INTRODUCTION
Neurosyphilis is the most common and severe manifestation of syphilis. It is caused by
Treponema pallidum subspecies pallidum, which can affect the central nervous system (CNS) during any stage of the disease. As ‘general paresis of the insane,’ which is a later symptomatic form of neurosyphilis, it involves neuropsychiatric deficits such as delusion, hallucination, and disorientation, and can mimic a variety of psychiatric disorders such as psychosis, mania, delirium, personality changes, and dementia.
123 Neurosyphilis was an important concern in psychiatric wards before and after the 1900s, because 20%–30% of psychiatric inpatients at the time had neurosyphilis. With the advent of penicillin, the prevalence of neurosyphilis has decreased to less than 2% since the 1950s.
4 Although neurosyphilis is now uncommon and has not attracted much interest among young clinicians, there has been a resurgence of syphilis in countries with limited medical resources.
5 In Korea, the most recent case of neurosyphilis was reported in 2018 and a case of general paresis in neurosyphilis was last reported in 2017.
67 Population mobility, such as immigration and refugee crises, is increasingly influencing the globalization of disease.
8 The foreign population in Korea, including migrant workers, has been growing rapidly, increasing from 1.3 million in 2012 to 2.36 million in 2018, accounting for 4.8% of the total population of Korea. Foreign residents from countries with limited medical resources represent the fastest-growing population in Korea.
9 With these changes, infectious diseases of the immigrant population are important issues for the health of both Korean nationals and foreigners living in Korea.
10 Concerns have emerged regarding the recent surge in numbers of people diagnosed with syphilis in Korea.
11 This case report of general paresis is intended to raise awareness of re-emerging neurosyphilis in Korea as a possible etiology of psychotic disorders.
CASE DESCRIPTION
A 68-year-old Korean-Chinese man from Yanbian Korean Autonomous Prefecture in China visited the Emergency Department of Jeju National University Hospital in 2019. He had exhibited mania-like symptoms, including talkativeness, buying sprees, and high impulsivity, commencing 1.5 years prior to presentation. One year previously, symptoms had appeared since that time including cognitive fluctuation, and disorientation with regard to time and place. From 3 months prior to presentation, he had exhibited out-of-the-ordinary behavior, including becoming angry easily when talking to his family and making sexual jokes to his niece. He had talked to himself as if having a conversation with another person. From 1 week prior to presentation, he had said things like, “Chinese police will shoot me dead,” “I saw a policeman in the car out there,” and he was acting terrified. In the emergency department, he exhibited disorientation with regard to time and place. He was very agitated because he believed that the Chinese police was chasing him and continually attempted to leave the emergency room; he was hospitalized in a psychiatric ward for further evaluation and treatment.
On mental status examination on day 1 after admission, pleomorphic psychiatric symptoms were observed. He exhibited the characteristic psychopathology of delirium, including inattention, disorientation with regard to time and place, and the characteristic psychopathology of psychosis, including auditory hallucination, soliloquy, and persecutory delusion. Various symptoms of mania, such as flight of ideas, pressure of speech, and violent behavior, were also observed. Mini-mental state examination (MMSE) could not be performed because he was not cooperative. Physical examination revealed no lesions suggesting syphilis, such as chancre or skin rash. Neurological examination revealed no signs suggestive of neurosyphilis, such as Argyll Robertson pupils, hyperreflexia, or sensory changes.
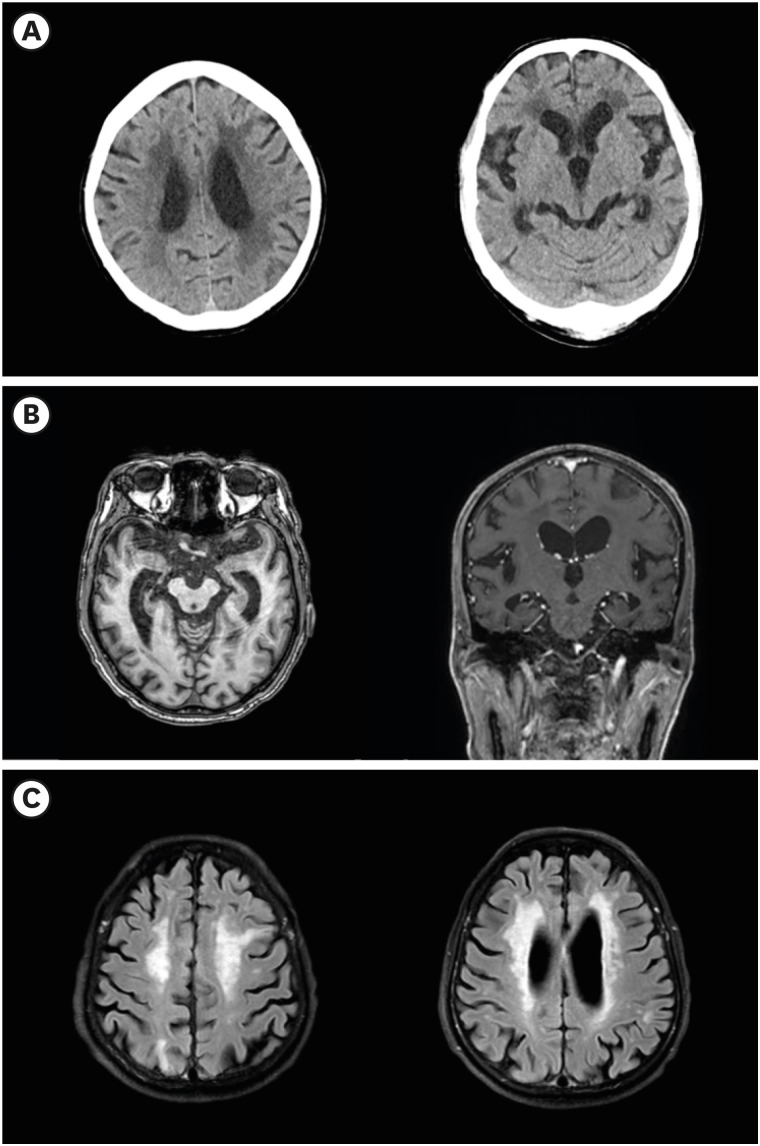
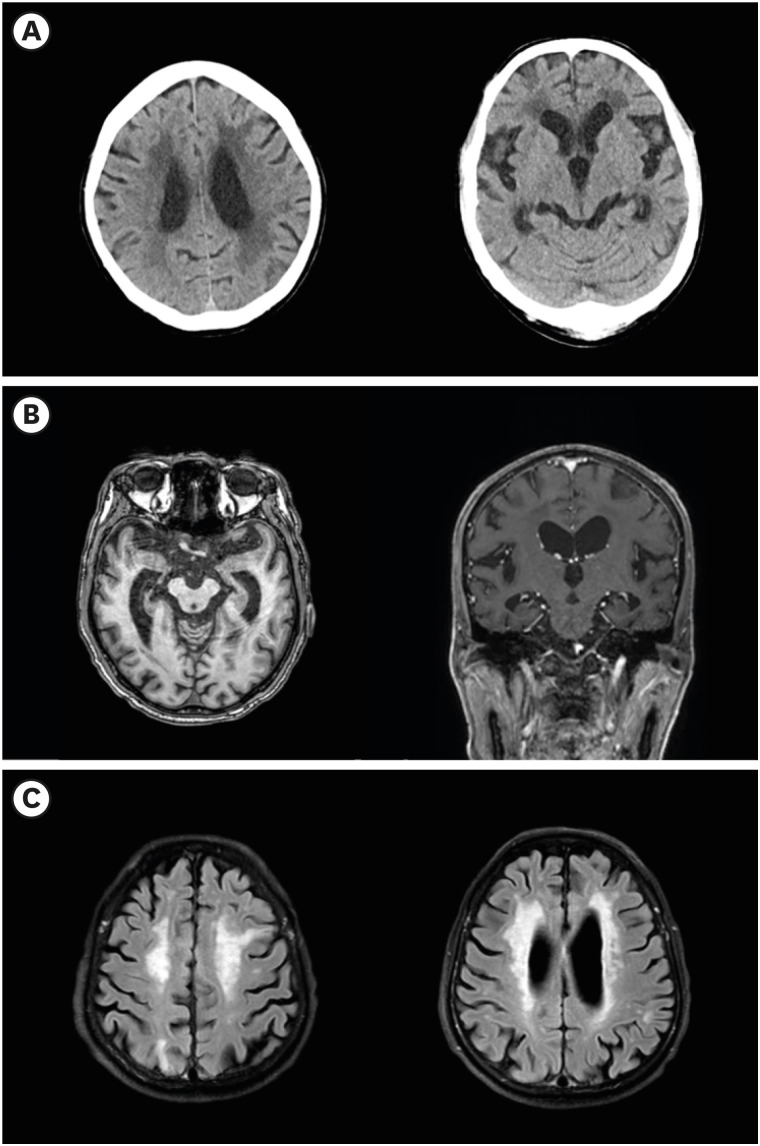
On day 1 after admission, serum rapid plasma reagin (RPR) test revealed that the patient's RPR level was elevated to 148.4 units. Brain atrophy and leukoaraiosis were detected on brain computed tomography (
Fig. 1). Additional serum treponemal tests were administered on the 2nd day and the results were reported on the 6th day. Fluorescent treponemal antibody absorption (FTA-ABS) test indicated positivity for FTA-ABS IgG and weak positivity for FTA-ABS IgM.
T. pallidum hemagglutination assay (TPHA) was reactive at 298.48 units. Positive serum treponemal-specific test confirmed a diagnosis of late latent syphilis. On the 6th day, diffuse brain atrophy, old ischemic lesions in the left frontal and right parietal subcortices, and periventricular hyperintensities with grade 3 on modified Fazekas's scale
12 were observed on brain magnetic resonance imaging (MRI) (
Fig. 1). On the 7th day, analysis of cerebrospinal fluid (CSF) through lumbar puncture revealed a positive Venereal Disease Research Laboratory (VDRL) test result at a titer of 1:1, with no increases in white blood cell (WBC) count (1/μL) or total protein level (45 mg/dL). The positive VDRL result in the CSF confirmed the diagnosis of neurosyphilis.
Fig. 1
Brain computed tomography and brain magnetic resonance imaging of the patient. (A) Non-enhanced computed tomography axial view. (B) T1-weighted axial and sagittal images. (C) T2-weighted fluid attenuated inversion recovery axial images. Published under agreement of the patient's guardian.
On the 1st day after admission, the atypical antipsychotic drug olanzapine was administered at a dose of 5 mg/day for alleviation of psychotic symptoms, manic symptoms, and behavioral problems, and the atypical antipsychotic drug quetiapine was administered at a dose of 50 mg/day for sleep at night. From day 1 to 20, olanzapine and quetiapine doses were increased to 15 mg/day and 150 mg/day, respectively.
From the 6th day after admission, the patient was administered intramuscular penicillin G benzathine at a dose of 2.4 million units once a week for 3 weeks. Aqueous crystalline penicillin G was not being produced in Korea, so until we obtained this medication the patient was administered intravenous ceftriaxone at a dose of 2 g once daily for 9 days, doxycycline at 100 mg orally twice daily for 8 days, and azithromycin at a dose of 2 g orally once daily for 2 days from the 7th day after admission. On the 15th day after admission, we obtained aqueous crystalline penicillin G from the Korea Orphan and Essential Drug Center and the patient was administered intravenous penicillin G, 4 million units every 4 hours, for 14 days.
From day 21, disorientation improved and the patient was relatively cooperative to interview. His MMSE score was 16, but psychotic symptoms remained. Olanzapine dose was increased to 30 mg/day. On day 28, his manic symptoms and behavioral problems were markedly alleviated, but his psychotic symptoms were only slightly alleviated. On day 35, the serum RPR test was performed again, and his RPR level was still elevated to 146.8 units. On day 36, neurocognitive test battery was administered. The MMSE score was 7 and the Clinical Dementia Rating score was 2. On day 40, analysis of CSF by lumbar puncture still revealed a positive VDRL result at a titer of 1:1 and no increases in WBC count (1/μL) or total protein level (37 mg/dL). By the time of discharge on day 42, the patient's manic symptoms and violent behavior had disappeared but psychotic symptoms, such as intermittent soliloquy, remained.
Ethics statement
The images are published under agreement of the patient's legal guardian.
DISCUSSION
The most common presentations of neurosyphilis include general paresis, tabes dorsalis, and meningovascular neurosyphilis. The late stage of neurosyphilis involves parenchymal effects in the brain leading to severe neuropsychiatric symptoms. In the present case, the patient was considered to have general paresis. General paresis, also known as general paralysis of the insane or paralytic dementia, can occur at any time from 3–30 years after infection, usually peaking 25 years after initial exposure. Symptoms of general paresis include neuropsychiatric deficits, such as personality changes, delusions and hallucination, and neurological deficits, such as Argyll Robertson pupils, hyperreflexia, and sensory changes. These symptoms are considered to be caused by progressive frontotemporal meningoencephalitis with diffuse cortical atrophy.
2
Fig. 1 presents various radiological findings. Diffuse brain atrophy, temporal horn widening, and hippocampal atrophy were observed on T1-weighted axial and sagittal images. Old ischemic lesions in the left frontal and right parietal subcortices, and periventricular hyperintensities classified as grade 3 on modified Fazekas's scale
12, were found on T2-weighted fluid-attenuated inversion recovery axial images.
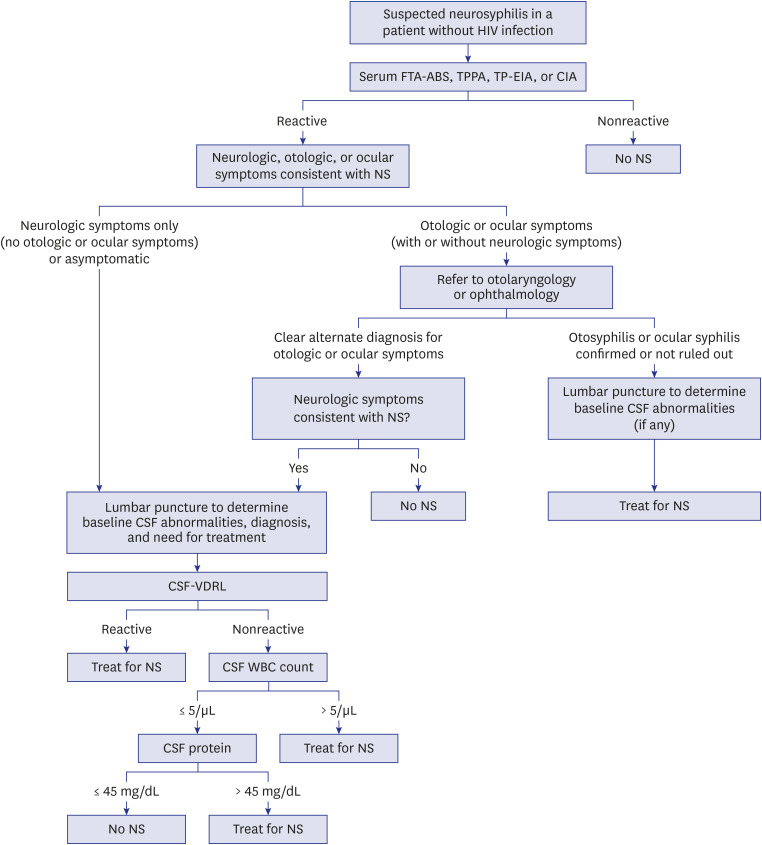
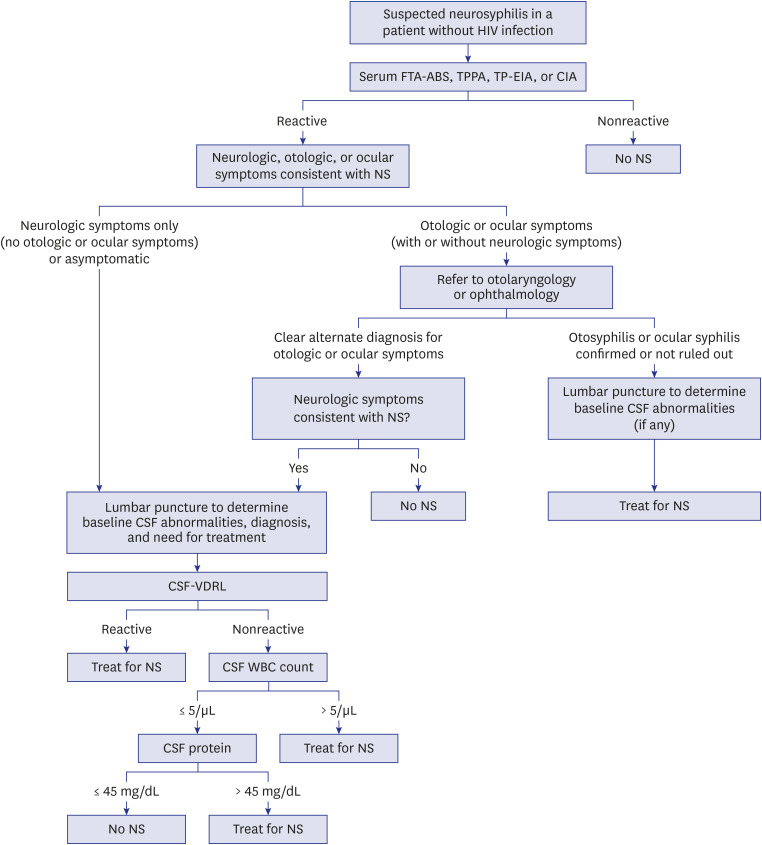
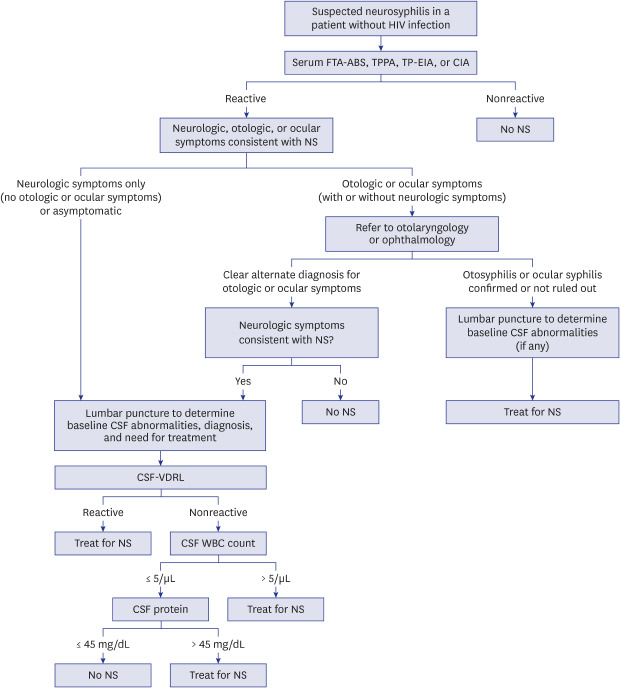
The US Centers for Disease Control and Prevention (CDC) recommends the following diagnostic methods for neurosyphilis, as shown in
Fig. 2.
1314 To diagnose neurosyphilis, infection with
T. pallidum must first be confirmed. A simple serum test for syphilis consists of serum non-treponemal tests and serum treponemal tests. Serum non-treponemal tests consist of VDRL testing and RPR testing. These tests can be nonreactive in patients with syphilis. Serum treponemal tests consist of FTA-ABS test,
T. pallidum particle agglutination assay (TPPA), and syphilis enzyme immunoassays. To diagnose syphilis, serum treponemal tests should always be performed because these tests remain reactive throughout life, regardless of prior treatment. CSF examination could be administered for known syphilis patients with neurological, ophthalmic, and neuropsychiatric deficits. The representative pathological CSF parameters are elevations of CSF WBC count > 5/μL or CSF total protein concentration > 45 mg/dL. Pathological CSF parameters include TPPA, TPHA, and VDRL test titer. Identification of CSF abnormalities is important to assess the activity of neurosyphilis for use in therapeutic decision-making and helping to assess the efficacy of treatment. Serum and CSF tests must be interpreted in relation to each other and to clinical findings and brain imaging.
1
Fig. 2
Algorithm of diagnosis of neurosyphilis in a patient without HIV infection. Adapted from Marra CM. UpToDate.14
HIV = human immunodeficiency virus, FTA-ABS = fluorescent treponemal antibody absorption test, TPPA = Treponema pallidum particle agglutination assay, TP-EIA = Treponema pallidum enzyme immunoassays, CIA = chemiluminescence immunoassays, NS = neurosyphilis, CSF = cerebrospinal fluid, VDRL = venereal disease research laboratory test, WBC = white blood cell.
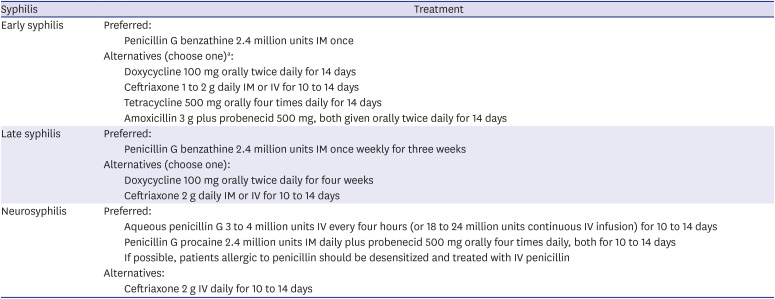
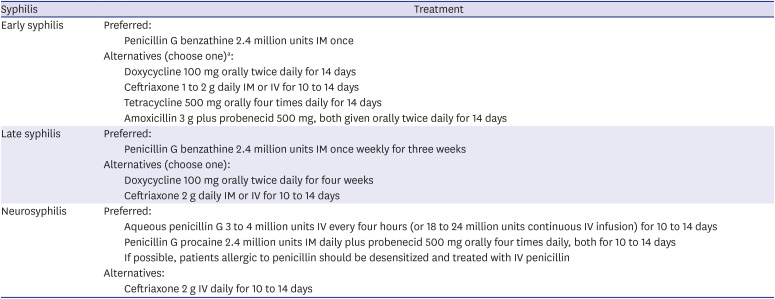
To treat neurosyphilis, the 2015 CDC guidelines
13 recommend administration of aqueous penicillin G by intravenous (iv) infusion every 4 hours at a dose of 3–4 million units per day for 10–14 days (
Table 1). Recommendations for treatment are based on clinical experience and on predicted penetration of penicillin into the CNS. Success of neurosyphilis treatment is judged by resolution or stabilization of clinical abnormalities and normalization of CSF abnormalities. To determine the necessity of retreatment, CSF-WBC and CSF-VDRL could be the most reliable parameters. Neurological examination and lumbar puncture should be performed every 6 months until the CSF-WBC count is normal and CSF-VDRL is nonreactive after treatment. Retreatment was suggested in cases in which the CSF-WBC count fails to decrease within 6 months after therapy or CSF-VDRL fails to decrease by fourfold within 1 year after therapy. If the initial titer is < 1:2, retreatment is suggested in cases with failure of achieve CSF-VDRL nonreactivity.
15 No well-controlled clinical data are available regarding type, optimal dosage, duration, or long-term efficacy of antibiotic therapy in the treatment of late-stage neurosyphilis. Normalization of specific serological reactions in serum and CSF after treatment can be delayed or even fail to appear. It is difficult to make a decision of when to retreat based on laboratory findings during the follow-up period. Treatment and monitoring of late-stage neurosyphilis are still challenging.
1
Table 1
Treatment of syphilis
|
Syphilis |
Treatment |
|
Early syphilis |
Preferred: |
|
Penicillin G benzathine 2.4 million units IM once |
|
Alternatives (choose one)a: |
|
Doxycycline 100 mg orally twice daily for 14 days |
|
Ceftriaxone 1 to 2 g daily IM or IV for 10 to 14 days |
|
Tetracycline 500 mg orally four times daily for 14 days |
|
Amoxicillin 3 g plus probenecid 500 mg, both given orally twice daily for 14 days |
|
Late syphilis |
Preferred: |
|
Penicillin G benzathine 2.4 million units IM once weekly for three weeks |
|
Alternatives (choose one): |
|
Doxycycline 100 mg orally twice daily for four weeks |
|
Ceftriaxone 2 g daily IM or IV for 10 to 14 days |
|
Neurosyphilis |
Preferred: |
|
Aqueous penicillin G 3 to 4 million units IV every four hours (or 18 to 24 million units continuous IV infusion) for 10 to 14 days |
|
Penicillin G procaine 2.4 million units IM daily plus probenecid 500 mg orally four times daily, both for 10 to 14 days |
|
If possible, patients allergic to penicillin should be desensitized and treated with IV penicillin |
|
Alternatives: |
|
Ceftriaxone 2 g IV daily for 10 to 14 days |
Although the prevalence of syphilis decreased dramatically after the widespread application of antibiotics, since the 1960s syphilis has been increasing again in the US as well as in Korea.
4 Cases of primary and secondary syphilis have increased in the US every year since 2000, with 9.5 cases per 100,000 persons in 2017, and the number of cases of late and late latent syphilis has increased by 17.2% yearly.
25 Rates of neurosyphilis in various series have been estimated at 0.47–2.1 cases per 100,000 in the population. In Korea, the cases of meningovascular syphilis in 2009,
16 neurosyphilis with mesiotemporal abnormalities in 2009
17 and neurosyphilis with cerebral gumma in 2009
18 and 2013
19 were reported. Recently, the cases of general paresis and neurosyphilis was also reported in 2017 and 2018.
67 However, the diagnosis of neurosyphilis with psychotic features tends to be overlooked in Korea.
Immigration plays an important role in the epidemiology of syphilis. Immigration-receiving nations such as the US, Canada, and Australia, where admissibility can be affected by health criteria, have routinely administered syphilis screening tests for several decades. A 2007 study of immigrants to Canada reported that the largest numbers of syphilis cases were found in immigration applicants from the Asia–Pacific region (803 cases of 2,208 with a known source region; 36.4%).
8 In a 2009–2013 study of refugees bound for the US, the second-highest overall age-adjusted prevalence rates of syphilis seropositivity were observed among refugees from East Asia and the Pacific region (397 cases per 100,000). Refugees may be at increased risk of sexually transmitted infection (STI) due to various factors such as poverty, sexually related violence, abuse, and exploitation. Additionally, refugees tend to come from countries with high prevalence rates of STIs and often live in areas where access to preventive services and healthcare may be inadequate.
20
Syphilis has reappeared in countries with limited medical resources and in certain populations within developed countries.
5 As of 2018, the number of foreign nationals in Korea had increased to 2.05 million, or 4.0% of the total population. More than half of the foreign nationals in Korea are Korean-Chinese, Chinese, or Vietnamese.
9 By 2000, the number of North Korean defectors in South Korea had increased to about 2,500 per year, and by 2019 this rate remained at more than 1,000 per year.
21 Population mobility has increasingly affected the globalization of disease, and the importation of syphilis through the process of migration may be significantly influencing the increasing numbers of syphilis cases in Korea.
This case report had several limitations. First, history was collected from the patient himself. As the cognitive function of our patient had already declined and his family did not know about his pre-marital personal history, it was not possible to determine the details of his personal history, such as preexisting psychiatric disorders, multiple sexual partners, etc. Second, the chronic infarcts in his left frontal and parietal subcortices were assumed to be related to previous inflammation from parenchymal infection of neurosyphilis. However, the latest brain MRI revealed no abnormal enhancements within the brain suggesting current cerebritis. Third, more detailed CSF profile such as IgG index and oligoclonal bands were not examined in this case. Although oligoclonal banding is not a satisfactory test for neurosyphilis and the CSF IgG index appears to help in only ruling out infection,
22 those CSF examinations can be used as biological monitors of clinical improvement, especially in meningeal and vascular neurosyphilis.
23
In conclusion, syphilis is still present and neurosyphilis should also be included as a possible etiology of psychotic disorders in Korea. At the initial evaluation, syphilis screening serum tests are recommended for psychotic patients, especially those with pleomorphic symptoms and cognitive dysfunction.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download