INTRODUCTION
Positional plagiocephaly is a deformation of the shape of the head due to external forces, and is not related to premature synostotic fusion of cranial sutures. Its incidence is estimated at 46.6%, making it the most common positional head shape abnormality among infants.
1 Moderate to severe cases that are left untreated predispose infants to the risk of cosmetic, and more importantly, psychomotor and cognitive problems.
2
Helmet therapy is a commonly prescribed treatment strategy for positional plagiocephaly and is regarded as a low-risk intervention. The primary consideration regarding the use of helmet therapy is its cost. Additionally, a recent review of helmet therapy found that it is associated with mild complications that can be resolved by discontinuing the treatment. The morbidity is usually due to mild skin irritation, which emphasises the need to maintain good hygiene.
3
The benefits of helmet therapy strongly correlate with age. Prior studies have advocated helmet therapy at a younger age to obtain maximum benefits.
4567 Likewise, several authors believe that the cut-off point where helmet therapy ceases to be beneficial could be as early as 8–12 months.
567 Recent reports have indicated that the age at treatment initiation and the severity of the asymmetry are the main factors that affect the effectiveness of treatment.
8 Although physicians consider these factors as important, early-stage positional plagiocephaly can easily be considered as normal; thus, the patient's first clinic visit for diagnosis can be delayed. Moreover, in Korea, we have frequently encountered patients with deformational plagiocephaly who are more than 6 months old. At this point, the appropriate treatment with or without a helmet must be decided. No consensus has been reached regarding the effective period range of helmet therapy for positional plagiocephaly.
In the present study, we clarified whether delayed initiation of helmet therapy is still effective, and investigated the factors affecting the effective application of helmet therapy for late-diagnosed plagiocephaly. If we extend the applicative period of effective helmet therapy, the results of this study can be implemented in daily practice as a practical guideline for treating patients with late-diagnosed positional plagiocephaly.
Go to :

RESULTS
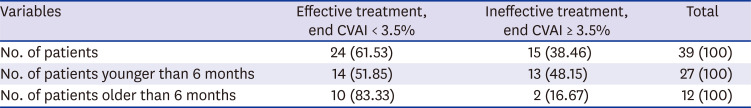
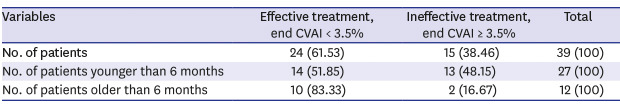
Thirty-nine patients with positional plagiocephaly were evaluated in this study. In accordance with our helmet therapy protocol, the therapy was considered successful in 24 patients (74.36%) with CVAI values of ≤ 3.5%. Twenty-seven patients were aged < 6 months, of whom 14 attained successful treatment results. However, 12 patients were aged > 6 months, of whom 10 attained effective treatment outcomes (
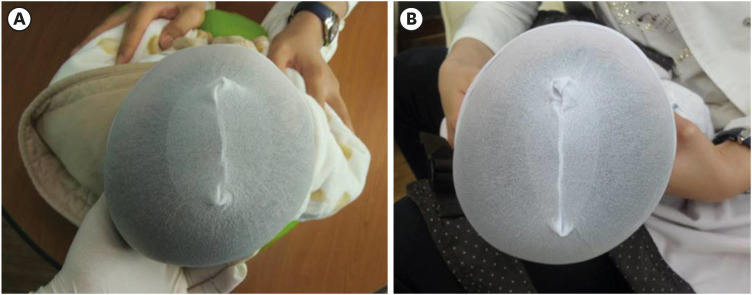
Table 1). A representative case is shown in
Fig. 2.
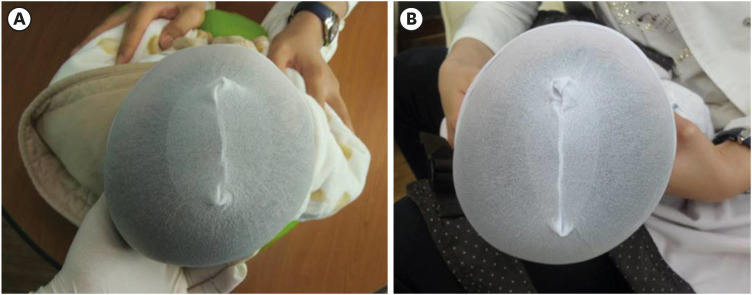 | Fig. 2
Representative case of a patient aged 8 months, for the reception of helmet therapy. Eight months could be considered late to start helmet therapy; however, his initial absolute diagonal distance difference was 15 mm and initial CVAI was 82.1. According to the regular treatment protocol, after 6 months of treatment, we could obtain a CVAI change of 4.06%. Proper indications for the helmet treatment can be effectively applied for patients with late-visited positional plagiocephaly. (A) Pre-treatment. (B) Six months post-treatment.
CVAI = cranial vault asymmetry index.

|
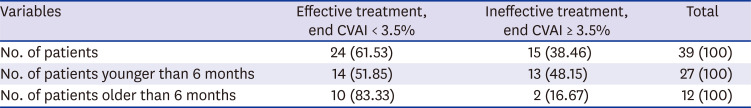
Table 1
Patient composition of the study group and their helmet treatment outcome
|
Variables |
Effective treatment, end CVAI < 3.5% |
Ineffective treatment, end CVAI ≥ 3.5% |
Total |
|
No. of patients |
24 (61.53) |
15 (38.46) |
39 (100) |
|
No. of patients younger than 6 months |
14 (51.85) |
13 (48.15) |
27 (100) |
|
No. of patients older than 6 months |
10 (83.33) |
2 (16.67) |
12 (100) |

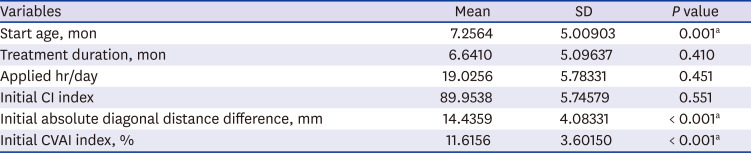
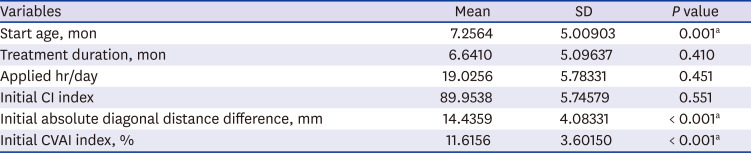
The mean ages of the patients at treatment initiation and duration of the treatment were 7.26 months (range, 3–24 months) and 6.64 months (range, 3–32 months), respectively. The mean duration of daily helmet use was 19.03 hours/day (range, 10–22 hours/day). The mean initial CI was 89.95% (range, 76.9%–100%). The mean initial absolute diagonal distance difference was 14.44 mm (range, 10–24 mm), and the mean initial CVAI was 11.62% (range, 6.30%–20.00%). The mean final CVAI value was 3.59% (range, 0.6%–7.69%). The mean difference in the CVAI was 8.02% ± 4.38%. In the multiple logistic regression analysis, we identified three variables that affected the change in CVAI (%), namely age at treatment initiation (
P = 0.001), initial absolute diagonal distance difference (
P < 0.001), and initial CVAI (
P < 0.001) (
Table 2).
Table 2
Multiple logistic regression test for effective change in CVAI (%)
|
Variables |
Mean |
SD |
P value |
|
Start age, mon |
7.2564 |
5.00903 |
0.001a
|
|
Treatment duration, mon |
6.6410 |
5.09637 |
0.410 |
|
Applied hr/day |
19.0256 |
5.78331 |
0.451 |
|
Initial CI index |
89.9538 |
5.74579 |
0.551 |
|
Initial absolute diagonal distance difference, mm |
14.4359 |
4.08331 |
< 0.001a
|
|
Initial CVAI index, % |
11.6156 |
3.60150 |
< 0.001a
|

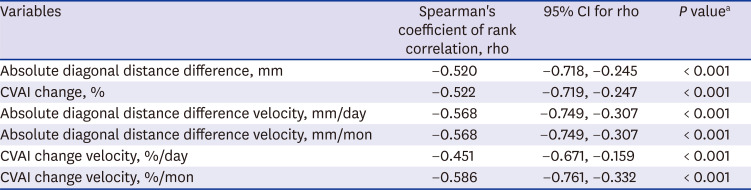
The Spearman rank correlation test for possible factors related to age at initiation of helmet therapy revealed that the following six parameters showed statistically significant negative correlations: absolute diagonal distance difference (mm;
P < 0.001), CVAI change (%;
P < 0.001), absolute diagonal distance difference change velocity (mm/day;
P < 0.001), absolute diagonal distance difference velocity (mm/month;
P < 0.001), CVAI change velocity in terms of days (%/day;
P < 0.001), and CVAI change velocity in terms of months (%/month;
P < 0.001) (
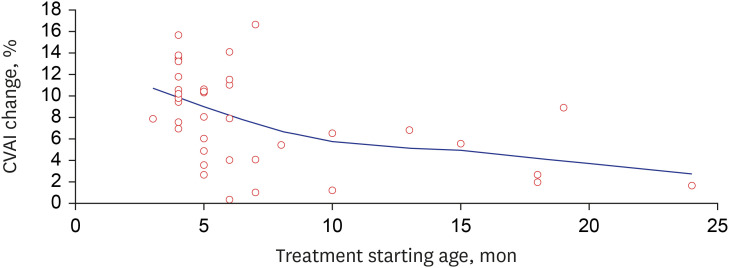
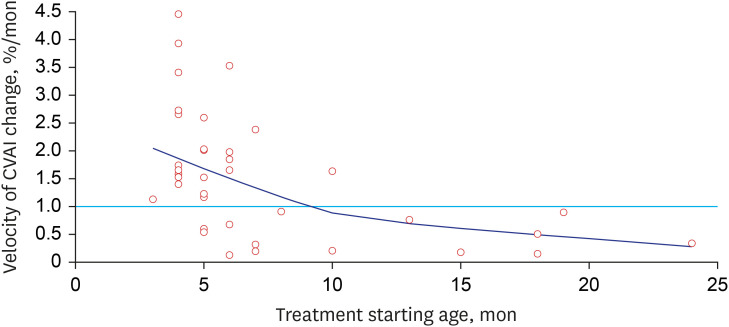
Table 3). However, CVAI correction was still attained in patients who started helmet therapy at a later age (
Fig. 3). Regarding CVAI change velocity, patients who started treatment at the age of 6 months showed no peak velocity and a gradual decrease in the velocity. When helmet use has a positive effect, a gradual change in CVAI of at least 1% should be apparent. Lower values are considered to have a minimal effect on treatment. Up to 9 months, as demonstrated by the velocity, the time at which a change of > 1%/month is achieved could be an effective period (
Fig. 4).
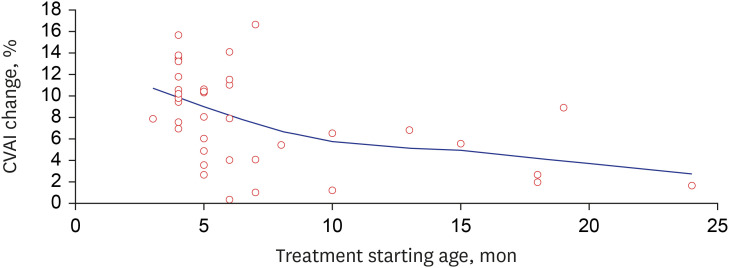 | Fig. 3
Relationship between CVAI (%) change and starting age of helmet treatment (month). This shows that patients older than 6 months can still have CVAI change (%).
CVAI = cranial vault asymmetry index.

|
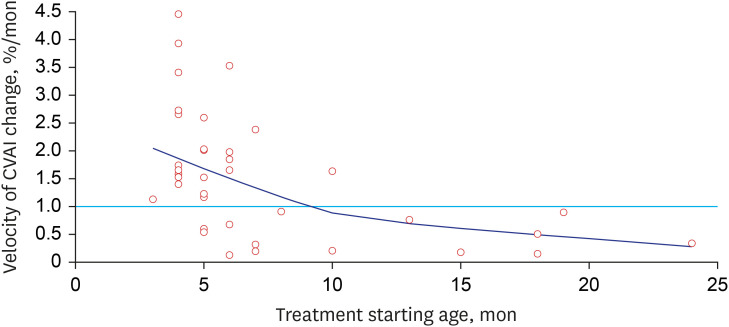 | Fig. 4
Relationship between CVAI change velocity (%/month) and starting age of helmet treatment (month). This shows that between 5 and 10 months, a CVAI change/month greater than 1% could be considered effective.
CVAI = cranial vault asymmetry index.

|
Table 3
Correlation between variables of effective helmet therapy and starting age (month), by the Spearman rank correlation test
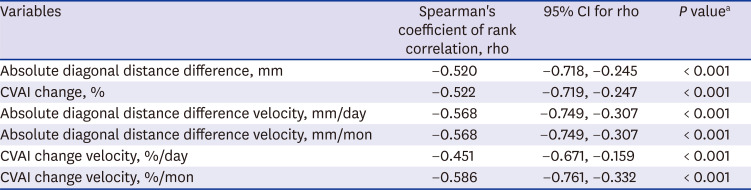
|
Variables |
Spearman's coefficient of rank correlation, rho |
95% CI for rho |
P valuea
|
|
Absolute diagonal distance difference, mm |
−0.520 |
−0.718, −0.245 |
< 0.001 |
|
CVAI change, % |
−0.522 |
−0.719, −0.247 |
< 0.001 |
|
Absolute diagonal distance difference velocity, mm/day |
−0.568 |
−0.749, −0.307 |
< 0.001 |
|
Absolute diagonal distance difference velocity, mm/mon |
−0.568 |
−0.749, −0.307 |
< 0.001 |
|
CVAI change velocity, %/day |
−0.451 |
−0.671, −0.159 |
< 0.001 |
|
CVAI change velocity, %/mon |
−0.586 |
−0.761, −0.332 |
< 0.001 |

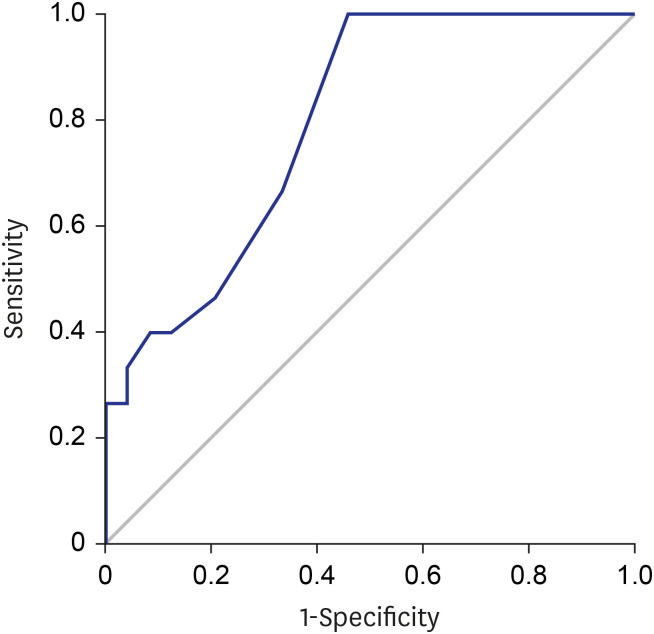
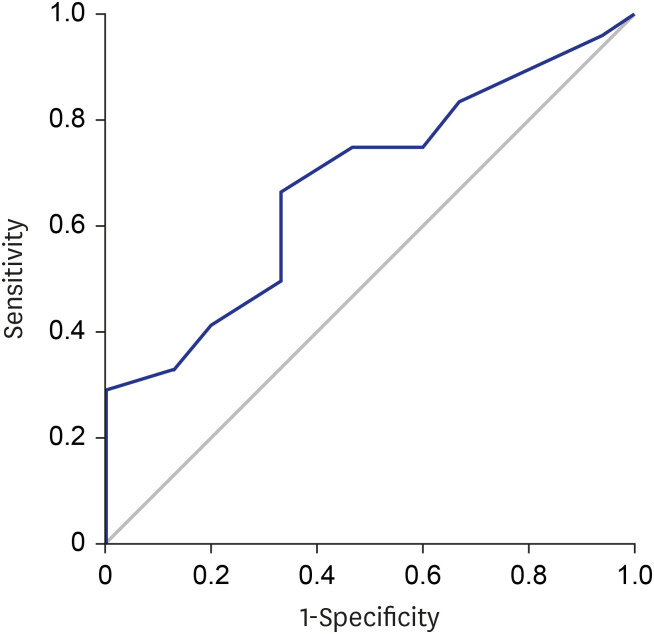
To investigate the optimal age range when a child should commence helmet therapy for effective treatment, we performed ROC curve analysis of the age at treatment initiation with a 95% confidence interval (CI). We found that the cut-off age for effective treatment was 5.5 months, with 66.7% sensitivity and 66.7% specificity (AUC-ROC, 0.796; 95% CI, 0.156–0.497;
P < 0.001) (
Fig. 5). The cut-off initial absolute diagonal distance difference for effective treatment was 13.50 mm, with 66.7% sensitivity and 66.7% specificity (AUC-ROC, 0.679; 95% CI, 0.510–0.848;
P < 0.001) (
Fig. 6). The cut-off initial CVAI for effective treatment was 11.03%, with 66.7% sensitivity and 66.7% specificity (AUC-ROC, 0.674; 95% CI, 0.503–0.844;
P < 0.001) (
Fig. 7).
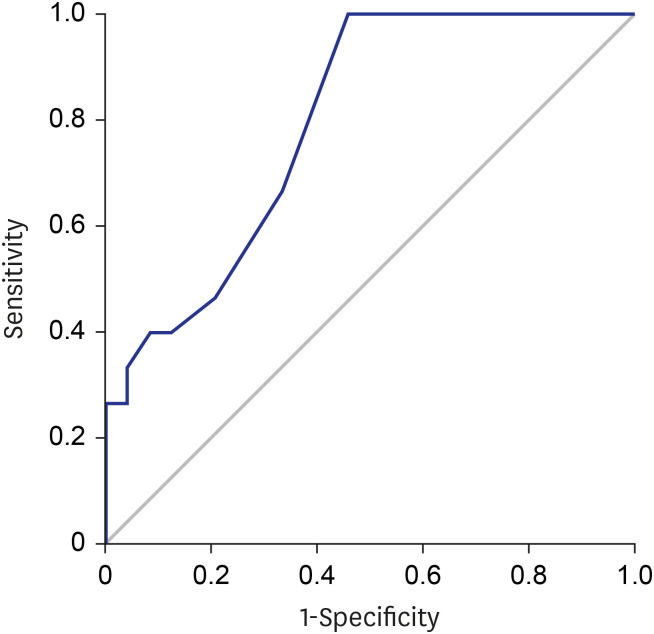 | Fig. 5
Relationship between age at treatment initiation and treatment effectiveness. ROC defining the sensitivity and specificity of age at treatment initiation for effective helmet treatment in patients with positional plagiocephaly (ROC area, 0.796; 95% confidence interval, 0.156–0.497; P < 0.001).
ROC = receiver-operating curve.

|
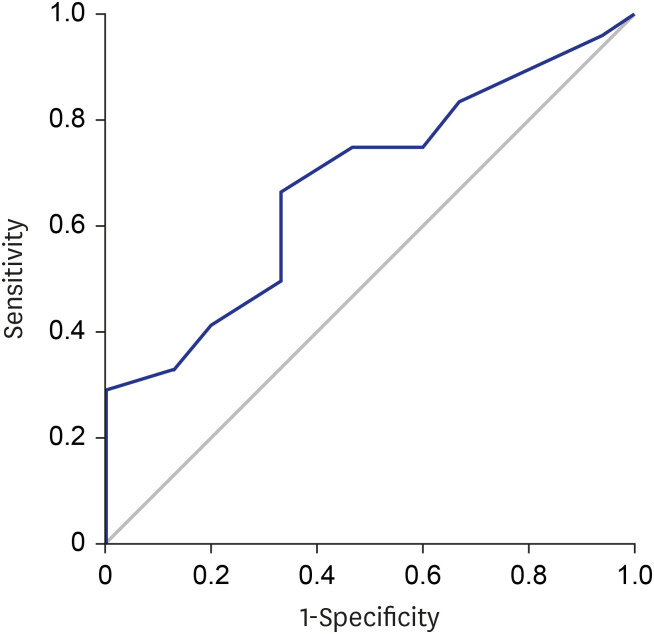 | Fig. 6
Relationship between initial absolute diagonal distance differences and treatment effectiveness. ROC defining the sensitivity and specificity of initial absolute diagonal distance differences for effective helmet treatment in patients with positional plagiocephaly (ROC area, 0.679; 95% confidence interval, 0.510–0.848; P < 0.001).
ROC = receiver-operating curve.

|
 | Fig. 7
Relationship between initial CVAI and treatment effectiveness. ROC defining the sensitivity and specificity of initial CVAI for effective helmet treatment in patients with positional plagiocephaly (ROC area, 0.674; 95% confidence interval, 0.503–0.844; P < 0.001).
CVAI = cranial vault asymmetry index, ROC = receiver-operating curve.

|
Go to :

DISCUSSION
Despite the common understanding that early initiation of helmet therapy is better for treating positional plagiocephaly, in reality, many patients visit our clinic at a later age. Given the natural history of positional plagiocephaly, parents easily consider that natural skull remodelling can resolve positional plagiocephaly, which results in delayed clinic visit.
1314 Particularly, Korea has a large population with brachycephaly based on the standardized cephalic index, but reference values for Koreans have not been established yet. Owing to these characteristics, cases of delayed diagnosis are common in Korea. Previous studies have only investigated possible factors for attaining the maximum benefit from helmet therapy for positional plagiocephaly. The general consensus is that in patients aged 5–6 months, repositioning therapy is preferred over helmet therapy.
4 Several previous studies described the benefits of introducing helmet therapy at earlier ages (< 6 months), including higher correction rates and the resulting shorter treatment durations.
4715 Therefore, when encountering delayed-diagnosed patients because of the unavoidable characteristics of positional plagiocephaly, clinicians need clearer evidence to prescribe helmet therapy. In clinical practice, this need is increasing, and this study demonstrated the efficacy of helmet therapy even in older patients.
Regarding the treatment outcomes, we observed successful outcomes in 51.85% of the patients who received early treatment and in 83.33% of the patients who received late treatment (
Table 1). Many cases of successful outcomes of helmet therapy for patients aged < 6 months have been reported; however, the mean age of the cohorts in the previous studies was 19.9 weeks, and that in our study was 22.8 weeks. The patients who received early treatment in this study were relatively older than those in Western studies. Therefore, we believe that these differences may have contributed to the differences in treatment outcomes. Furthermore, owing to the small study population that received delayed treatment, we cannot conclude that late treatment has more benefits. In this study, we demonstrated that even patients who received late treatment had satisfactory treatment outcomes.
This study clearly reflects the Korean outpatient clinical setting with respect to positional plagiocephaly. This is because 12 of our 39 patients received treatment at an older age, of whom 83.33% showed effective treatment outcomes. Moreover, besides age at treatment initiation, various factors can affect the final CVAI change, such as initial absolute diagonal distance difference and initial CVAI. Therefore, these two factors can be considered concurrently when deciding whether to prescribe helmet therapy for late-visiting patients. Although the CVAI correction rate plummeted until no further effect could be observed after the age of 15 months, we still found moderate to minimal changes in CVAI range from 5 to 10 months. The decrease in the curve was not sharp but gradual. This is in accordance with the findings of Seruya et al.,
15 who described that the declining rate of correction reflects a logarithmic decline in head circumference growth. Nonetheless, head growth may actually reach its limit at the age of 6 years, i.e., improvement can still be observed up to that age. Another study with the same objective showed that the rate of improvement was the same between older (> 12 months) and younger patients (< 3 months).
6
In this study, complication rates were not compared between early- and late-onset helmet therapy. As we included only patients who followed the proper helmet therapy protocol, our patient cohort was small and the follow-up period was short. These are the limitations of our study. Even though we demonstrated that starting helmet therapy at later ages is possible, the slow improvement rate can increase the risk of complications such as dermatitis, which potentially outweighs the benefits. However, we did not observe any notable complications such as pressure sores, skin infections, or subcutaneous abscesses. Thus, we expect that our findings support the benefits of helmet therapy more than its risk of complications. More studies on the potential complications of helmet therapy are warranted. At this point, we emphasise that diagnosis at a later age is not a valid reason to refuse the commencement of helmet therapy. The effectiveness of helmet therapy depends not only on the age at treatment initiation but also on the initial absolute diagonal distance difference and CVAI index. Once patients are diagnosed with positional plagiocephaly, an initial absolute diagonal distance difference of > 13.50 mm and an initial CVAI index of > 11.03% can predict the effectiveness of the treatment, given that the proper treatment protocol is applied, regardless of late onset of treatment. One similarity concerning the optimal age among the different findings is that several factors influence the relationship between optimal age and plagiocephaly correction rate, such as severity of the deformity and parent compliance.
6 Several other authors asserted that the cut-off point at which helmet therapy ceases to be beneficial could be as early as 8–12 months.
67
Implementing the concept of a long effective period in plagiocephaly management will help healthcare providers educate parents. One study reported that helmet therapy confers a lot of stress on parents, who are the actual caregivers. A significant proportion of caregivers (31.9%) temporarily stop the therapy without consulting their physicians.
4 Establishment of an optimal treatment period would mean that parents should take full advantage of the period where maximum benefits can be received. Furthermore, understanding that the treatment can be effective even after 6 months of age can give parents psychological encouragement to endure the hardship from the treatment for a certain limited period.
We allowed parents to minimise the time of helmet use when the patient refuses the treatment, because we are more concerned about steady treatment. In the retrospective chart review, we had to exclude all these patients in accordance with the strictly accepted helmet therapy protocol; thus, the number of patients included in this study was small. Our future studies will focus on the differences between data of Korean patients with positional plagiocephaly and the standardized reference, as well as on the effect of the treatment protocol on a wider range of patients. One more limitation of our study was the shorter study period compared to those of other studies.
In conclusion, the effectiveness of helmet therapy is affected by age at treatment initiation, initial absolute diagonal distance difference, and initial CVAI. Age has been the only main consideration for indicating helmet therapy; however, late-diagnosed patients can attain effective treatment outcomes despite gradual decrease in the correction rate. We recommend that healthcare providers should not hesitate to introduce helmet therapy to patients who visit the clinic beyond the optimal effective period if they fulfil the treatment criteria.
Go to :







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download