As of July 17, 2020, the Republic of Korea (Korea) had 13,672 confirmed cases of coronavirus disease 2019 (COVID-19) (26.4 per 100,000 population) and 293 COVID-19-related deaths (2.14%). The incidence of COVID-19 among children in Korea is 231 and 756 cases among those aged 0-9 and 10-19 years, respectively, while there has been no reported case of a child dying from COVID-19 in the country.1 Korea has classified COVID-19 as a “Class 1 infectious disease,”2 and confirmed people—regardless of the presence of symptoms or disease severity—are required to be hospitalized as mandated by the Infectious Disease Control and Prevention Act.3 Accordingly, those confirmed are sent to hospitals or residential treatment centers according to the severity of the disease.4
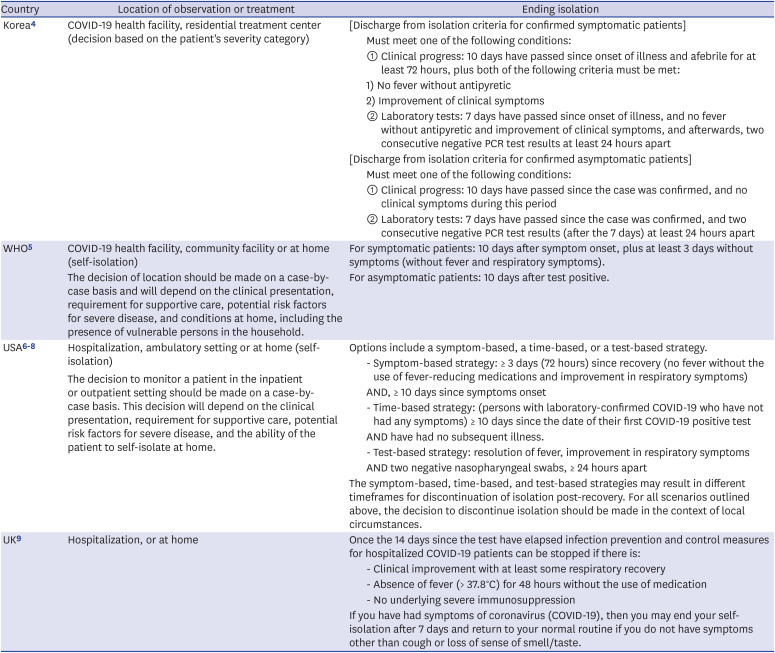
While such methods are being enforced for strict infection control at the national level in response to COVID-19, most countries—including the United States and many in Europe—allow people who are asymptomatic or those with mild symptoms be placed under self-isolation for at-home treatment (Table 1).56789 The policies in Korea do not allow infected people who are asymptomatic or those with mild symptoms to choose where he or she will be placed under isolation, which could raise human rights issues. Moreover, unnecessarily prolonging the length of a hospital stay until they satisfy the criteria for discharge from isolation could cause a relative decrease in the healthcare capacity for severe and critical patients. Therefore, reasonable allocation of hospital beds must be considered to reduce COVID-19-related mortality rate.
Isolation is considered an unavoidable measure for controlling infectious diseases, especially emerging infectious diseases. However, adverse psychological effects that entail such advantages of effective infection mitigation should not be neglected. According to a recent literature review, signs of post-traumatic stress symptoms, confusion and anger after isolation/quarantine were found in numerous studies, and such signs tended to become worse as the duration of isolation/quarantine increased.10 The disease control authorities in each country must put forth the effort to have clear indications for isolation and minimize the duration of isolation.
Furthermore, it is already known that a higher percentage of children confirmed with COVID-19 are asymptomatic or show mild symptoms, and the disease at their age tends to be less severe compared to adults.11 Children experience a growth stage when their personality is formed through relationships with others, and they have a high dependency on their parents. In particular, when a child below primary school age is placed in an isolation unit at a healthcare institution, it creates a situation of requiring an uninfected stressful adult guardian to be isolated together to take care of the child.12 It is also important to pay special attention to the psychological and emotional support for children and parents (or primary caregivers) who have to be separated from each other. To minimize these disadvantages in children, home isolation should be adopted as early treatment sites like many other countries.
Although the previous Korean isolation release criteria relied only upon PCR test results, the recently updated criteria, which references the World Health Organization guideline5 enabling a shorter isolation period, includes both symptom-based and test-based criteria. With respect to the recently updated Korean isolation release criteria,45 asymptomatic cases can be released from isolation if they 1) develop no clinical symptoms for 10 days after being confirmed, OR 2) receive two consecutive negative PCR test results taken at least 24 hours apart after 7 days since the date of their first COVID-19 positive test. Symptomatic cases can be released from isolation 1) after 10 days have passed since the onset of illness and are afebrile without antipyretics for at least 72 hours while showing improvement of clinical symptoms, OR 2) after 7 days have passed since the onset of illness and are afebrile without antipyretics while showing improvement of clinical symptoms, plus two consecutive negative PCR test results taken at least 24 hours apart (Table 1).
Meanwhile, epidemiological investigations and laboratory analyses on re-positive COVID-19 cases of people who test positive after recovery show no concrete evidence that they have infectivity.13 Rather, in these cases, more weight is given to the potential of SARS-CoV-2 viral RNA detection rather than SARS-CoV-2 with infectivity. Therefore, considering the recovery processes of respiratory viruses, avoiding policies that delay the return to society after isolation will help overcome the COVID-19 era. Furthermore, in asymptomatic people including children, using test-based strategies for discharge from isolation can cause unnecessarily long isolation periods that will eventually have negative impact on both individuals and the society.
Under the uncertain circumstances of when the COVID-19 pandemic will come to an end, people who are asymptomatic or those with mild symptoms need to be allowed to stay at home after evaluation. We therefore propose a change in the current policy that prioritizes isolation in healthcare institutions and residential treatment centers, to providing an isolation environment for pediatric patients to make a smooth recovery and emotionally/psychologically overcome the threatening COVID-19. To make this possible, the following things should be considered: a separated area for sleep and taking meals for the patient and guardian, the guardian must not be a high risk for COVID-19, and channels of communication that allow the patient's status to be communicated to a medical institution or to health authorities as needed. Telemedicine (telephone/video visits, etc.) and medical staff visits are key elements fundamental to the infrastructure of medical care support in the home isolation of children.
To summarize, the aggressive response to COVID-19 executed by the Korean disease control system has been effective in managing the situation so far. However, after several months of experience in combating COVID-19, it is necessary to make efforts to further reduce the isolation period based on scientific research data that is continuously being updated—taking into consideration disease severity, human rights, and normalization of individuals and society. We suggest that hospitalization should not initially be required in people who are asymptomatic or those with mild clinical presentations and believe that many patients will be able to manage their illness at home under close medical observation.
References
1. Korea Centers for Disease Control and Prevention. Coronavirus disease-19, Republic of Korea as of July 17, 2020. Updated 2020. Accessed July 17, 2020. http://ncov.mohw.go.kr/en/.
2. Infectious Disease Control and Prevention Act. No. 16101, Article 41. 2018. 12. 31.
3. Infectious Disease Control and Prevention Act. No. 16101, Article 2. 2018. 12. 31.
4. Korea Centers for Disease Control and Prevention. Response guidelines against COVID-19. 9th ed. Updated 2020. Accessed July 15, 2020. http://ncov.mohw.go.kr/duBoardList.do?brdId=2&brdGubun=24.
5. World Health Organization. Clinical management of COVID-19: interim guidance. Updated 2020. Accessed June 5, 2020. https://apps.who.int/iris/handle/10665/332196.
6. Center for Disease Control and Prevention. Discontinuation of isolation for persons with COVID-19 not in healthcare settings: interim guidance. Updated 2020. Accessed June 5, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-in-home-patients.html.
7. Center for Disease Control and Prevention. Discontinuation of transmission-based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance). Updated May 2, 2020. Accessed June 5, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html.
8. Center for Disease Control and Prevention. Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19). Updated 2020. Accessed June 5, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html.
9. Public Health England. Stay at home: guidance for households with possible or confirmed coronavirus (COVID-19) infection. Updated 2020. Accessed June 17, 2020. https://www.gov.uk/government/publications/covid-19-stay-at-home-guidance/stay-at-home-guidance-for-households-with-possible-coronavirus-covid-19-infection#ending-isolation.
10. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395(10227):912–920. PMID: 32112714.

11. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020; 145(6):e20200702. PMID: 32179660.

12. Kim H, Park KJ, Shin YW, Lee JS, Chung S, Lee T, et al. Psychological impact of quarantine on caregivers at a children’s hospital for contact with case of COVID-19. J Korean Med Sci. 2020; 35(28):e255. PMID: 32686372.

13. Korean Center for Disease Control and Prevention. Findings from investigation and analysis of re-positive cases. Updated 2020. Accessed June 15, 2020. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030.
Table 1
Location of observation or treatment and ending isolation criteria for confirmed COVID-19 cases in different countries
| Country | Location of observation or treatment | Ending isolation | ||
|---|---|---|---|---|
| Korea4 | COVID-19 health facility, residential treatment center (decision based on the patient's severity category) | [Discharge from isolation criteria for confirmed symptomatic patients] | ||
| Must meet one of the following conditions: | ||||
| 1) Clinical progress: 10 days have passed since onset of illness and afebrile for at least 72 hours, plus both of the following criteria must be met: | ||||
| ① No fever without antipyretic | ||||
| ② Improvement of clinical symptoms | ||||
| 2) Laboratory tests: 7 days have passed since onset of illness, and no fever without antipyretic and improvement of clinical symptoms, and afterwards, two consecutive negative PCR test results at least 24 hours apart | ||||
| [Discharge from isolation criteria for confirmed asymptomatic patients] | ||||
| Must meet one of the following conditions: | ||||
| 1) Clinical progress: 10 days have passed since the case was confirmed, and no clinical symptoms during this period | ||||
| 2) Laboratory tests: 7 days have passed since the case was confirmed, and two consecutive negative PCR test results (after the 7 days) at least 24 hours apart | ||||
| WHO5 | COVID-19 health facility, community facility or at home (self-isolation) | For symptomatic patients: 10 days after symptom onset, plus at least 3 days without symptoms (without fever and respiratory symptoms). | ||
| The decision of location should be made on a case-by-case basis and will depend on the clinical presentation, requirement for supportive care, potential risk factors for severe disease, and conditions at home, including the presence of vulnerable persons in the household. | For asymptomatic patients: 10 days after test positive. | |||
| USA678 | Hospitalization, ambulatory setting or at home (self-isolation) | Options include a symptom-based, a time-based, or a test-based strategy. | ||
| The decision to monitor a patient in the inpatient or outpatient setting should be made on a case-by-case basis. This decision will depend on the clinical presentation, requirement for supportive care, potential risk factors for severe disease, and the ability of the patient to self-isolate at home. | - Symptom-based strategy: ≥ 3 days (72 hours) since recovery (no fever without the use of fever-reducing medications and improvement in respiratory symptoms) | |||
| AND, ≥ 10 days since symptoms onset | ||||
| - Time-based strategy: (persons with laboratory-confirmed COVID-19 who have not had any symptoms) ≥ 10 days since the date of their first COVID-19 positive test | ||||
| AND have had no subsequent illness. | ||||
| - Test-based strategy: resolution of fever, improvement in respiratory symptoms | ||||
| AND two negative nasopharyngeal swabs, ≥ 24 hours apart | ||||
| The symptom-based, time-based, and test-based strategies may result in different timeframes for discontinuation of isolation post-recovery. For all scenarios outlined above, the decision to discontinue isolation should be made in the context of local circumstances. | ||||
| UK9 | Hospitalization, or at home | Once the 14 days since the test have elapsed infection prevention and control measures for hospitalized COVID-19 patients can be stopped if there is: | ||
| - Clinical improvement with at least some respiratory recovery | ||||
| - Absence of fever (> 37.8°C) for 48 hours without the use of medication | ||||
| - No underlying severe immunosuppression | ||||
| If you have had symptoms of coronavirus (COVID-19), then you may end your self-isolation after 7 days and return to your normal routine if you do not have symptoms other than cough or loss of sense of smell/taste. | ||||




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download