 mg, GA was induced using propofol 2 mg/kg and fentanyl 1–2 μg/kg. Tracheal intubation was facilitated with rocuronium 0.6 mg/kg. Patients received either CV group (a tidal volume of 9–10 mL/kg predicted body weight [PBW] with no PEEP) or PV group (a tidal volume of 6–8 mL/kg PBW and PEEP 5 cmH
2O) via pressure-controlled ventilation with volume guaranteed (PCV-VG) using an AVANCE CS2 anesthesia machine (GE Healthcare, Wauwatosa, WI, USA) according to the group assignment. Each patient's PBW was calculated using a previously defined formula.
16 Anesthesia was maintained with sevoflurane (1.5–2.5 vol%) in a 50% oxygen/air mixture at a flow rate of 3 L/min to maintain a bispectral index of 40–60 and blood pressure within 20% of the baseline value. Ventilation was controlled to maintain end-tidal carbon dioxide between 30 and 40 mmHg. When arterial desaturation (defined as peripheral oxygen saturation ≤ 92%) developed, an increase in the FiO
2 and the use of RMs were permitted. An intravenous fluid bolus of 5 mL/kg per hour was administered at anesthesia induction. Crystalloid solutions at a dose of 8–10 mL/kg per hour were used as maintenance fluid intraoperatively. Bolus colloid or blood could be used to replace blood loss intraoperatively at the anesthesiologist's discretion. Upon the conclusion of surgery, patients were extubated in the operating room after reversal of residual muscle relaxation using pyridostigmine and glycopyrrolate. Train-of-four stimulation was used to assess the presence of residual neuromuscular block, with a train-of-four ratio ≥ 0.9 considered suitable for extubation. In the recovery room, oxygen was delivered via mask at 6 L/min and postoperative analgesia was provided with fentanyl and nonsteroidal anti-inflammatory drugs at the patient's request. At two time points (B and C), mechanical ventilation parameters, including tidal volume, respiratory rate, PEEP, lung compliance, peak inspiratory pressure, and end-inspiratory plateau pressure, were collected with the spirometer built into the anesthesia ventilator. Vital signs, results of arterial blood gas analyses, and FiO
2 were noted at each ultrasonographic examination. The presence and severity of pain in the recovery room were assessed with a numeric rating scale (0–10).
Statistical analyses
SPSS version 22.0 was used for statistical analyses. The primary endpoint was the modified LUS score assessed at the end of surgery. The secondary outcomes were the LUS score at time points B and D, and the number of patients requiring RMs. Based on our preliminary data with five patients in each group, we expected LUS scores of 5.5 ± 0.9 points with CV and 6.6 ± 0.9 points with PV at the end of surgery. Therefore, a sample size of 19 patients (α = 0.05, power = 95%) per group was calculated (two-tailed t-test). Correction for dropouts suggested the need for 21 patients per group. Categorical variables were analyzed using the χ2 or Fisher's exact tests. Continuous variables were analyzed using the t-test or the Mann-Whitney U test after assessment for normality, and results are presented as means ± standard deviations or medians with interquartile ranges (IQRs), as appropriate. The LUS scores of the anterior, lateral, posterior, and total lung parts measured at each time point were analyzed by repeated measures analyses of variance followed by Bonferroni correction. To assess the relationship between the change in LUS score and the change in PaO2/FiO2 ratio, we calculated the changes between time points B and C, and then calculated the Spearman's correlation coefficient (rs). In all analyses, two-sided P < 0.05 was taken to indicate statistical significance.
Ethics statement
This study was approved by the local ethics committee of Ewha Womans University, Seoul, Korea (EUMC 2018-07-087-001) on September 21, 2018. The trial was registered with the Clinical Trial Registry of Korea (No. KCT0003746), and all patients provided written informed consent. The study was conducted in accordance with the tenets of the Declaration of Helsinki without any deviation from the study protocol.
Go to :

RESULTS
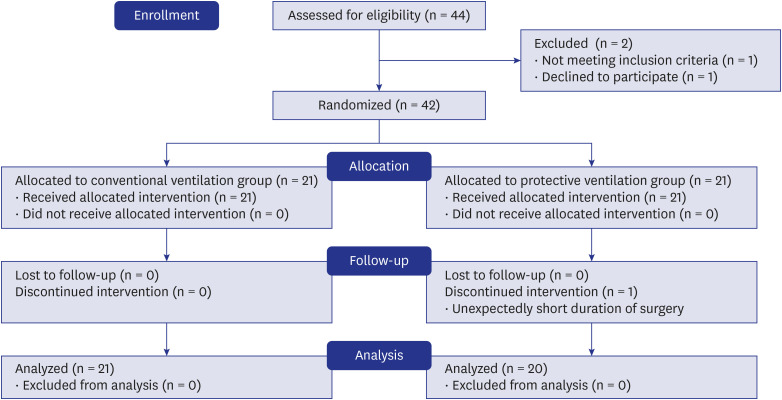
Of 44 patients assessed for eligibility, 42 were enrolled in the analyses. One patient was excluded because he had an unexpectedly short duration of surgery.
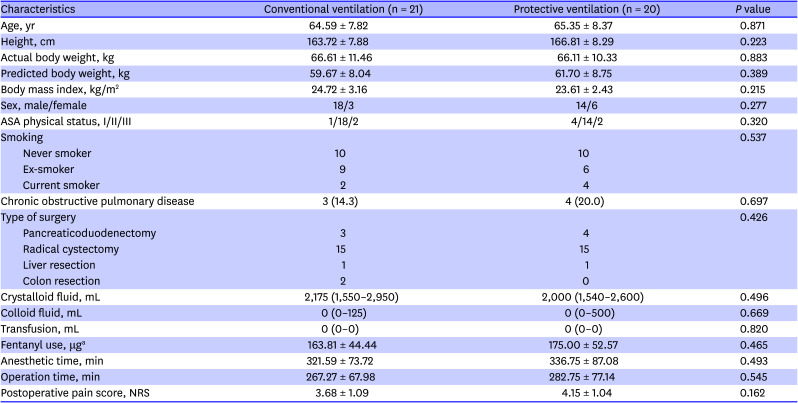
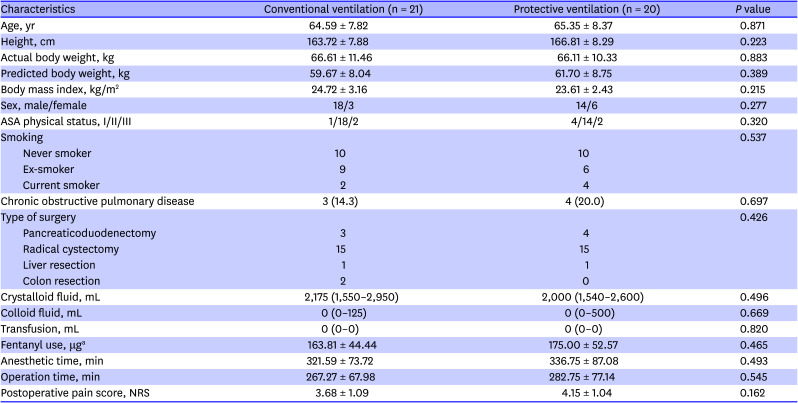
Fig. 2 illustrates the allocation process according to the Consolidated Standards of Reporting Trials statement. Baseline characteristics were well balanced between the two groups. Perioperative clinical details such as total fluid intake, duration of operation and anesthesia, and postoperative pain score were also similar between the groups (
Table 1).
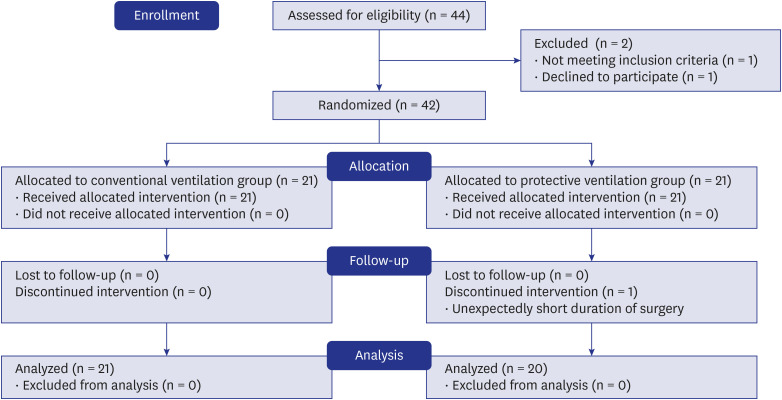 | Fig. 2 The consolidated standards of reporting trials statement.
|
Table 1
Patient characteristics and perioperative data
|
Characteristics |
Conventional ventilation (n = 21) |
Protective ventilation (n = 20) |
P value |
|
Age, yr |
64.59 ± 7.82 |
65.35 ± 8.37 |
0.871 |
|
Height, cm |
163.72 ± 7.88 |
166.81 ± 8.29 |
0.223 |
|
Actual body weight, kg |
66.61 ± 11.46 |
66.11 ± 10.33 |
0.883 |
|
Predicted body weight, kg |
59.67 ± 8.04 |
61.70 ± 8.75 |
0.389 |
|
Body mass index, kg/m2
|
24.72 ± 3.16 |
23.61 ± 2.43 |
0.215 |
|
Sex, male/female |
18/3 |
14/6 |
0.277 |
|
ASA physical status, I/II/III |
1/18/2 |
4/14/2 |
0.320 |
|
Smoking |
|
|
0.537 |
|
Never smoker |
10 |
10 |
|
Ex-smoker |
9 |
6 |
|
Current smoker |
2 |
4 |
|
Chronic obstructive pulmonary disease |
3 (14.3) |
4 (20.0) |
0.697 |
|
Type of surgery |
|
|
0.426 |
|
Pancreaticoduodenectomy |
3 |
4 |
|
Radical cystectomy |
15 |
15 |
|
Liver resection |
1 |
1 |
|
Colon resection |
2 |
0 |
|
Crystalloid fluid, mL |
2,175 (1,550–2,950) |
2,000 (1,540–2,600) |
0.496 |
|
Colloid fluid, mL |
0 (0–125) |
0 (0–500) |
0.669 |
|
Transfusion, mL |
0 (0–0) |
0 (0–0) |
0.820 |
|
Fentanyl use, μga
|
163.81 ± 44.44 |
175.00 ± 52.57 |
0.465 |
|
Anesthetic time, min |
321.59 ± 73.72 |
336.75 ± 87.08 |
0.493 |
|
Operation time, min |
267.27 ± 67.98 |
282.75 ± 77.14 |
0.545 |
|
Postoperative pain score, NRS |
3.68 ± 1.09 |
4.15 ± 1.04 |
0.162 |

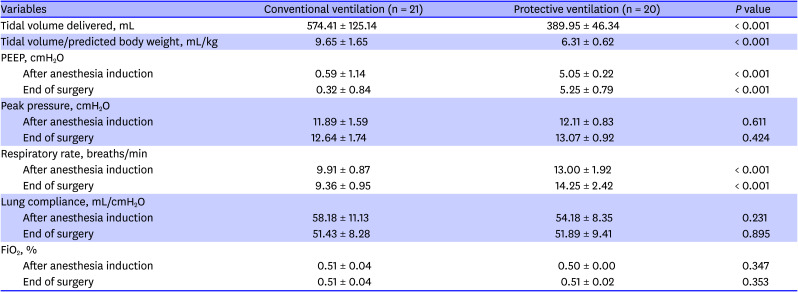
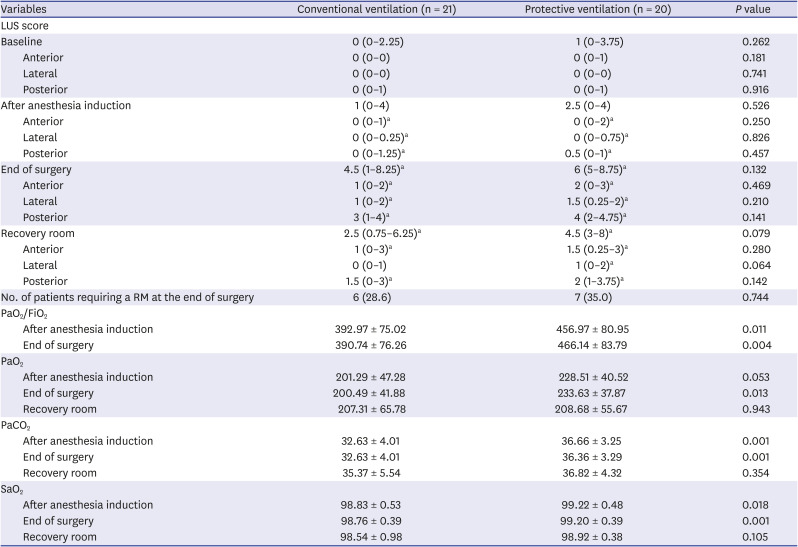
As shown in
Table 2, tidal volume delivered to patients differed significantly between the groups: 574.41 ± 125.14 mL (9.65 ± 1.65 mL/kg of PBW) in the CV group and 389.95 ± 46.34 mL (6.31 ± 0.62 mL/kg of PBW) in the PV group (
P < 0.001). PEEP applied at the end of surgery was 0.32 ± 0.84 cmH
2O in the CV group and 5.25 ± 0.79 cmH
2O in the PV group. Peak airway pressure, lung compliance, and FiO
2 delivered were similar between the two groups.
Table 2
Perioperative data
|
Variables |
Conventional ventilation (n = 21) |
Protective ventilation (n = 20) |
P value |
|
Tidal volume delivered, mL |
574.41 ± 125.14 |
389.95 ± 46.34 |
< 0.001 |
|
Tidal volume/predicted body weight, mL/kg |
9.65 ± 1.65 |
6.31 ± 0.62 |
< 0.001 |
|
PEEP, cmH2O |
|
|
|
|
After anesthesia induction |
0.59 ± 1.14 |
5.05 ± 0.22 |
< 0.001 |
|
End of surgery |
0.32 ± 0.84 |
5.25 ± 0.79 |
< 0.001 |
|
Peak pressure, cmH2O |
|
|
|
|
After anesthesia induction |
11.89 ± 1.59 |
12.11 ± 0.83 |
0.611 |
|
End of surgery |
12.64 ± 1.74 |
13.07 ± 0.92 |
0.424 |
|
Respiratory rate, breaths/min |
|
|
|
|
After anesthesia induction |
9.91 ± 0.87 |
13.00 ± 1.92 |
< 0.001 |
|
End of surgery |
9.36 ± 0.95 |
14.25 ± 2.42 |
< 0.001 |
|
Lung compliance, mL/cmH2O |
|
|
|
|
After anesthesia induction |
58.18 ± 11.13 |
54.18 ± 8.35 |
0.231 |
|
End of surgery |
51.43 ± 8.28 |
51.89 ± 9.41 |
0.895 |
|
FiO2, % |
|
|
|
|
After anesthesia induction |
0.51 ± 0.04 |
0.50 ± 0.00 |
0.347 |
|
End of surgery |
0.51 ± 0.04 |
0.51 ± 0.02 |
0.353 |

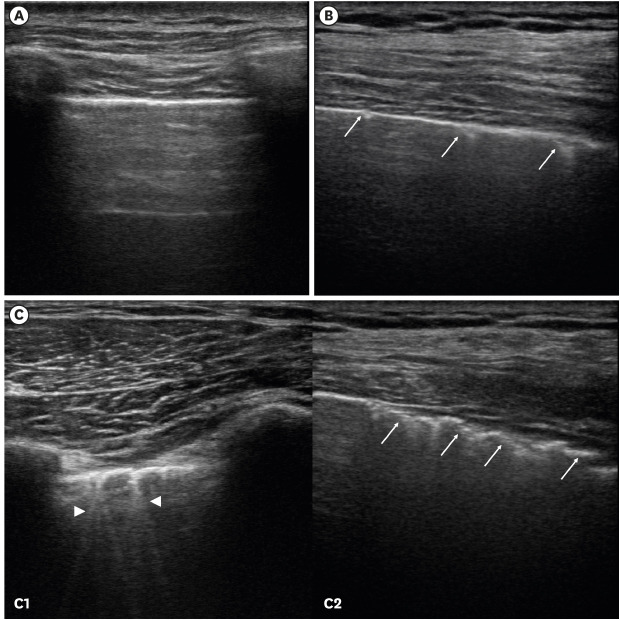
As shown in
Table 3, total LUS scores at the end of surgery were 4.5 (IQR: 1–8.25) points in the CV group and 6 (IQR: 5–8.75) points in the PV group, which were not significantly different (
P = 0.132). The LUS scores were also not significantly different between groups after anesthesia induction (1 [IQR: 0–4] points vs. 2.5 [IQR: 0–4] points, respectively,
P = 0.526) or in the recovery room (2.5 [IQR: 0.75–6.25] points vs. 4.5 [IQR: 3–8] points, respectively,
P = 0.079). In both groups, total LUS score did not significantly differ after anesthesia induction but did significantly increase at the end of surgery compared to the baseline value (
P < 0.001). It decreased after emergence from anesthesia but remained higher than baseline (
P < 0.001). When the LUS scores of three longitudinal regions (anterior, lateral, posterior) were analyzed separately, the LUS score increased significantly after anesthesia induction and further increased at the end of surgery in each of the three regions.
Table 3
LUS score and the number of patients requiring a RM
|
Variables |
Conventional ventilation (n = 21) |
Protective ventilation (n = 20) |
P value |
|
LUS score |
|
|
|
|
Baseline |
0 (0–2.25) |
1 (0–3.75) |
0.262 |
|
Anterior |
0 (0–0) |
0 (0–1) |
0.181 |
|
Lateral |
0 (0–0) |
0 (0–0) |
0.741 |
|
Posterior |
0 (0–1) |
0 (0–1) |
0.916 |
|
After anesthesia induction |
1 (0–4) |
2.5 (0–4) |
0.526 |
|
Anterior |
0 (0–1)a
|
0 (0–2)a
|
0.250 |
|
Lateral |
0 (0–0.25)a
|
0 (0–0.75)a
|
0.826 |
|
Posterior |
0 (0–1.25)a
|
0.5 (0–1)a
|
0.457 |
|
End of surgery |
4.5 (1–8.25)a
|
6 (5–8.75)a
|
0.132 |
|
Anterior |
1 (0–2)a
|
2 (0–3)a
|
0.469 |
|
Lateral |
1 (0–2)a
|
1.5 (0.25–2)a
|
0.210 |
|
Posterior |
3 (1–4)a
|
4 (2–4.75)a
|
0.141 |
|
Recovery room |
2.5 (0.75–6.25)a
|
4.5 (3–8)a
|
0.079 |
|
Anterior |
1 (0–3)a
|
1.5 (0.25–3)a
|
0.280 |
|
Lateral |
0 (0–1) |
1 (0–2)a
|
0.064 |
|
Posterior |
1.5 (0–3)a
|
2 (1–3.75)a
|
0.142 |
|
No. of patients requiring a RM at the end of surgery |
6 (28.6) |
7 (35.0) |
0.744 |
|
PaO2/FiO2
|
|
|
|
|
After anesthesia induction |
392.97 ± 75.02 |
456.97 ± 80.95 |
0.011 |
|
End of surgery |
390.74 ± 76.26 |
466.14 ± 83.79 |
0.004 |
|
PaO2
|
|
|
|
|
After anesthesia induction |
201.29 ± 47.28 |
228.51 ± 40.52 |
0.053 |
|
End of surgery |
200.49 ± 41.88 |
233.63 ± 37.87 |
0.013 |
|
Recovery room |
207.31 ± 65.78 |
208.68 ± 55.67 |
0.943 |
|
PaCO2
|
|
|
|
|
After anesthesia induction |
32.63 ± 4.01 |
36.66 ± 3.25 |
0.001 |
|
End of surgery |
32.63 ± 4.01 |
36.36 ± 3.29 |
0.001 |
|
Recovery room |
35.37 ± 5.54 |
36.82 ± 4.32 |
0.354 |
|
SaO2
|
|
|
|
|
After anesthesia induction |
98.83 ± 0.53 |
99.22 ± 0.48 |
0.018 |
|
End of surgery |
98.76 ± 0.39 |
99.20 ± 0.39 |
0.001 |
|
Recovery room |
98.54 ± 0.98 |
98.92 ± 0.38 |
0.105 |

There was no statistically significant difference between the groups in the number of patients requiring RMs at the end of surgery (LUS score ≥ 2 points in any region): 6 patients (28.6%) in the CV group and 7 patients (35%) in the PV group. Among these 13 patients, LUS scores ≥ 2 points were observed most frequently in the lower posterior region (92%), followed by the upper posterior region (23.07%), and lower lateral region (23.07%). No patient had a LUS score of 3 points in any region.
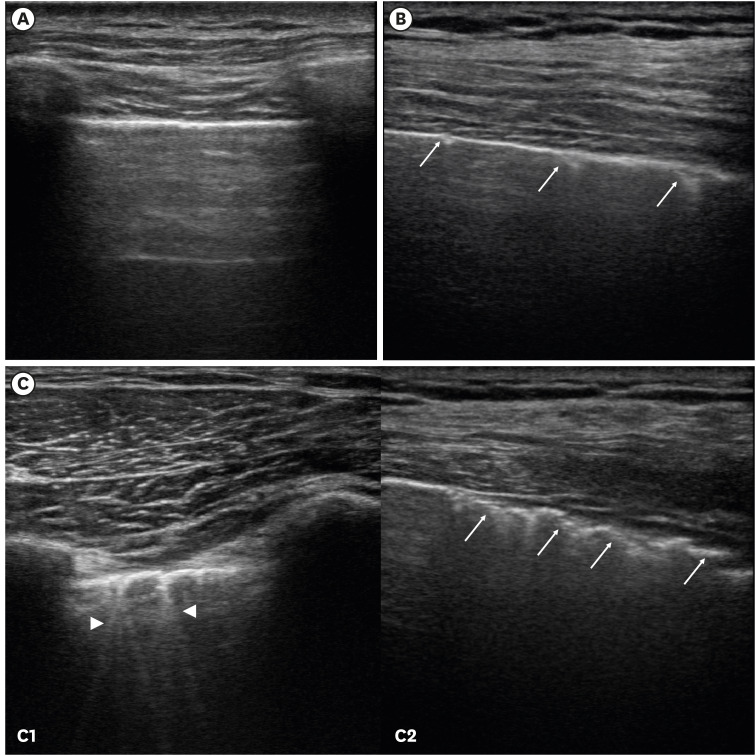
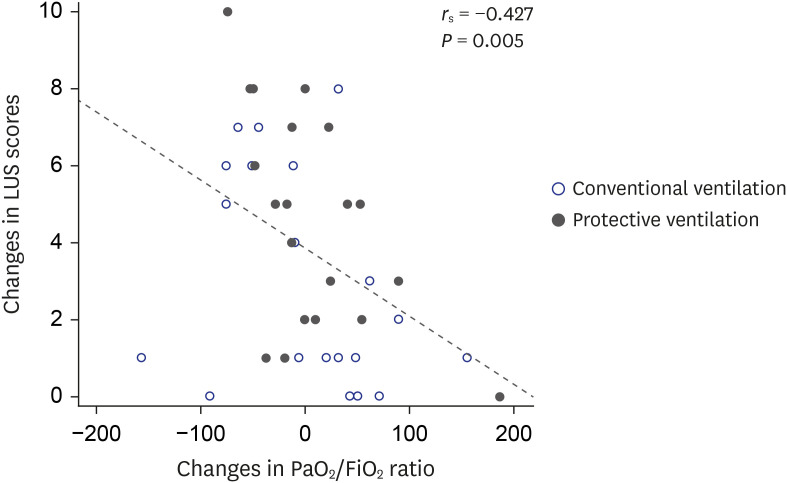
During the study period, arterial desaturation did not occur in any patient. Therefore, RMs were not used except in patients with LUS score ≥ 2 points in any region at the end of surgery. Arterial blood gas analyses showed significantly higher PaO
2/FiO
2, PaCO
2, and SaO
2 at time points B and C in the PV group, and this difference was not observed in the recovery room. As shown in
Fig. 3, the changes in the LUS scores were moderately correlated with the changes in the PaO
2/FiO
2 ratio between time points B and C (
rs = −0.427,
P = 0.005).
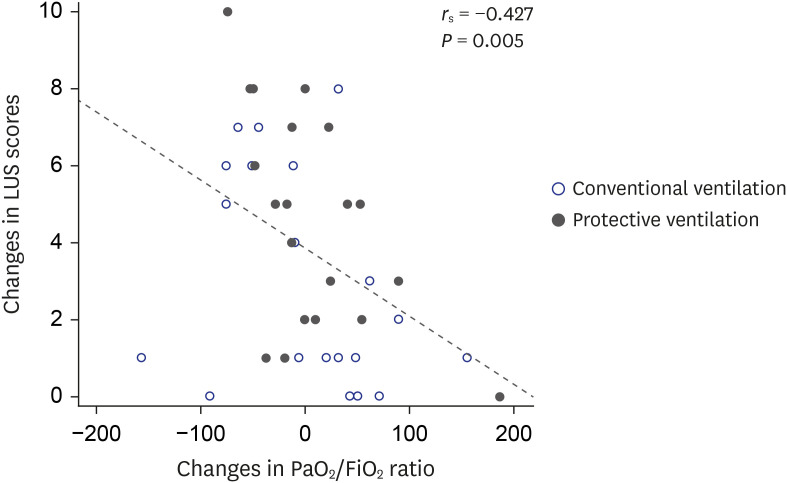 | Fig. 3
Relationship between the changes in the LUS scores and the changes in the PaO2/FiO2 ratio using Spearman's correlation coefficients (rs). The change was calculated between 5 minutes after anesthesia induction and the end of surgery.
LUS = lung ultrasound.

|
Go to :

DISCUSSION
This prospective randomized study demonstrated that ventilation with low tidal volume (6.31 ± 0.62 mL/kg PBW) with 5 cmH2O PEEP brought about similar loss of aeration compared to high tidal volume ventilation (9.65 ± 1.65 mL/kg PBW) in patients undergoing open abdominal surgery. The number of patients who needed RMs at the end of the surgery was similar between those receiving high tidal volume and those receiving low tidal volume with PEEP. Aeration loss was predominantly distributed in dependent lung areas without significant differences between the two groups.
To the best of our knowledge, only one previous study has assessed the effects of low tidal volume ventilation on anesthesia-induced atelectasis identified by CT, and our results are consistent with that study.
1 In that study, low tidal volume ventilation included a tidal volume of 6 mL/kg without PEEP. It reported no differences in atelectasis based on the tidal volume, indicating that low tidal volume ventilation does not cause further atelectasis compared to high tidal volume ventilation. However, the examination was limited to only 1 cm above the top of the right diaphragm, not the whole lung.
Ventilation with low tidal volume is usually accompanied with the use of PEEP and/or RMs to decrease atelectrauma.
5 Our assessment results for the whole lung indicate that PV strategies commonly used by anesthesiologists (low tidal volume with 5 cmH
2O PEEP, without RMs),
171819 do not cause more atelectasis in the immediate postoperative period compared to CV. A higher PaO
2/FiO
2 ratio was observed in the PV group during mechanical ventilation, which could not be explained based only on LUS scores. This discrepancy may have been due to the moderate correlation efficient between the change in LUS score and the change in PaO
2/FiO
2 ratio in these patients. A moderate correlation between them found in this study is comparable to previously reported results in patients without lung injury undergoing laparoscopic surgery.
14 The correlations in that previous study and our study including surgical patients without lung injury were weaker than those previously reported in ARDS patients.
20 In two studies on ARDS patients treated with high PEEP, a high level of PEEP displaced the alveolar interface filled with inflammatory materials or alveolar edema, leading to an increase in PEEP-induced lung recruitment volume, improvement of LUS score, and a consequent high correlation coefficient between LUS score and PaO
2 level.
2021 In contrast to ARDS patients, surgical patients without lung injury have normal (i.e., non-pathological) alveoli and usually experience minor atelectasis. Therefore, the effects of low PEEP could not be observed definitively by lung ultrasonography in these patients compared to patients in a more severe condition. In addition, as we did not use RMs, low PEEP was applied to prevent the occurrence of atelectasis rather than to reopen the collapsed alveoli. The higher PaO
2/FiO
2 ratio observed in the PV group may have been due to the increase in alveolar surfaces by extrinsic PEEP throughout the respiratory cycles, even though it was not clearly detected by lung ultrasonography. In this context, we postulated that this may have been why the LUS score in low tidal volume ventilation with 5 cmH
2O PEEP was comparable to that of CV but with a higher PaO
2/FiO
2 ratio.
In accordance with previous studies,
14 we found that the distribution of aeration loss was predominant and severe in dependent lung regions during anesthesia. Anesthesia-induced atelectasis is considered to be a result of alveolar collapse and appears in the dependent regions of lungs within 5 minutes of anesthesia induction.
22 GA causes relaxation and cephalad displacement of the diaphragm, which makes it less effective for maintaining distinct pressure within the intrathoracic and abdominal cavities, leading to the development of posterior paradiaphragmatic atelectasis.
1 According to the method described by Acosta et al.,
11 we used additional oblique scans along the intercostal space, in particular for the posterobasal region of the lung, because the classic lung sonographic approach may undervisualize the region hidden in the acoustic shadows of the ribs. Nonetheless, some dorsal parts of the lung where atelectasis most frequently occurs in anesthetized patients are necessarily blinded when the patient is in the supine position. Scanning paravertebral regions using small probes by turning the patient to the lateral position was recommended for a more precise examination of these regions.
23 However, we did not scan in the lateral position because of safety concerns associated with changing the position of paralyzed patients as well as limitations associated with the scapula that remains even after the change in position. This may have led to underestimation of the presence of atelectasis in the present study. No patients exhibited severe loss of aeration corresponding to a LUS score of 3 points in any region, consistent with previous reports. The LUS pattern of anesthesia-induced atelectasis typically includes small juxtapleural consolidation and air bronchograms as short bright echogenic structures.
11
The overall LUS score was 6.14 ± 4.10 points at the end of surgery. This is lower than the scores reported by Monastesse et al.
14 using the same scoring system, which were approximately 9 points 5 minutes after insufflation of the pneumoperitoneum and 10 points in the recovery room. This finding may be explained by differences in either surgery type or ventilation method between the two studies. First, Monastesse et al.
14 included patients undergoing laparoscopic surgery, in which pneumoperitoneum causes more cephalad displacement of the diaphragm, which results in decreased compliance and compressive atelectasis. Second, in their study, ventilation consisted of a tidal volume of 8 mL/kg PBW and no PEEP via volume-controlled ventilation (VCV). Low tidal volume ventilation combined with low or no PEEP could increase the incidence and amount of atelectasis.
57 Another possible reason is that we used PCV-VG given its reported advantages, including lower peak inspiratory pressure, lower driving pressure, and greater dynamic compliance when delivering the same amount of tidal volume.
24 In previous research on LUS scores based on ventilation mode in elderly patients, a PCV-VG group had lower LUS scores compared to a VCV group, which suggests that the distribution of ventilation and LUS score may vary depending on the ventilation mode.
25
The PV used in the present study consisted of a tidal volume of 6–8 mL/kg PBW and PEEP 5 cmH
2O PEEP without RMs. In a previous review article, mechanical ventilation using low tidal volumes (6–8 mL/kg PBW) and low PEEP (≤ 2 cmH
2O) without RMs was proposed for nonobese patients without lung injury undergoing open abdominal surgery, and the concept of intraoperative permissive atelectasis was introduced.
5 Various degrees of PEEP have been suggested to reduce PPCs, with recommendations ranging from 2 to 6 cmH
2O. A multicenter randomized controlled trial noted that intraoperative PV should include a low tidal volume and low PEEP without RMs.
26 On the other hand, a large retrospective study that investigated the association between intraoperative mechanical ventilator settings and outcomes showed that the use of minimal PEEP (2.2–5 cmH
2O) combined with low tidal volumes was associated with increased risk for 30-day mortality.
9 PEEP requirements vary widely among patients receiving PV during abdominal surgery. A previous study that explored the level of electrical impedance tomography-guided PEEP that minimizes lung collapse and hyperdistention showed that individualized PEEP reduced postoperative atelectasis and improved intraoperative oxygenation.
27 In fact, low tidal volumes and driving pressure,
28 rather than PEEP combined with lung RMs, are known to be responsible for lung protection in the intraoperative period.
7 In this study, we assessed loss of lung aeration during the perioperative period and examined whether a commonly used PV strategy using low tidal volume is associated with more atelectasis compared to CV.
171819 Although basing the level of PEEP on patient characteristics is the ideal approach, identifying the optimal level of PEEP was beyond the scope of the present study. Given our results showing no further atelectasis in low tidal volume ventilation and those of a previous study demonstrating interpatient variability in the amount of atelectasis induced by GA,
2 bedside ultrasonography may be a useful tool for monitoring perioperative anesthesia-induced atelectasis for individual patients who are ventilated with low tidal volume.
The present study had several limitations. First, our study population included both upper and lower abdominal surgery patients in the fields of urology and general surgery, as open abdominal surgery was limited to only a few types of surgery that did not involve laparoscopy or robots in our institution. However, the types of surgery were evenly distributed between the groups. Second, we did not use zero PEEP for the PV group based on the suggestion that PEEP compensates for anesthesia-induced reduction in functional residual capacity
5 and that intraoperative low tidal volume ventilation is beneficial only when used with PEEP.
9 Future studies including low tidal volume ventilation with zero PEEP may reach different conclusions. Third, our results should be interpreted in the setting used in this study, and have limited generalizability to other types of surgery, surgical position, and various combinations of tidal volume and PEEP and/or RMs. Our results could form a basis for future studies in perioperative ventilation. Fourth, FiO
2 delivered through masks may vary among patients. When FiO
2 was considered to be 50% in all patients, PaO
2/FiO
2 was similar between the groups in the recovery room (data not shown). Finally, we focused on aeration loss scores and did not assess lung overinflation. Although PEEP-induced hyperinflation was not expected to be prevalent in our patients because we did not use an excessively high tidal volume and/or high PEEP, lung ultrasonography has limited capability to detect lung hyperinflation.
20 In conclusion, low tidal volume ventilation combined with 5 cmH
2O PEEP did not cause further loss of aeration compared to high tidal volume ventilation in patients undergoing open abdominal surgery. Low tidal volume ventilation can be used for patients without lung injury based on bedside lung ultrasonography.
Go to :





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download