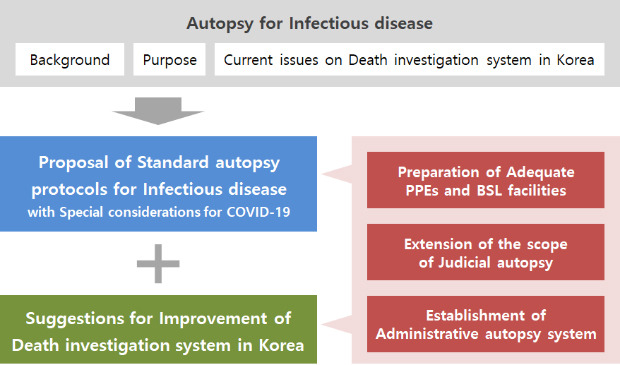
I. INTRODUCTION
II. OVERVIEW OF INFECTIOUS DISEASE AND ITS AUTOPSY
1. Background
1) General classification
2) Diagnostic clues during the autopsy
3) Regulations associated with the infectious diseases in Korea
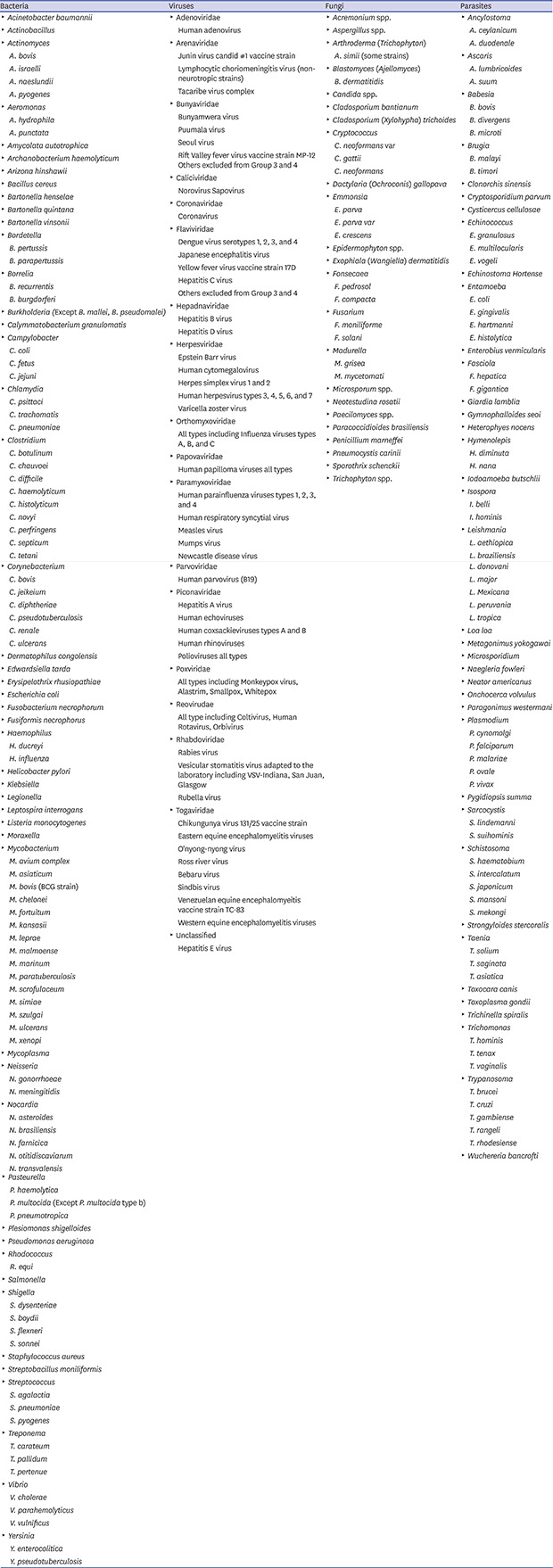
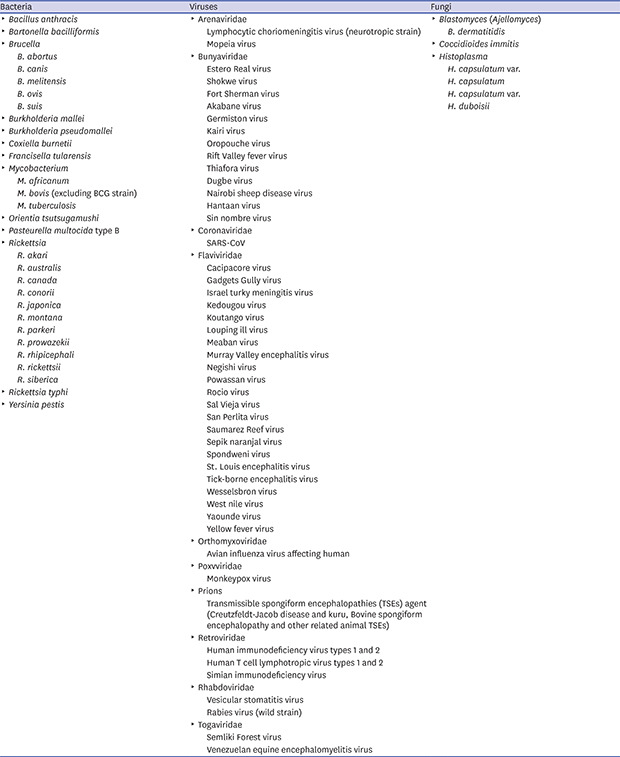
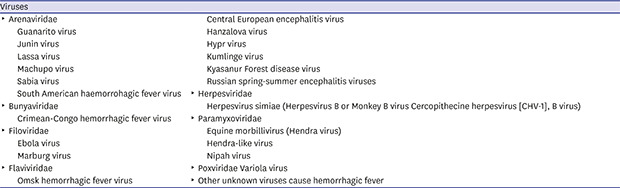
4) Risk group classification of the infectious agents
5) Biosafety level required for handling high-risk agents
• Grade 1: facilities that handle high-risk pathogens that are unlikely to cause diseases to healthy adults.
• Grade 2: facilities that handle high-risk pathogens that can cause human diseases unlikely to be a serious hazard and for which effective treatment and preventive measures are available.
• Grade 3: facilities that handle high-risk pathogens that usually cause serious human diseases and for which effective treatment and preventive measures are available.
• Grade 4: facilities that handle high-risk pathogens that usually cause serious human diseases and for which effective treatment and preventive measures are not usually available.
2. The purpose of the autopsy for infectious diseases
1) Identification of the causal relationship between death and infectious diseases
2) Provide medical and epidemiological information through a final diagnosis based on pathology
3) Provide grounds for judgment on potential legal disputes
3. Current issues regarding the autopsy for infectious diseases in Korea
1) Lack of medical history of the deceased
2) A criminal justice-oriented death investigation system
3) Regional and institutional deviation of autopsy facilities and equipment
4) Insufficient health support for autopsy personnel
5) Lack of safety considerations for other facilities and workers related to the autopsy
III. STANDARD AUTOPSY PROTOCOLS FOR INFECTIOUS DISEASES
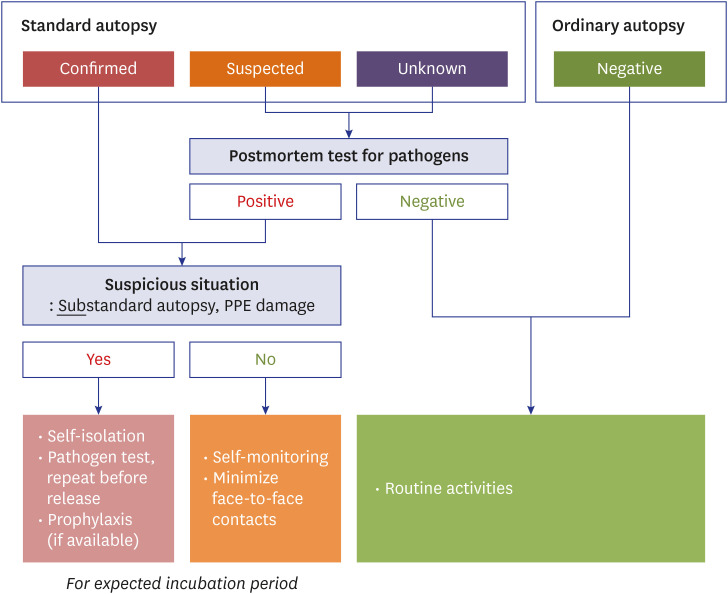
1. Target subjects and principles
1) General principles
2) Risk classification
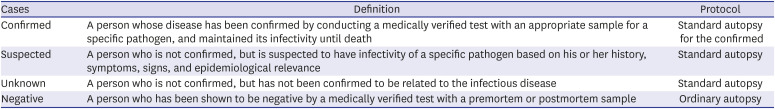
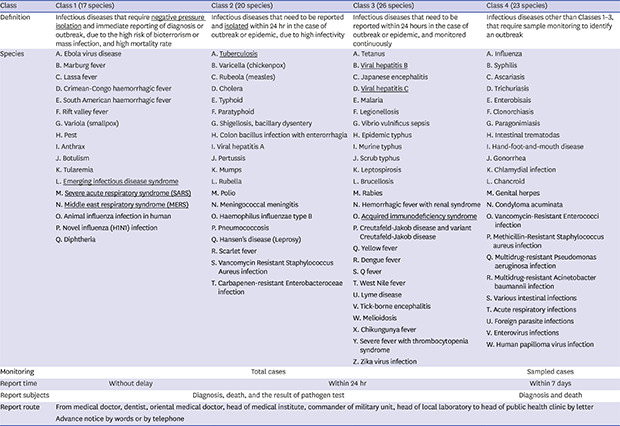
Table 1
Case classification and their definitions
2. Preparations before autopsy
1) Consideration of preliminary test
2) Storage and transfer of the body
2. Management of the facilities and working environment
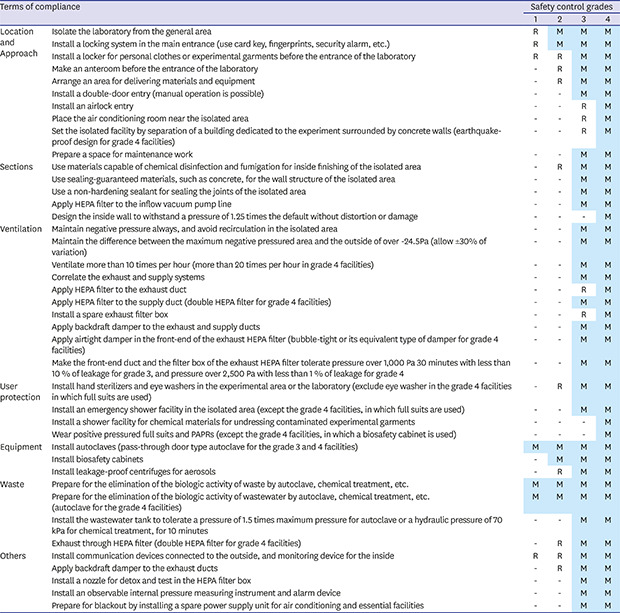
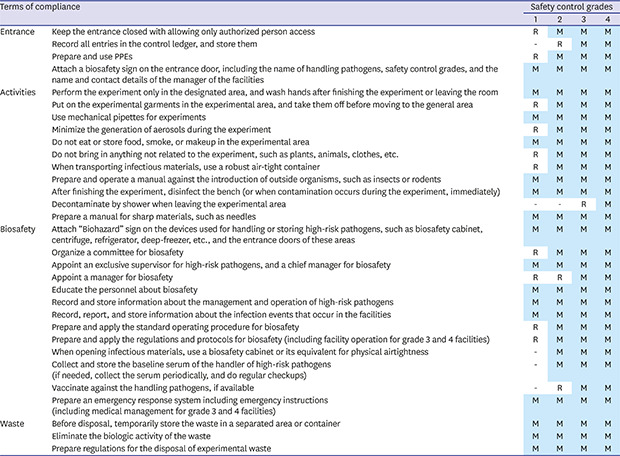
1) Facility standards
2) Waste disposal
3) Disinfection
4) Laundry
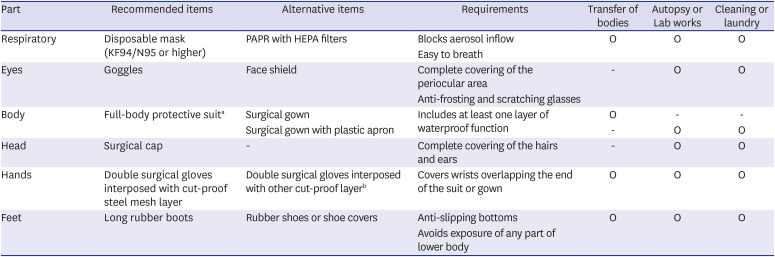
3. PPEs
1) General principles
2) Selection of PPEs
Table 2
Recommended components of PPEs, and their alternatives




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download