1. Benson SC, Pershadsingh HA, Ho CI, Chittiboyina A, Desai P, Pravenec M, et al. Identification of telmisartan as a unique angiotensin II receptor antagonist with selective PPARgamma-modulating activity. Hypertension. 2004; 43(5):993–1002. PMID:
15007034.
2. Song KH, Park JH, Jo I, Park JY, Seo J, Kim SA, et al. Telmisartan attenuates hyperglycemia-exacerbated VCAM-1 expression and monocytes adhesion in TNFα-stimulated endothelial cells by inhibiting IKKβ expression. Vascul Pharmacol. 2016; 78:43–52. PMID:
26455386.

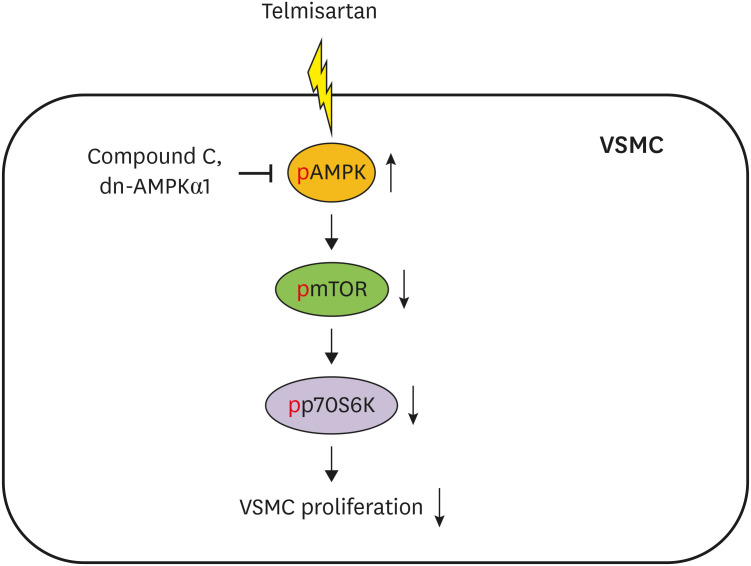
3. Hwang YJ, Cho DH. Activation of AMPK/proteasome/MLCK degradation signaling axis by telmisartan inhibits VSMC contractility and vessel contraction. Biochem Biophys Res Commun. 2020; 524(4):853–860. PMID:
32046856.

4. Lacolley P, Regnault V, Nicoletti A, Li Z, Michel JB. The vascular smooth muscle cell in arterial pathology: a cell that can take on multiple roles. Cardiovasc Res. 2012; 95(2):194–204. PMID:
22467316.

5. Rivard A, Andrés V. Vascular smooth muscle cell proliferation in the pathogenesis of atherosclerotic cardiovascular diseases. Histol Histopathol. 2000; 15(2):557–571. PMID:
10809377.
6. Yamamoto K, Ohishi M, Ho C, Kurtz TW, Rakugi H. Telmisartan-induced inhibition of vascular cell proliferation beyond angiotensin receptor blockade and peroxisome proliferator-activated receptor-gamma activation. Hypertension. 2009; 54(6):1353–1359. PMID:
19822796.
7. Destro M, Cagnoni F, Dognini GP, Galimberti V, Taietti C, Cavalleri C, et al. Telmisartan: just an antihypertensive agent? A literature review. Expert Opin Pharmacother. 2011; 12(17):2719–2735. PMID:
22077832.

8. Michel MC, Foster C, Brunner HR, Liu L. A systematic comparison of the properties of clinically used angiotensin II type 1 receptor antagonists. Pharmacol Rev. 2013; 65(2):809–848. PMID:
23487168.

9. Miura S, Karnik SS, Saku K. Review: angiotensin II type 1 receptor blockers: class effects versus molecular effects. J Renin Angiotensin Aldosterone Syst. 2011; 12(1):1–7. PMID:
20603272.

10. Papadopoulos N, Lennartsson J. The PDGF/PDGFR pathway as a drug target. Mol Aspects Med. 2018; 62:75–88. PMID:
29137923.

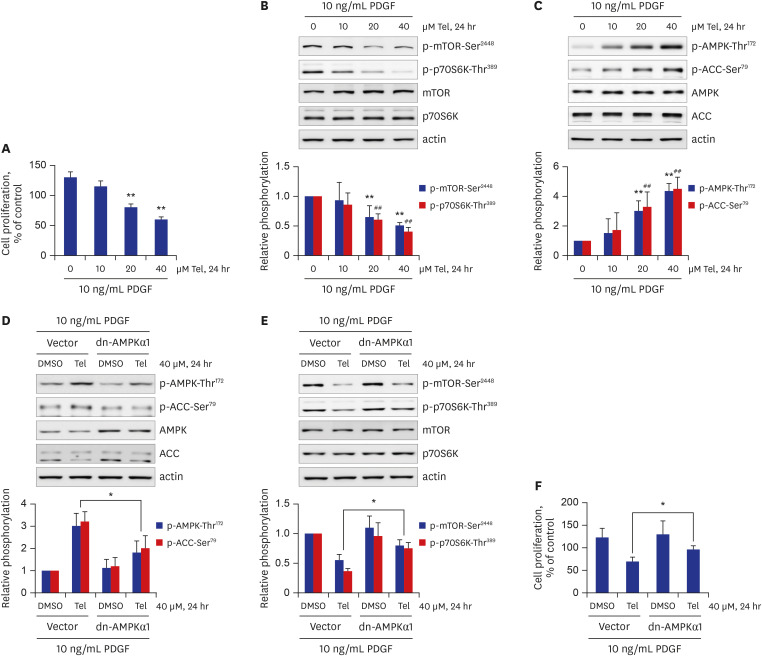
11. Shawky NM, Segar L. Sulforaphane inhibits platelet-derived growth factor-induced vascular smooth muscle cell proliferation by targeting mTOR/p70S6kinase signaling independent of Nrf2 activation. Pharmacol Res. 2017; 119:251–264. PMID:
28212891.

12. Dong X, Hu H, Fang Z, Cui J, Liu F. CTRP6 inhibits PDGF-BB-induced vascular smooth muscle cell proliferation and migration. Biomed Pharmacother. 2018; 103:844–850. PMID:
29710500.

13. Gomez D, Owens GK. Smooth muscle cell phenotypic switching in atherosclerosis. Cardiovasc Res. 2012; 95(2):156–164. PMID:
22406749.

14. Fuster V, Badimon L, Badimon JJ, Chesebro JH. The pathogenesis of coronary artery disease and the acute coronary syndromes (1). N Engl J Med. 1992; 326(4):242–250. PMID:
1727977.
15. Schwartz SM, deBlois D, O'Brien ER. The intima. Soil for atherosclerosis and restenosis. Circ Res. 1995; 77(3):445–465. PMID:
7641318.
16. Dzau VJ, Braun-Dullaeus RC, Sedding DG. Vascular proliferation and atherosclerosis: new perspectives and therapeutic strategies. Nat Med. 2002; 8(11):1249–1256. PMID:
12411952.

17. Hong MK. Restenosis following coronary angioplasty: current status. Korean J Intern Med (Korean Assoc Intern Med). 2001; 16(2):51–55.
18. Li Z, Li Y, Jia Y, Ding B, Yu J. Rab1A knockdown represses proliferation and promotes apoptosis in gastric cancer cells by inhibition of mTOR/p70S6K pathway. Arch Biochem Biophys. 2020; 685:108352. PMID:
32240637.

19. Li J, Liu W, Hao H, Wang Q, Xue L. Rapamycin enhanced the antitumor effects of doxorubicin in myelogenous leukemia K562 cells by downregulating the mTOR/p70S6K pathway. Oncol Lett. 2019; 18(3):2694–2703. PMID:
31404320.

20. Lu QB, Wan MY, Wang PY, Zhang CX, Xu DY, Liao X, et al. Chicoric acid prevents PDGF-BB-induced VSMC dedifferentiation, proliferation and migration by suppressing ROS/NFκB/mTOR/P70S6K signaling cascade. Redox Biol. 2018; 14:656–668. PMID:
29175753.

21. Morita M, Gravel SP, Hulea L, Larsson O, Pollak M, St-Pierre J, et al. mTOR coordinates protein synthesis, mitochondrial activity and proliferation. Cell Cycle. 2015; 14(4):473–480. PMID:
25590164.

22. You G, Long X, Song F, Huang J, Tian M, Xiao Y, et al. Metformin activates the AMPK-mTOR pathway by modulating lncRNA TUG1 to induce autophagy and inhibit atherosclerosis. Drug Des Devel Ther. 2020; 14:457–468.
23. Wu H, Song A, Hu W, Dai M. The anti-atherosclerotic effect of paeonol against vascular smooth muscle cell proliferation by up-regulation of autophagy via the AMPK/mTOR signaling pathway. Front Pharmacol. 2018; 8:948. PMID:
29354055.

24. Zhao Y, Shang F, Shi W, Zhang J, Zhang J, Liu X, et al. Angiotensin II receptor type 1 antagonists modulate vascular smooth muscle cell proliferation and migration via AMPK/mTOR. Cardiology. 2019; 143(1):1–10. PMID:
31307032.

25. Jin Z, Tan Q, Sun B. Telmisartan ameliorates vascular endothelial dysfunction in coronary slow flow phenomenon (CSFP). Cell Biochem Funct. 2018; 36(1):18–26. PMID:
29314204.

26. Markan U, Pasupuleti S, Pollard CM, Perez A, Aukszi B, Lymperopoulos A. The place of ARBs in heart failure therapy: is aldosterone suppression the key? Ther Adv Cardiovasc Dis. 2019; 13:1753944719868134. PMID:
31401939.

27. Yusuf S, Teo K, Anderson C, Pogue J, Dyal L, Copland I, et al. Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomised controlled trial. Lancet. 2008; 372(9644):1174–1183. PMID:
18757085.
28. Diener HC. Preventing stroke: the PRoFESS, ONTARGET, and TRANSCEND trial programs. J Hypertens Suppl. 2009; 27(5):S31–6. PMID:
19587553.

29. Kliewer SA, Forman BM, Blumberg B, Ong ES, Borgmeyer U, Mangelsdorf DJ, et al. Differential expression and activation of a family of murine peroxisome proliferator-activated receptors. Proc Natl Acad Sci U S A. 1994; 91(15):7355–7359. PMID:
8041794.

30. Rosen ED, Spiegelman BM. PPARgamma: a nuclear regulator of metabolism, differentiation, and cell growth. J Biol Chem. 2001; 276(41):37731–37734. PMID:
11459852.
31. Zídek V, Mlejnek P, Simáková M, Silhavy J, Landa V, Kazdová L, et al. Tissue-specific peroxisome proliferator activated receptor gamma expression and metabolic effects of telmisartan. Am J Hypertens. 2013; 26(6):829–835. PMID:
23426788.
32. Auboeuf D, Rieusset J, Fajas L, Vallier P, Frering V, Riou JP, et al. Tissue distribution and quantification of the expression of mRNAs of peroxisome proliferator-activated receptors and liver X receptor-alpha in humans: no alteration in adipose tissue of obese and NIDDM patients. Diabetes. 1997; 46(8):1319–1327. PMID:
9231657.

33. Toba H, Wang J, Ohigashi M, Kobara M, Nakata T. Telmisartan protects against vascular dysfunction with peroxisome proliferator-activated receptor-γ activation in hypertensive 5/6 nephrectomized rats. Pharmacology. 2013; 92(5-6):265–275. PMID:
24281041.

34. Shiota A, Shimabukuro M, Fukuda D, Soeki T, Sato H, Uematsu E, et al. Activation of AMPK-Sirt1 pathway by telmisartan in white adipose tissue: a possible link to anti-metabolic effects. Eur J Pharmacol. 2012; 692(1-3):84–90. PMID:
22819702.





 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download