INTRODUCTION
The urinary system discharges waste products from the body in the form of urine through the kidney, ureter, bladder, and urethra. Transurethral surgery using the opposite route of the urine drainage is a specialized area of urology and a typical minimal invasive surgery using natural orifice. Transurethral surgery can be categorized into four types depending on the type of target organ: transurethral ureteral surgery, transurethral bladder surgery, transurethral prostate surgery, and transurethral urethral surgery. Transurethral surgery has been steadily changing with the advance of technology and instruments. In particular, advances in optical technology and working elements have provided better feasibility to the operator. In the studies using big data in the United States and Australia, changes in transurethral surgery for prostatic hyperplasia have been observed.
12 We recently reported a rapid change in the recent 8 years of ureteroscopic surgery for symptomatic urolithiasis.
3 Transurethral surgery is a popular surgical method for urologists, and it is easily performed in hospital and clinic.
4 However, most recent reports of changes in the transurethral surgery have been limited to the prostate surgery. There is a lack of reports on transurethral surgery by other surgical sites. At the urological outpatient site, various tests and procedures are performed for the diagnosis and treatment for patients. Demographic change and advances in technology and equipment also affect urological outpatient examinations and procedures. Cystoscopy and uroflowmetry are important examination tools in urological outpatient clinics. However, there are few population-based studies that accurately assess the trend of the frequency of diagnostic tests and procedures applied directly to urologic outpatients. We examined the recent epidemiologic trends in transurethral surgeries and urological outpatient procedures from 2009 to 2016 in Korea using the entire population-based cohort.
Go to :

DISCUSSION
In Korea, 23.2% of male adults over 50 years suffered from moderate to severe lower urinary symptoms, with the incidence increasing with age.
6 Urinary incontinence is common in the elderly and increases with age. The prevalence of urinary incontinence in medical welfare facilities in Korea was about 65.3%.
7 With the increase in the elderly population and the prevalence of LUTS, the demand for diagnostic tools has increased and treatment options are also changing. In addition, medical costs associated with the diagnosis and treatment of urologic diseases continue to increase with the aging of the global population.
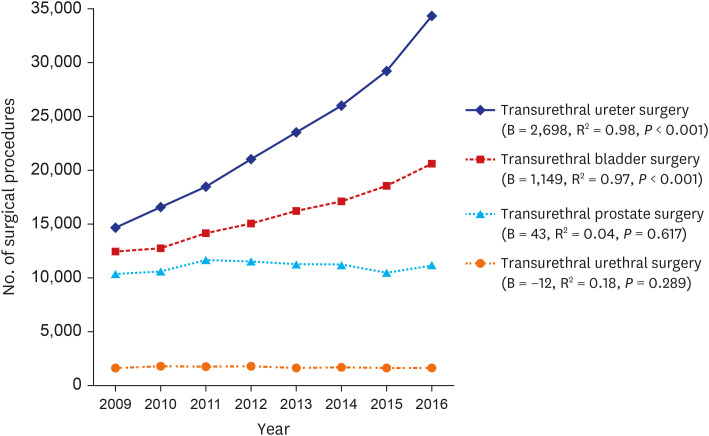
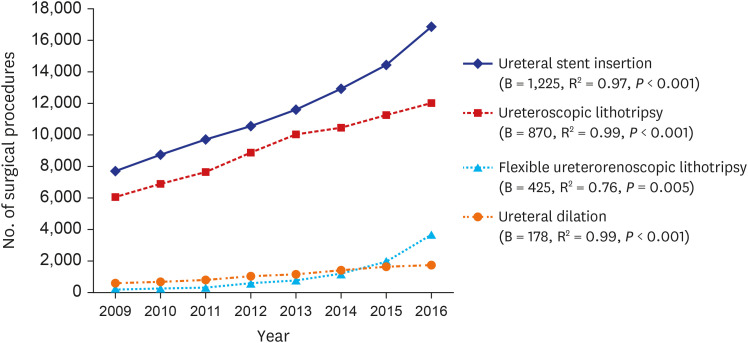
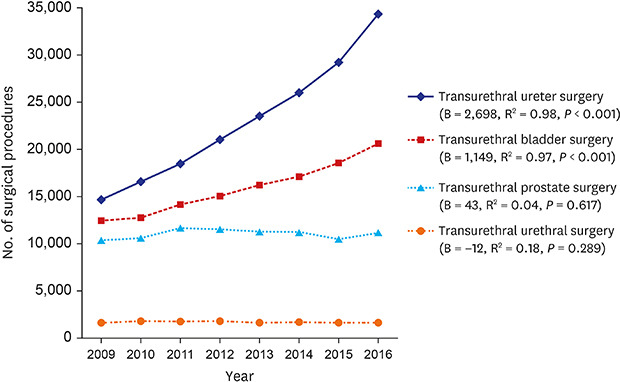
8 In this study, we analyzed recent changes over the last 8 years in diagnostic tools and treatment options in patients who underwent urologic diseases. Transurethral endoscopic surgery is a relatively less invasive surgical procedure that can be performed on the urinary tract. In this study, we confirmed that transurethral ureter surgery and transurethral bladder surgery were significantly increased. Ureteroscopic lithotripsy and flexible ureterorenoscopic lithotripsy showed a significant increase during the 8-year period. In particular, flexible ureterorenoscopic lithotripsy has increased rapidly in recent years thanks to improvements in endoscopic performance and advance of therapeutic materials such as access sheath. Extracorporeal shockwave lithotripsy (ESWL) is the most preferred treatment by urologists for urolithiasis. In the previous study, the use of ESWL for treating urolithiasis increased by 16% from 89,553 in 2009 to 104,013 in 2016 (B = 2,284; R
2 = 0.684;
P = 0.011).
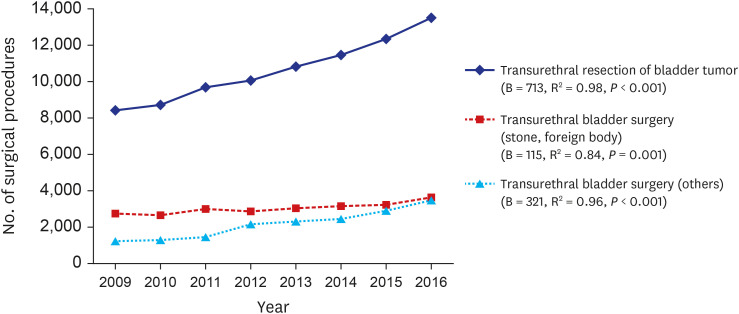
3 In recent, many urologists have chosen flexible ureterorenoscopic surgery to completely remove complex renal stones, and actively switching to ureteroscopic surgery for stones with delayed discharge even after ESWL. This is presumed to be because most urologists claim ureteral stent insertion when switching to ureteroscopic surgery due to delayed discharge of stones and severe pain after ESWL. In the United States, incidence rates of bladder cancer increased by 0.16% per year for the last four decades and incidence-based mortality decreased since 2000.
9 In particular, the age-adjusted incidence rate and 5-year survival rates for a localized stage of bladder cancer increased from 1973 to 2009.
10 In Korea, the number of bladder cancer cases increased from 2,180 cases in 1999 to 3,549 cases in 2011.
11 The increment of bladder cancer incidence rate might contribute to the increase in TUR-BT. Moreover, as our study shows, the increment of cystoscopy seems to help with early detection of initial and recurrent bladder cancer. These could contribute to the steady increase of TUR-BT. Patients with prostatic hyperplasia usually start with medical treatment and optionally undergo surgical treatment.
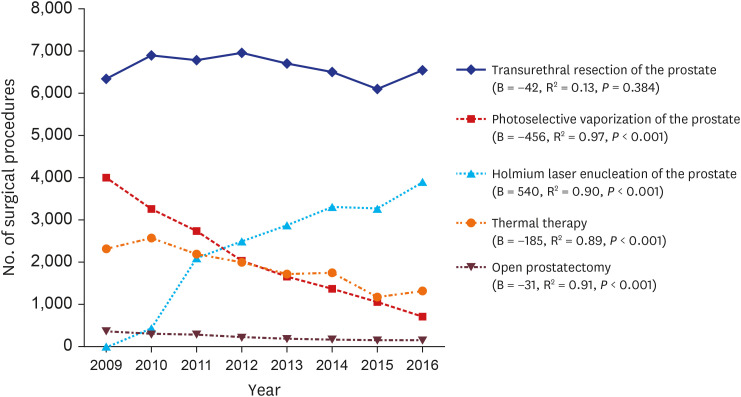
5 In this study, there were not significant changes in transurethral prostate surgery over the 8-years period. Conventional TUR-P is still recognized as a gold standard surgical treatment in prostatic hyperplasia, and it is steadily implemented because most medical institutions have basic TUR equipment. HoLEP has more benefits such as the increased amount of tissue removal, shorter catheterization time, shorter hospital length of stay, and lower transfusion rates than other transurethral prostate surgeries.
412 Recently, HoLEP showed comparable or superior surgical outcomes than TUR-P, and many urologists prefer HoLEP due to fewer postoperative complications.
4 Our data show that HoLEP is rapidly replacing PVP.
With the increase in the elderly population, uroflowmetry, which is used for diagnosis and monitoring of voiding diseases, continues to increase. Uroflowmetry is easy to perform and can be analyzed quickly, and its installation costs are relatively low, making it widely used in the outpatient field. Also, cystoscopy is an effective diagnostic tool that can be easily performed in the outpatient field and is widely used in the diagnosis of hematuria, bladder tumors, and persistent voiding disorders.
13 In our study, it was confirmed that uroflowmetry and cystoscopy increased continuously during the investigation period, but prostate massage continues to decline significantly. Prostate massage is an outpatient procedure used to diagnose and treat chronic prostatitis. The previous survey reported that many urologists do not routinely subject their patients to the diagnostic procedures required to differentiate among the various manifestations of chronic prostatitis syndrome.
14 In Korea, less than half of urologists employ culture tests in the diagnosis of chronic prostatitis, and most urologists prescribe antibiotic treatment as a treatment of chronic prostatitis according to personal beliefs and professional characteristics of individual physicians.
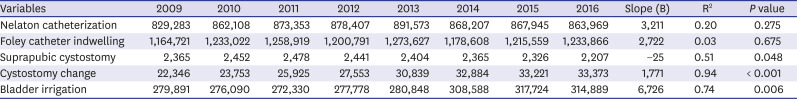
15 Prostate massage, which has been widely practiced in the past, seems to decrease continuously due to clinician preference for diagnosis and treatment. Nelaton catheterization, Foley catheter indwelling, and suprapubic cystostomy have been maintained steadily during the investigation period, and cystostomy change and bladder irrigation have been cumulative and increased during the investigation period.
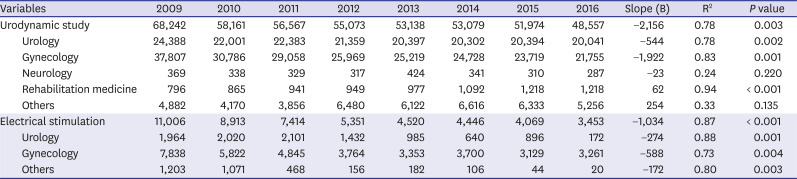
A study of UDS patterns in the United States from 2002 to 2007 showed that stress incontinence was the most common clinical condition, urologists performed 59.8%, and gynecologists performed 35.5%.
16 In Korea, UDS is obligatory before anti-incontinence surgery. Anti-incontinence surgery in Korea was significantly reduced to 60,520 cases in 2006 and 24,599 cases in 2015.
17 In this study, UDS has been continuously decreasing during the investigation period. The reduction in gynecology was found to be greater than that of urology. Our results showed a steady decline in EST during the study period. Previous studies revealed a large variation in the effect of EST for urinary incontinence and discontinuation rate is relatively high.
181920
It will remain unchanged that ESWL is the first treatment option in urolithiasis treatment. However, for rapid relief of stone pain and complete elimination of complex stones, transurethral ureter surgery is expected to continue to increase and develop. Also, with an increase in the elderly population, transurethral prostate surgery and urological outpatient procedures are presumed to continue to increase.
There are some limitations to this study. First, it was a population-based analysis using an established cohort of NHIS based on medical insurance claims data. Thus, it has limitations in reflecting the actual situation in the field. Second, we could not adjust the number of performing tests and treatments per year by age. Our HIRA data lacks some important clinical data and individualized data. Despite these limitations, we believe that providing the actual number of claims provided by the health care provider has helped to identify the current trends in common urologic diagnostic tools and transurethral surgeries.
In conclusion, transurethral ureter surgery and transurethral bladder surgery have been continuously increasing in Korea. Transurethral prostate surgery and transurethral urethral surgery remained constant with no increase or decrease. Cystoscopy and uroflowmetry continue to increase, while UDS and EST continue to decrease.
Go to :






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download